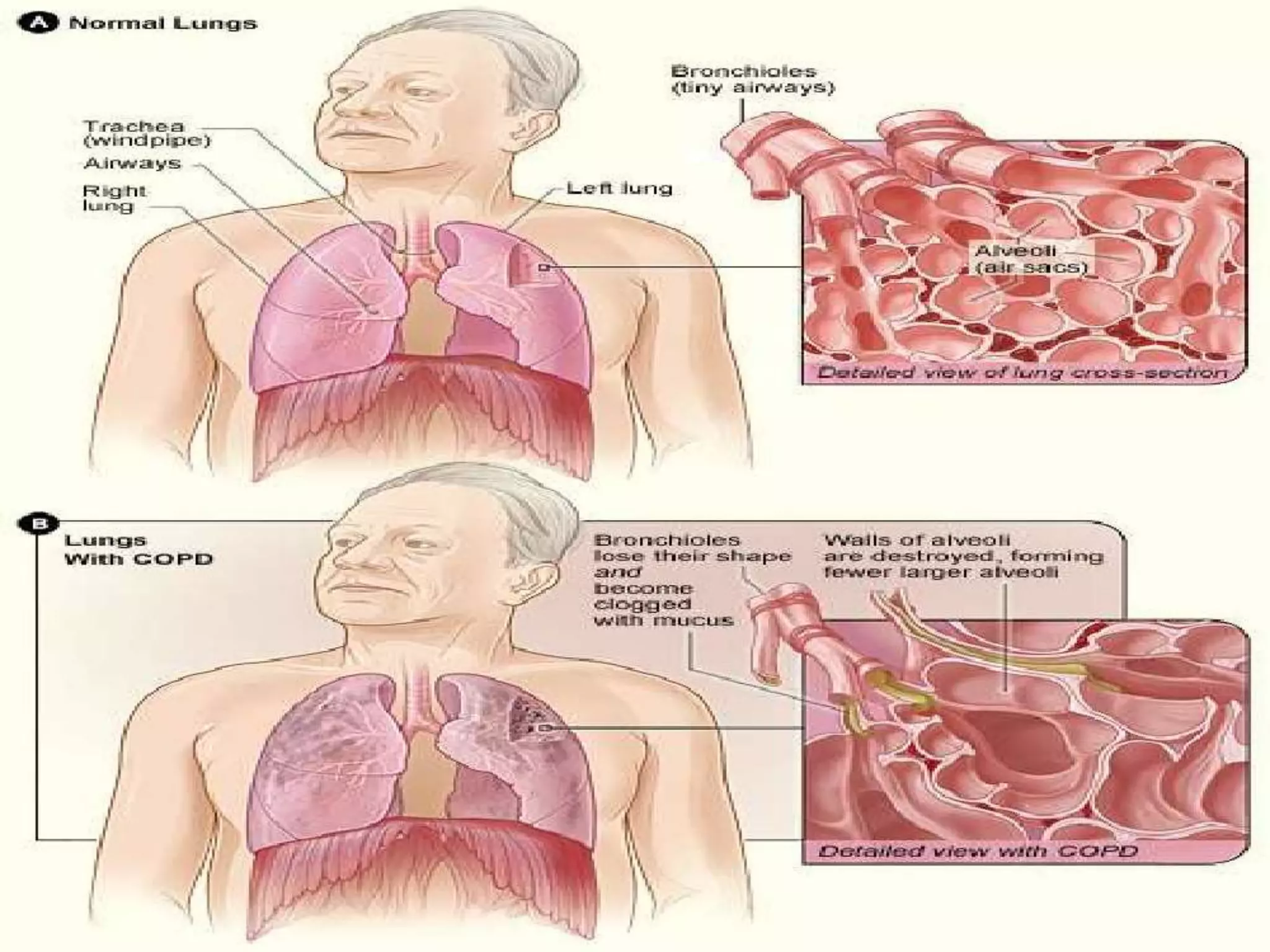
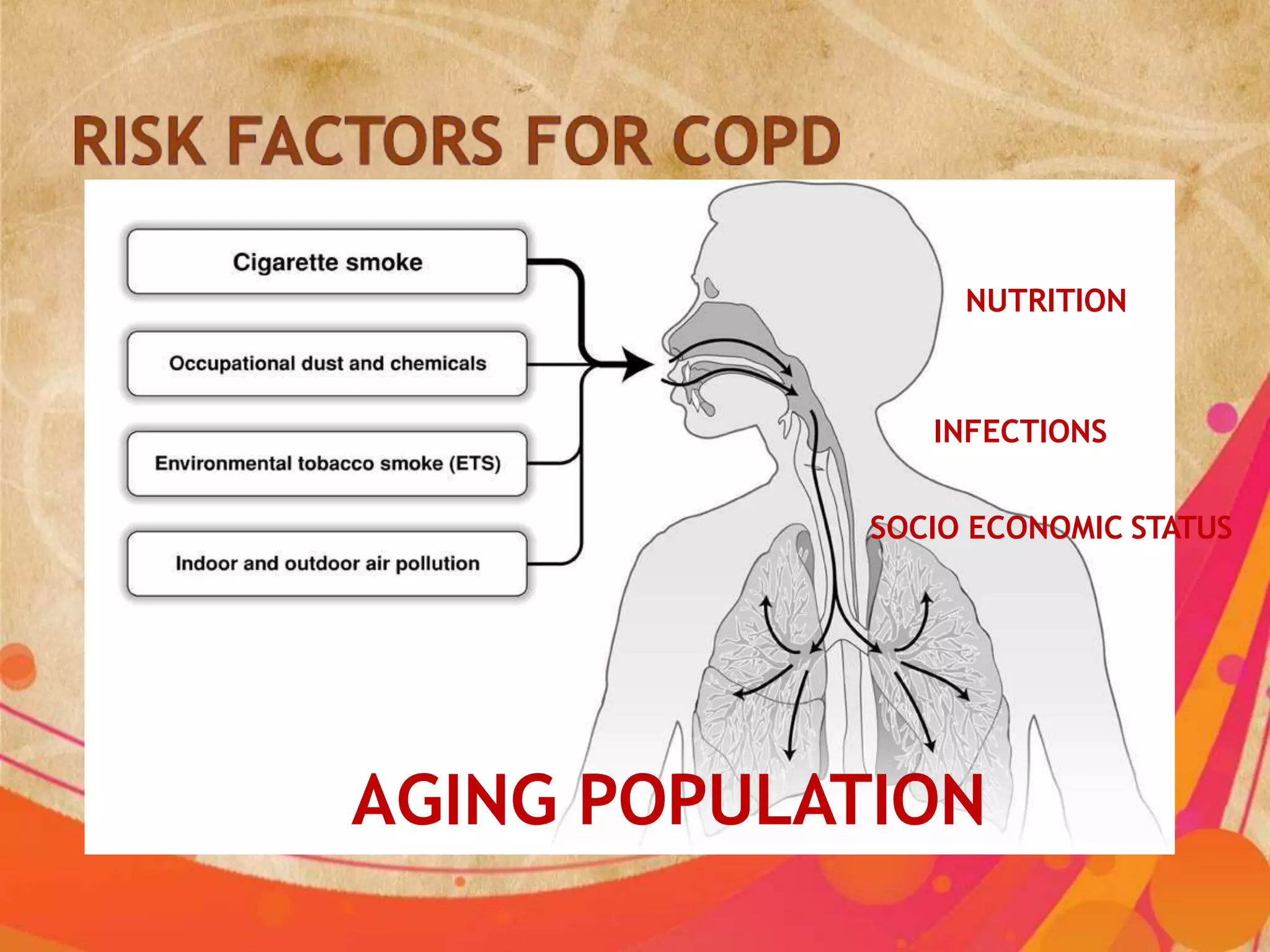
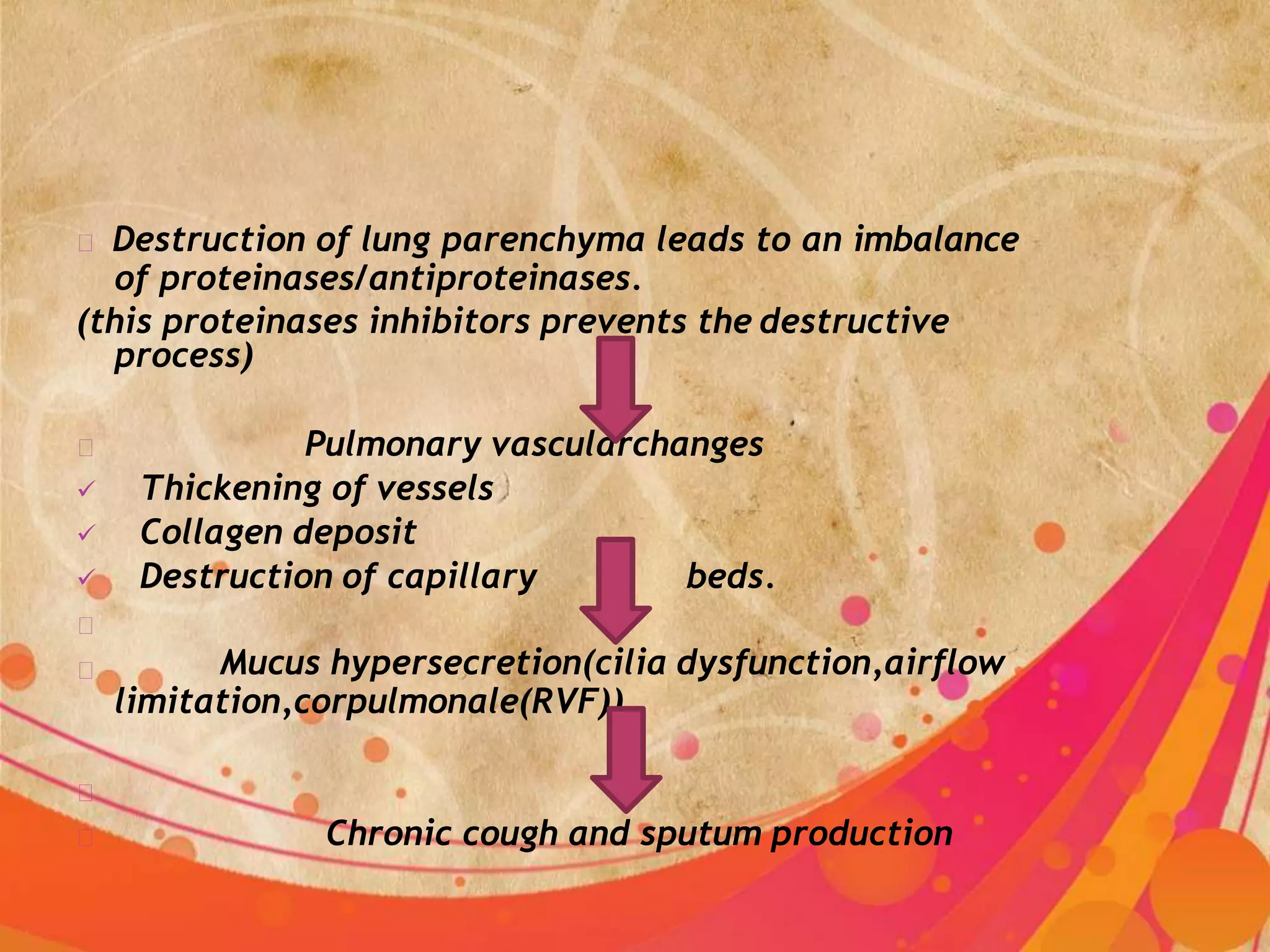
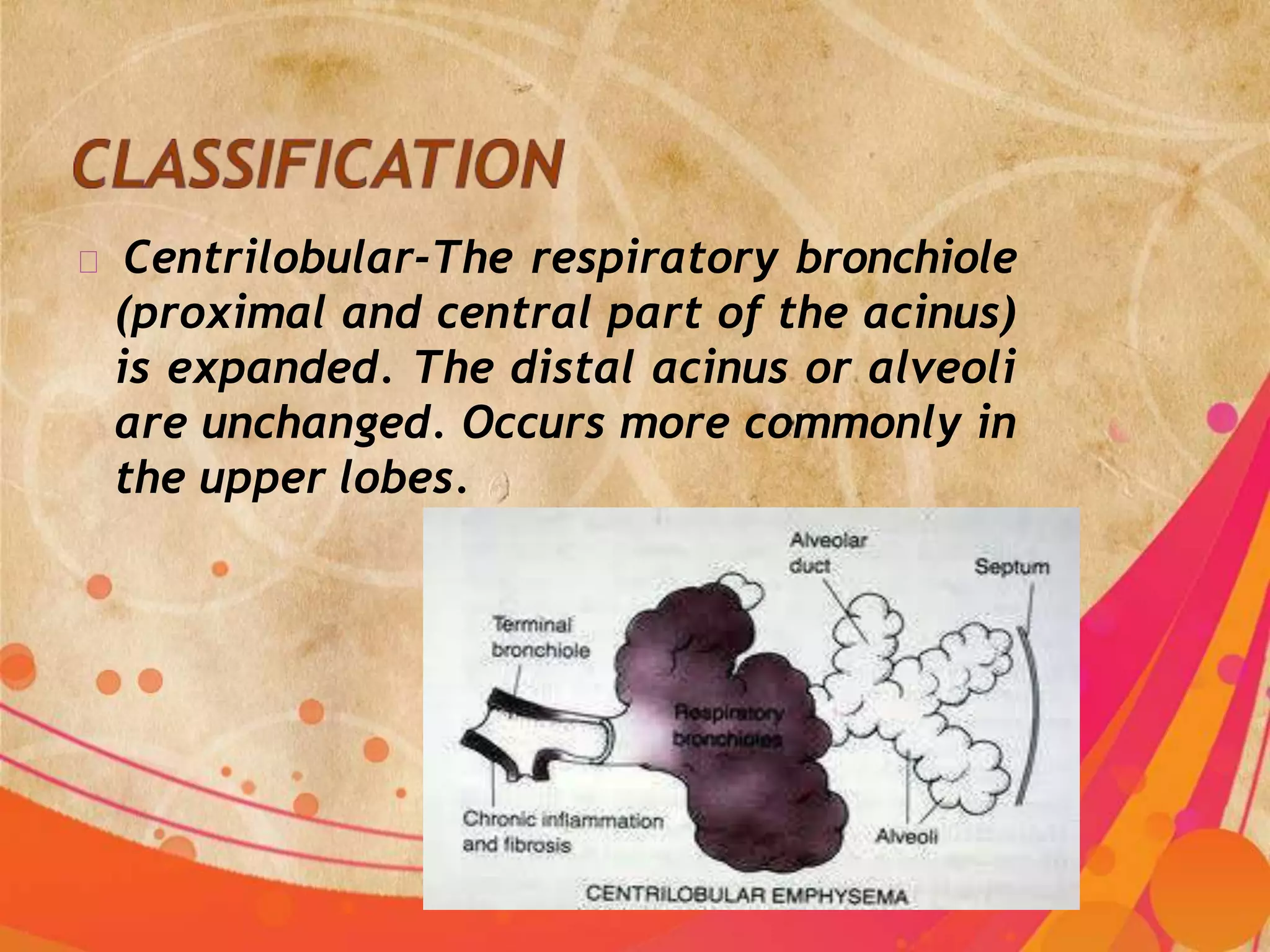
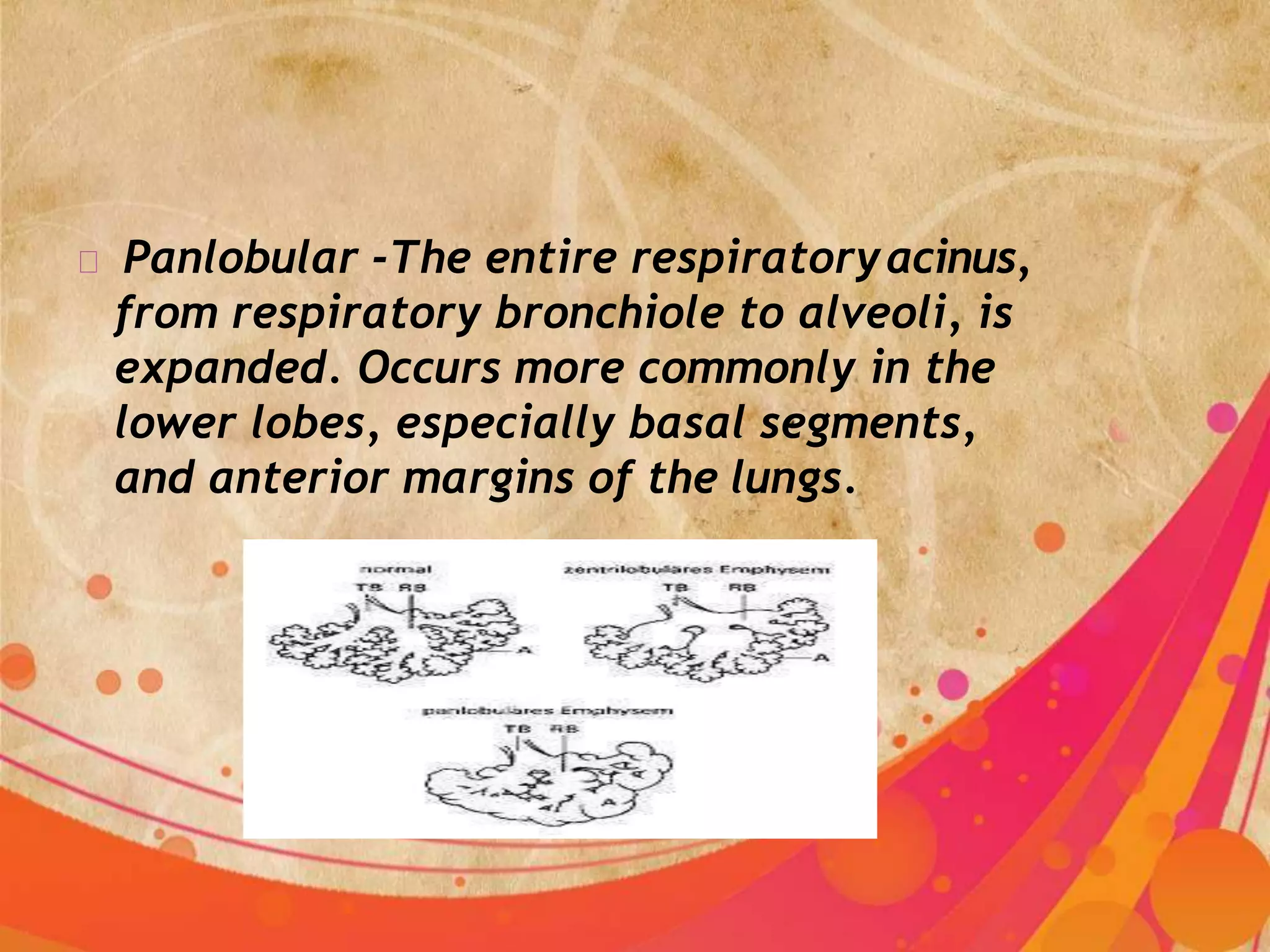
COPD refers to chronic bronchitis and emphysema, two commonly co-existing lung diseases where the airways become narrowed leading to limited airflow. The main causes are smoking, occupational exposures, air pollution, and genetic conditions. Symptoms include chronic cough, sputum production, wheezing, chest tightness, and shortness of breath. Management includes bronchodilators, corticosteroids, oxygen therapy, promoting exercise, and controlling complications to improve lung function and general health.