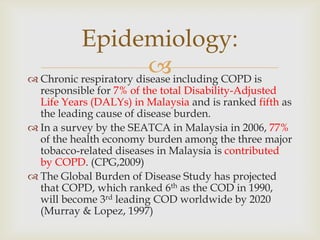
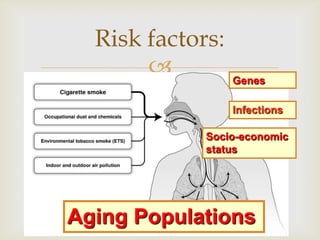
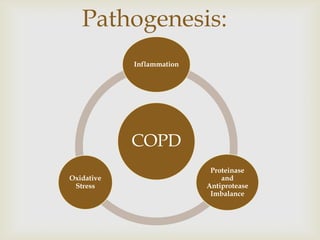
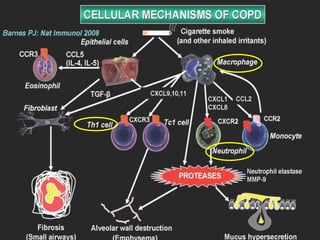
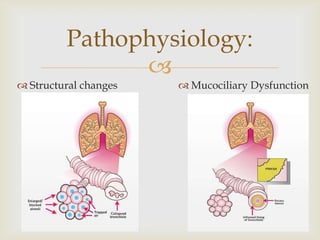
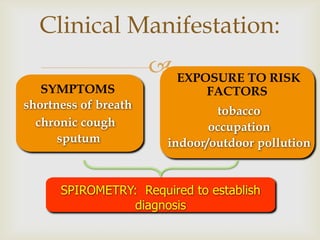
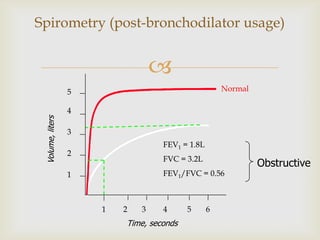
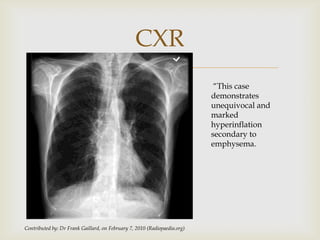
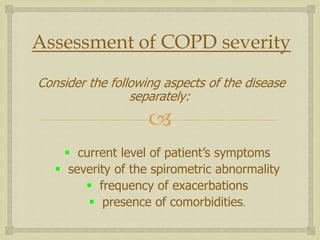
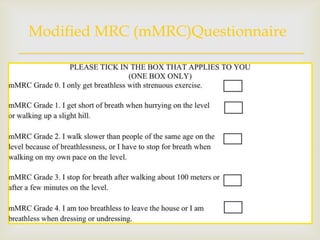
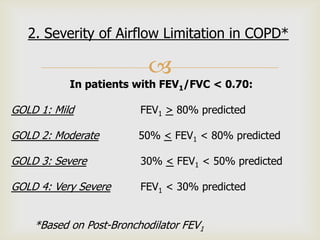
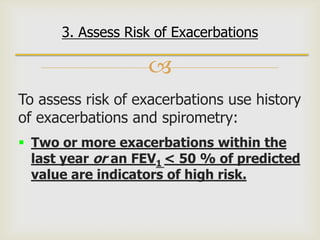
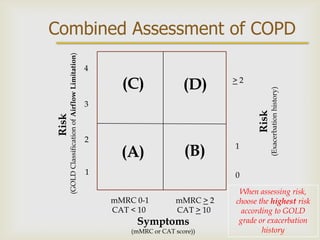
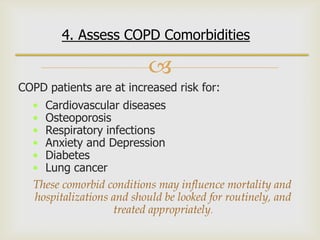
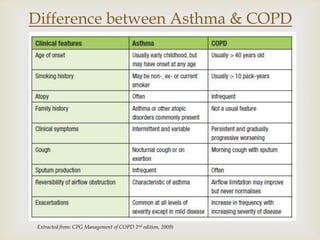
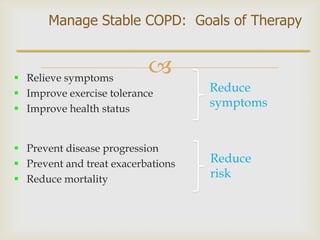
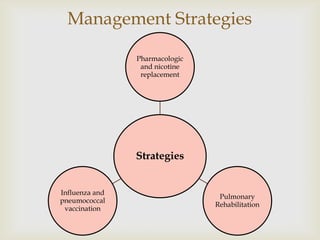
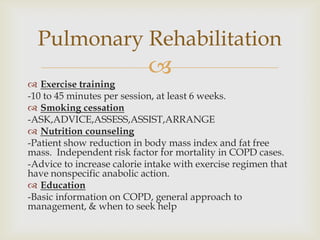
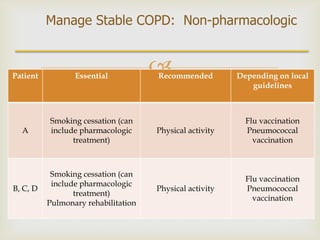
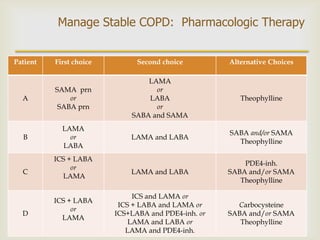
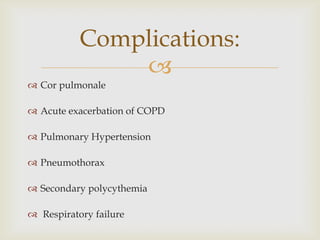
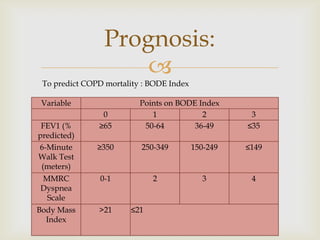
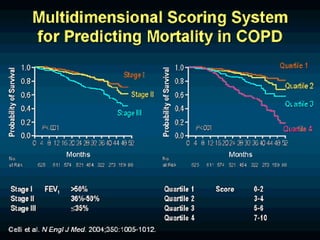
COPD is a common preventable disease characterized by persistent airflow limitation that is usually progressive. It is caused by exposure to noxious particles or gases, most commonly from cigarette smoking. COPD places a significant disease burden and is projected to become the third leading cause of death worldwide by 2020. The diagnosis is established through spirometry showing airflow obstruction that is not fully reversible. Disease severity is assessed based on symptoms, degree of airflow limitation, exacerbation frequency, and comorbidities. Treatment involves smoking cessation, pulmonary rehabilitation, pharmacotherapy including bronchodilators and inhaled corticosteroids, and management of exacerbations and complications. Prognosis can be estimated using the BODE index.