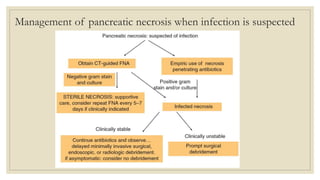
Mr. T, a 56-year-old man, presented with acute pancreatitis symptoms including epigastric pain and nausea. Investigations confirmed elevated pancreatic enzymes. He was initially treated conservatively but his condition deteriorated, requiring ICU admission and intubation. Imaging showed acute pancreatitis with peripancreatic fluid collection. Antibiotics were started after he developed a fever. Complications of acute pancreatitis like pancreatic necrosis and pseudocyst formation were discussed. The role of antibiotics, ERCP, and surgical or radiologic drainage of infected collections was also outlined.