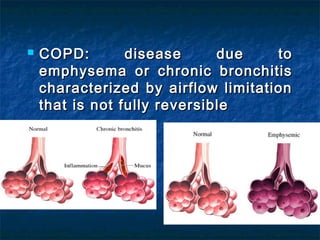
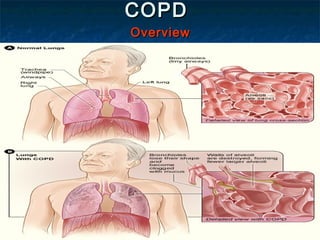
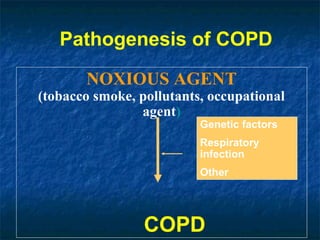
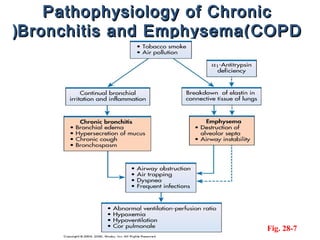
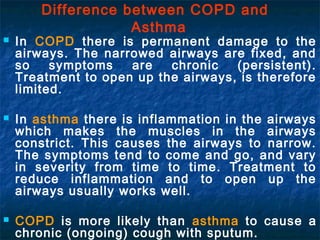
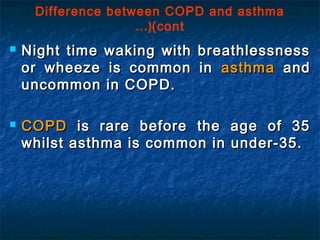
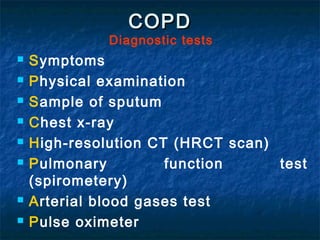
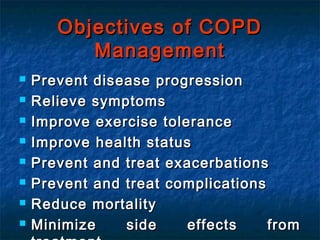
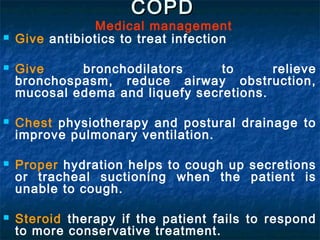
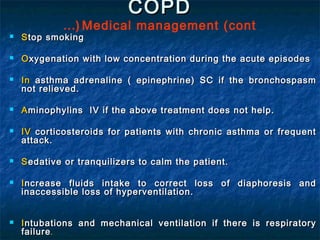
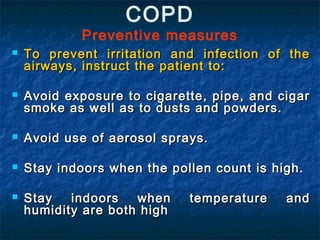
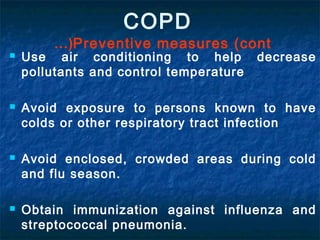
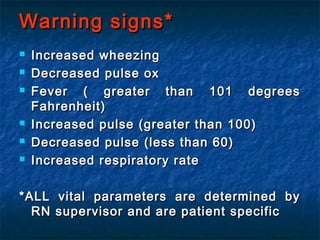
The document discusses chronic obstructive pulmonary disease (COPD), including its definition as a progressive lung disease characterized by limited airflow; causes such as smoking, air pollution, and genetic factors; symptoms like breathlessness, cough, and sputum production; diagnostic tests and medical management including bronchodilators, antibiotics, and oxygen therapy; preventive measures like smoking cessation and flu vaccines; and nursing interventions focused on assessment, education, and managing complications. COPD encompasses chronic bronchitis and emphysema and is a serious lung condition caused primarily by smoking.