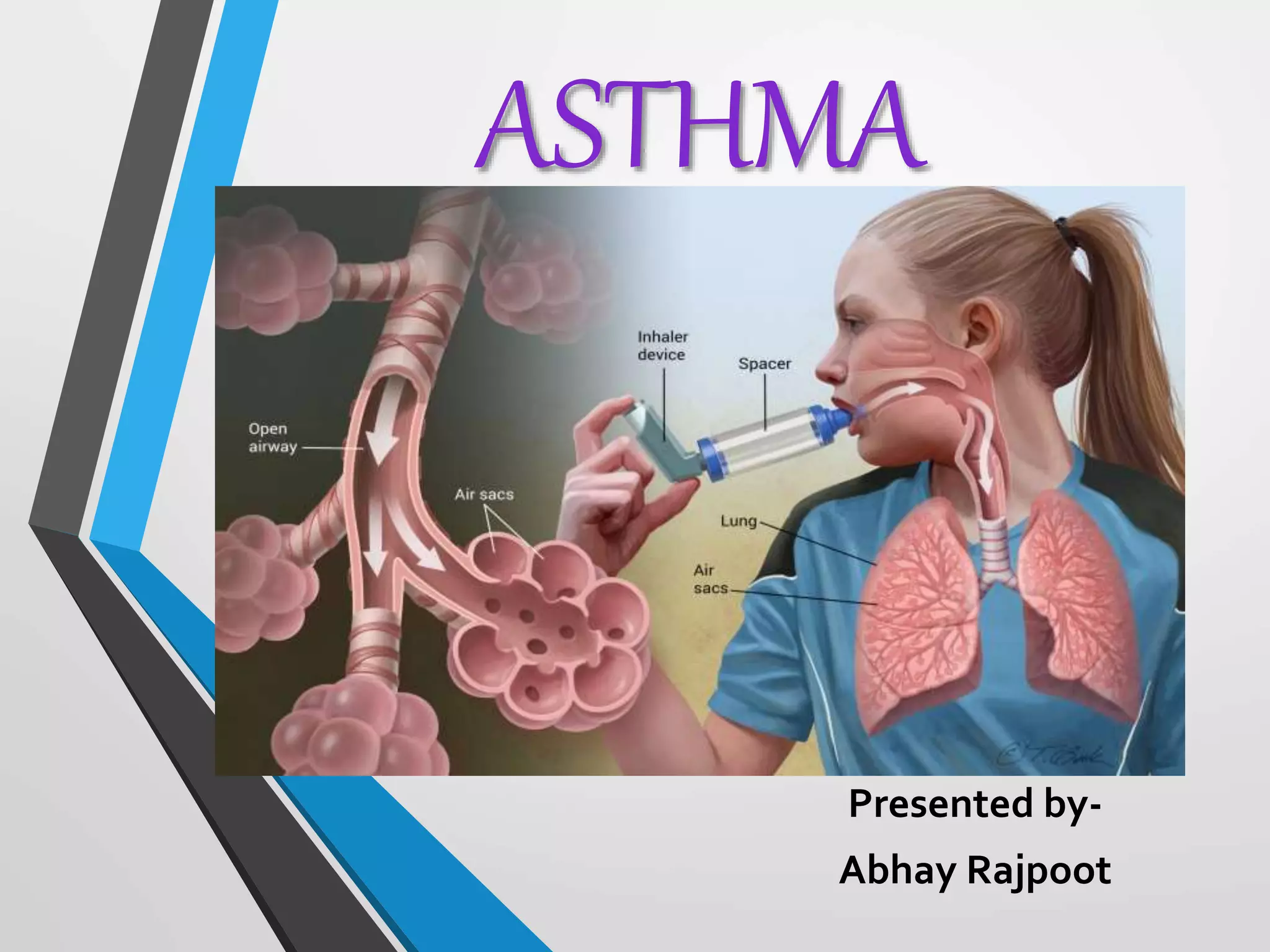
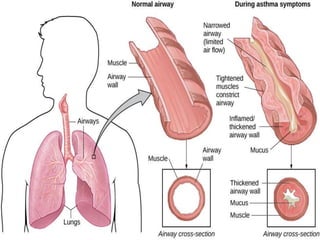
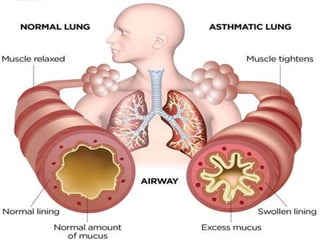
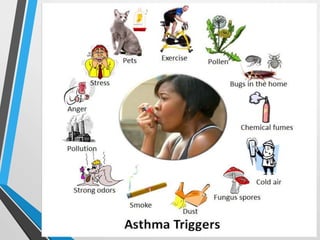
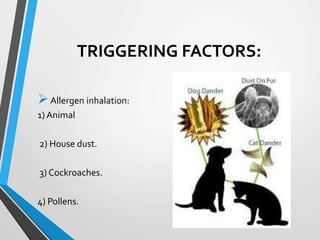
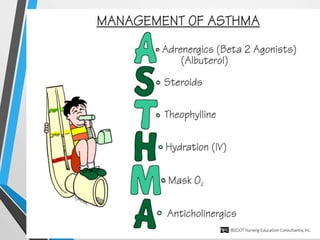
Asthma is a chronic inflammatory disorder of the airways, leading to symptoms like wheezing, breathlessness, and cough, with a higher prevalence among adult women. The condition is influenced by various triggers, including allergens, air pollutants, and occupational exposures, and classified into types such as allergic, non-allergic, and mixed asthma. Treatment includes long-term control medications, quick relief options, and patient education on proper medication use, with lifestyle factors like vitamin D levels playing a role in management.