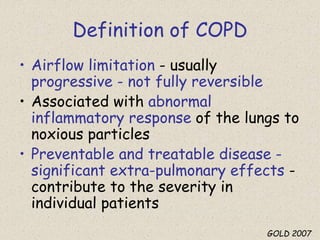
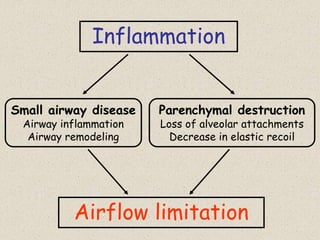
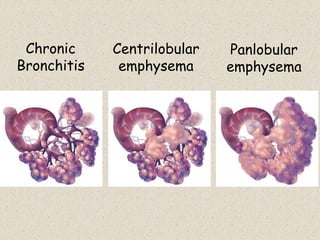
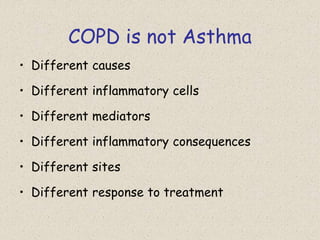
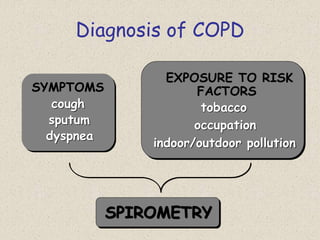
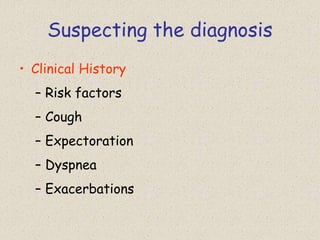
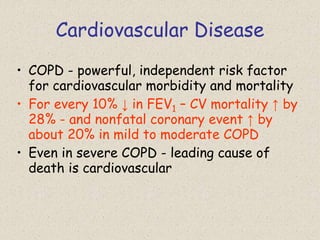
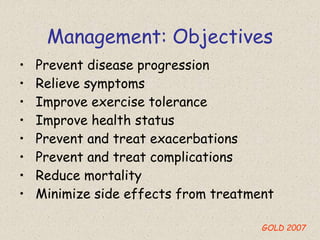
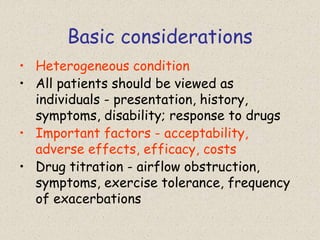
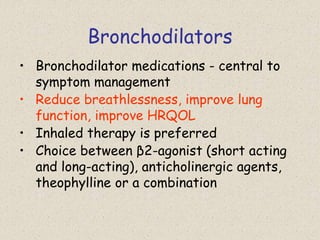
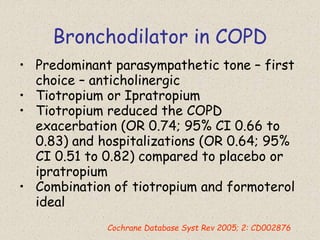
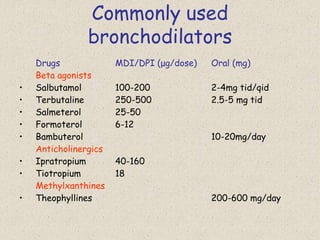
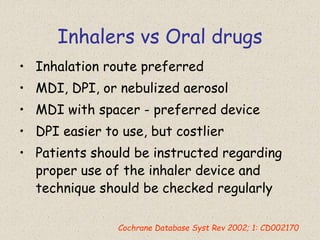
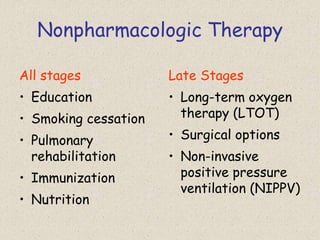
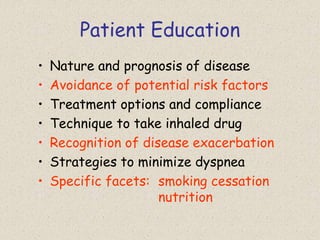
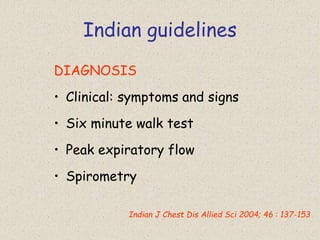
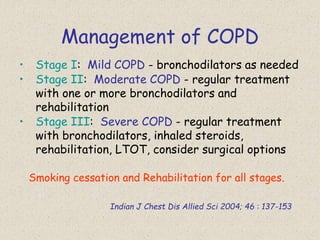
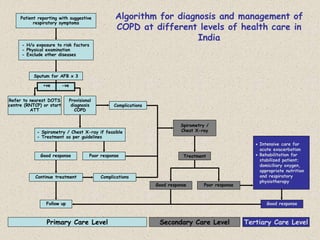
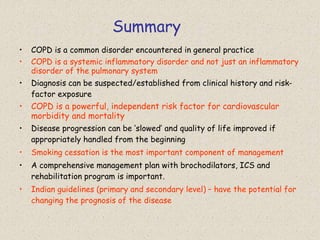
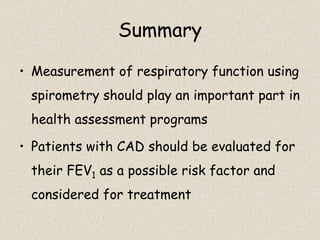
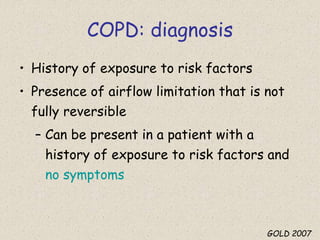
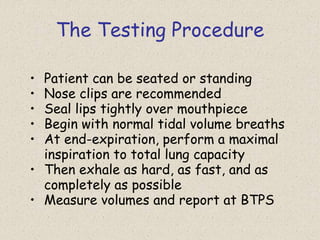
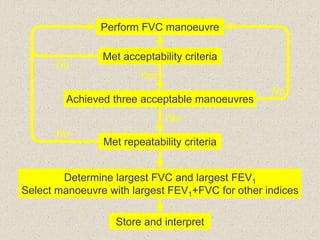
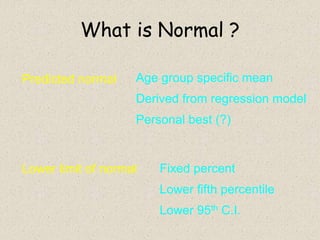
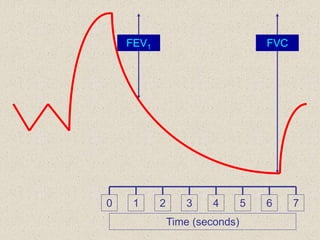
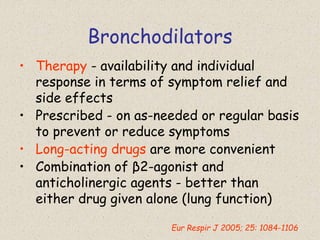
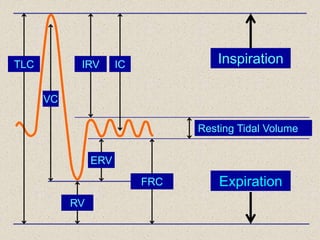
This document discusses chronic obstructive pulmonary disease (COPD). It defines COPD as a progressive airway disease associated with abnormal lung inflammation in response to noxious particles. Key features include small airway disease, airway remodeling, and parenchymal destruction leading to airflow limitation. The document reviews the epidemiology and burden of COPD in India, mechanisms of inflammation and different COPD phenotypes. It emphasizes the importance of spirometry in diagnosis and differentiating COPD from asthma. Management strategies discussed include smoking cessation, bronchodilators, pulmonary rehabilitation and long-term oxygen therapy. The document also provides Indian guidelines for COPD diagnosis and management at primary, secondary and tertiary levels of care.




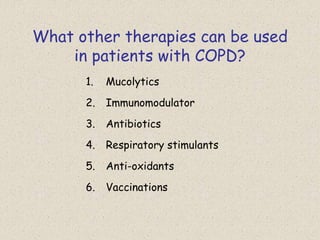




![Other drugs
• Vaccines – Influenza and Pneumococcus –
in all patients
• Oral mucolytics - reduce the viscosity of
sputum, no effect on lung function
• Oral immunostimulatory agent – OM-85
BV (extract of 8 bacteria) - recurrent
exacerbations
• Antioxidants - N-acetylcysteine- no clear
role [Lancet 2005; 365: 1552–60 ]
GOLD 2007](https://image.slidesharecdn.com/copd-ldhjan2010-230708045651-5dcd1823/85/COPD-Ldh-Jan-2010-ppt-70-320.jpg)