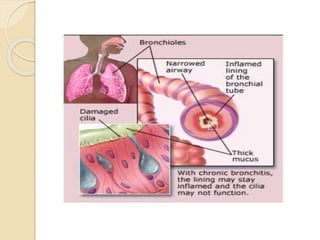
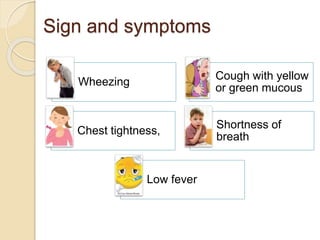
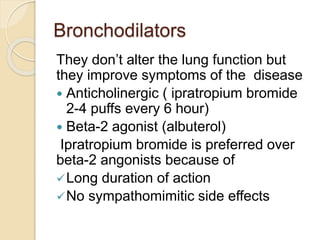
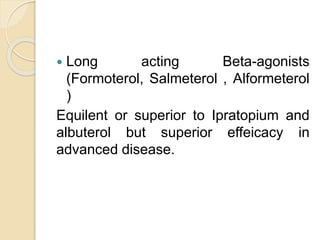
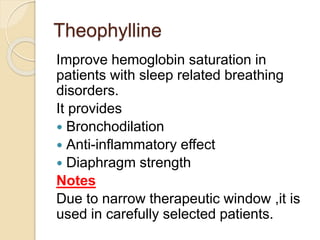
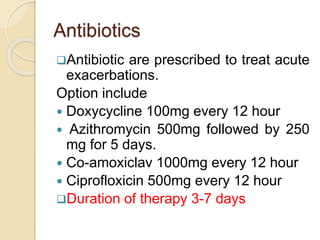
Bronchitis is an inflammation of the air passages between the nose and lungs. Acute bronchitis usually follows a viral infection like a cold and resolves within two weeks, while chronic bronchitis presents symptoms for at least three months per year for two consecutive years, often caused by smoking. Treatment for acute bronchitis focuses on air flow optimization using expectorants, bronchodilators, and sometimes antibiotics or corticosteroids. Treatment for chronic bronchitis emphasizes smoking cessation and uses long-acting bronchodilators and inhaled corticosteroids to manage symptoms.