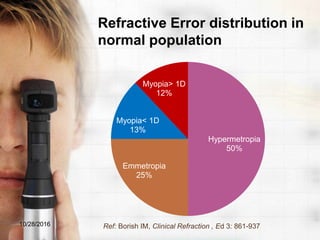
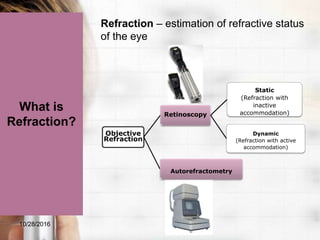
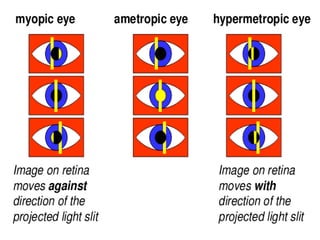
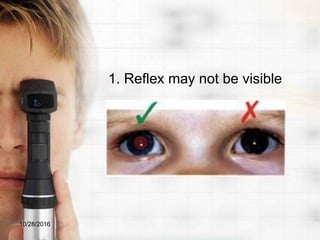
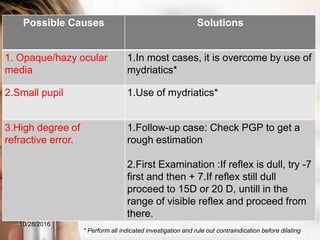
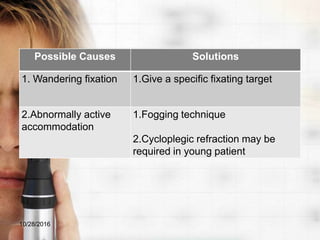
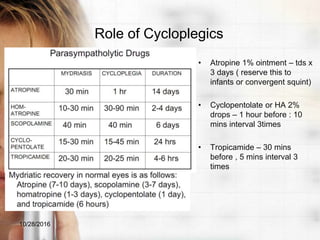
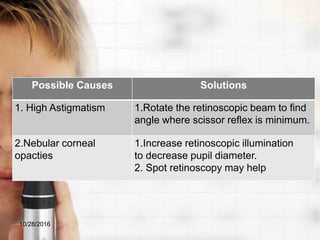
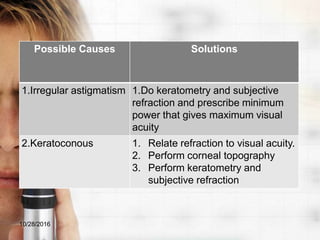
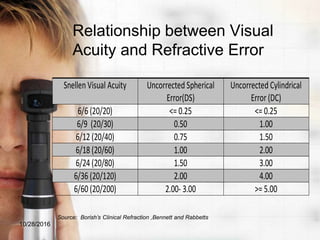
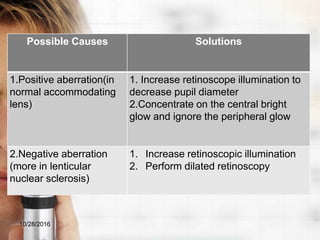
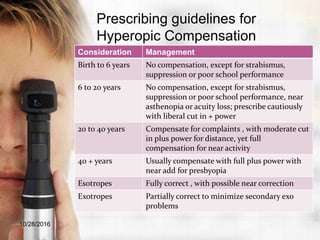
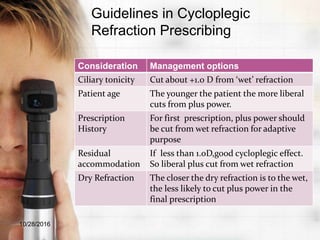
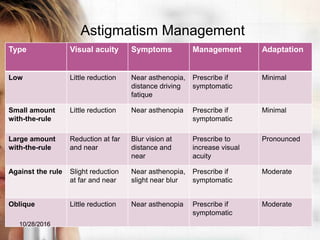
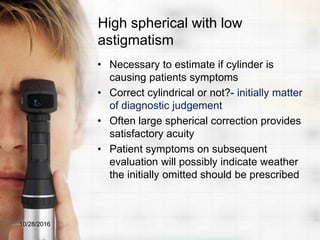
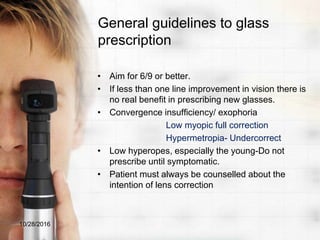
This document discusses various aspects of refractive error assessment and management. It begins by defining refractive error and describing its causes and treatment options. It then discusses the distribution of refractive errors in the normal population. Several sections provide details on objective refraction techniques like retinoscopy, including prerequisites, procedures, troubleshooting difficulties, and the importance of retinoscopy. Guidelines are provided for prescribing for various refractive error types and patient characteristics.