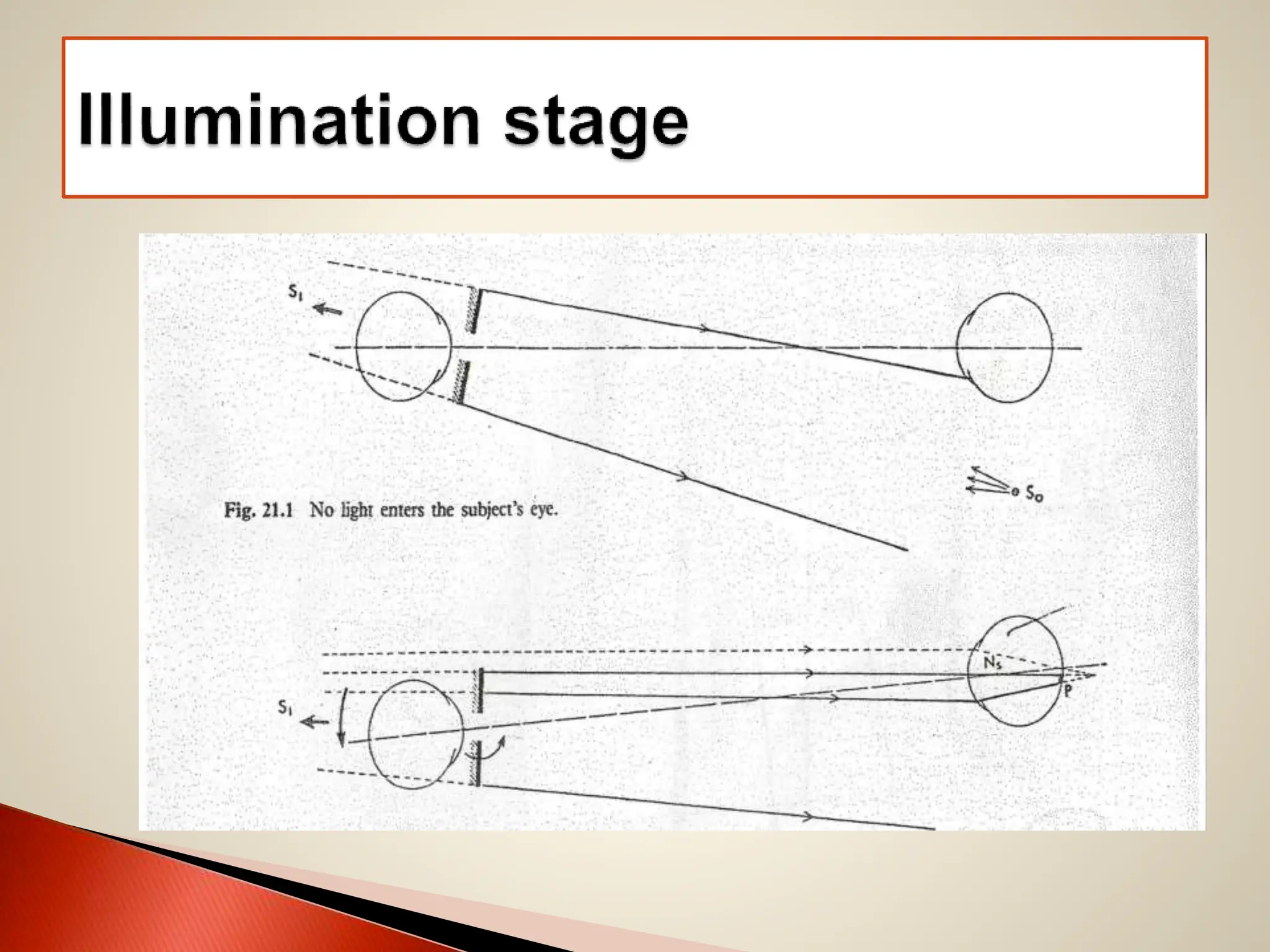
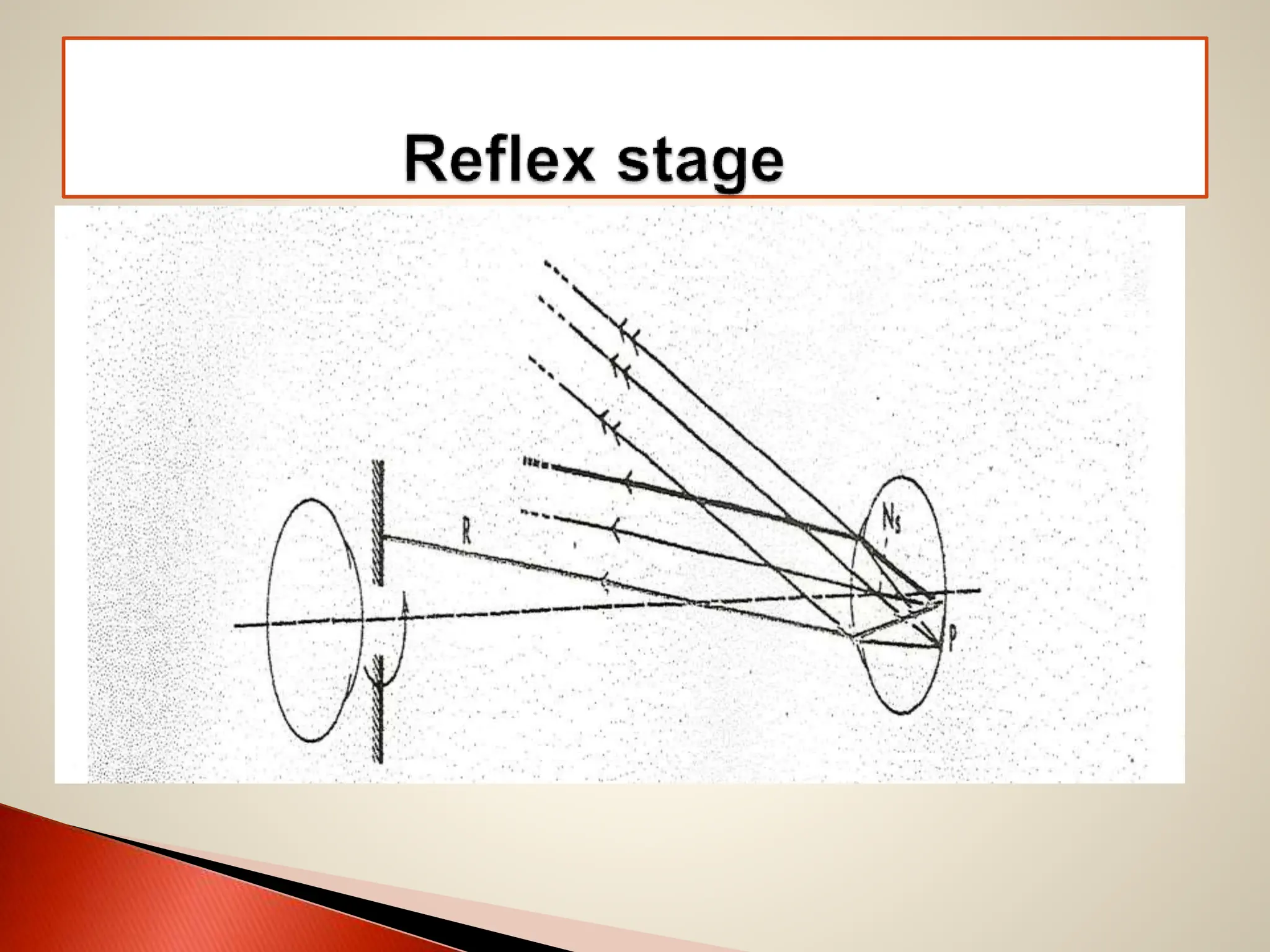
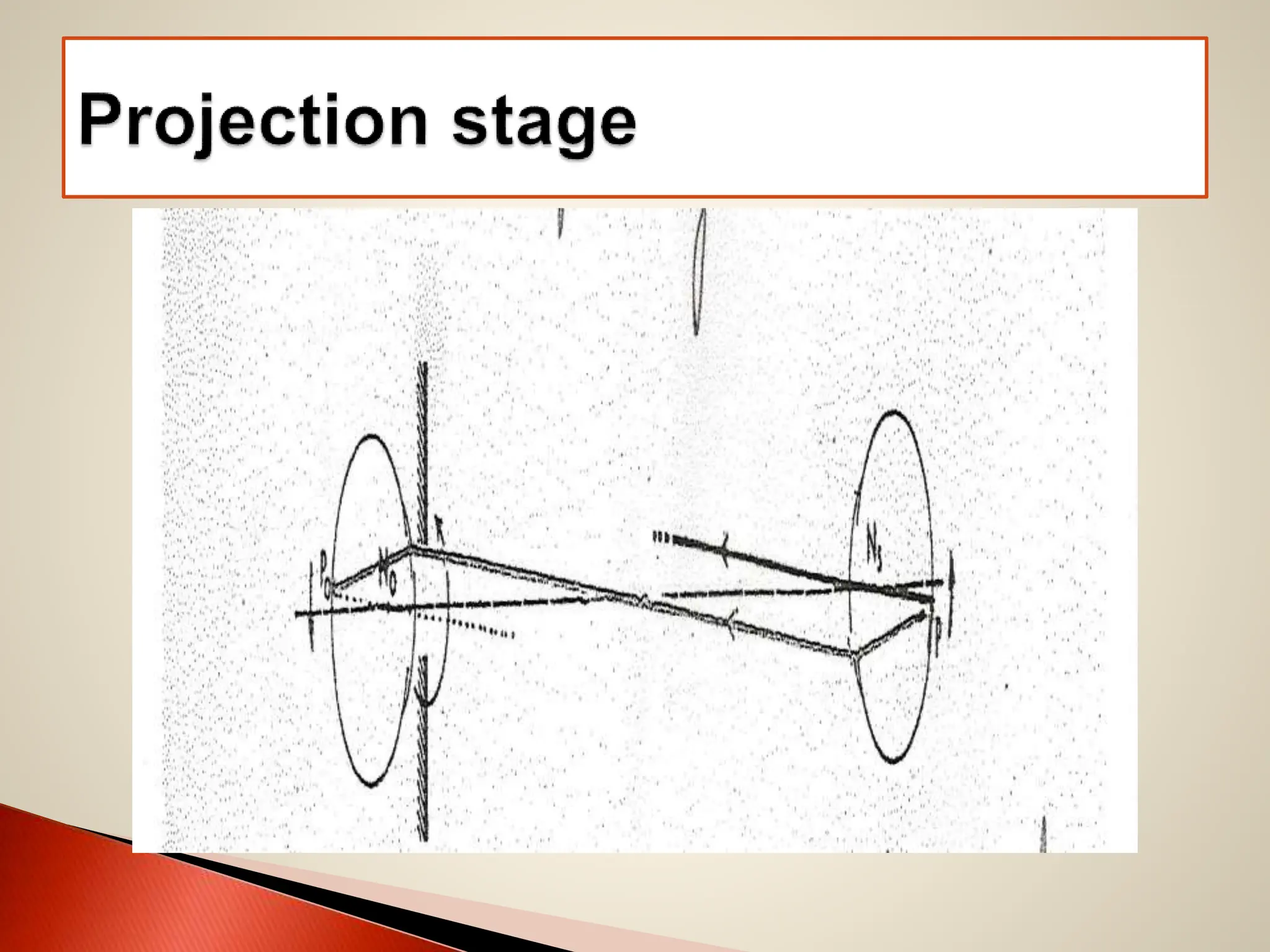
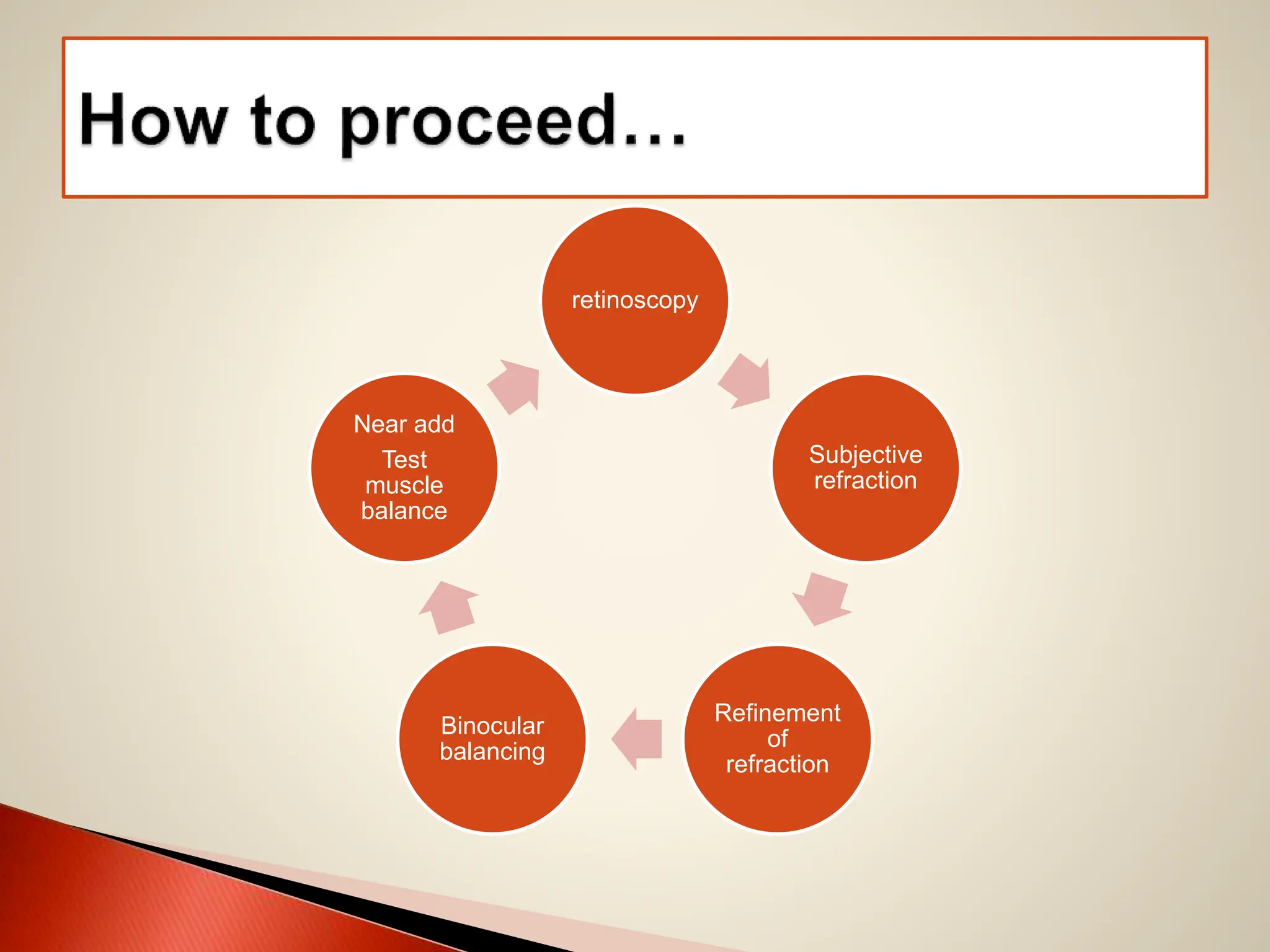
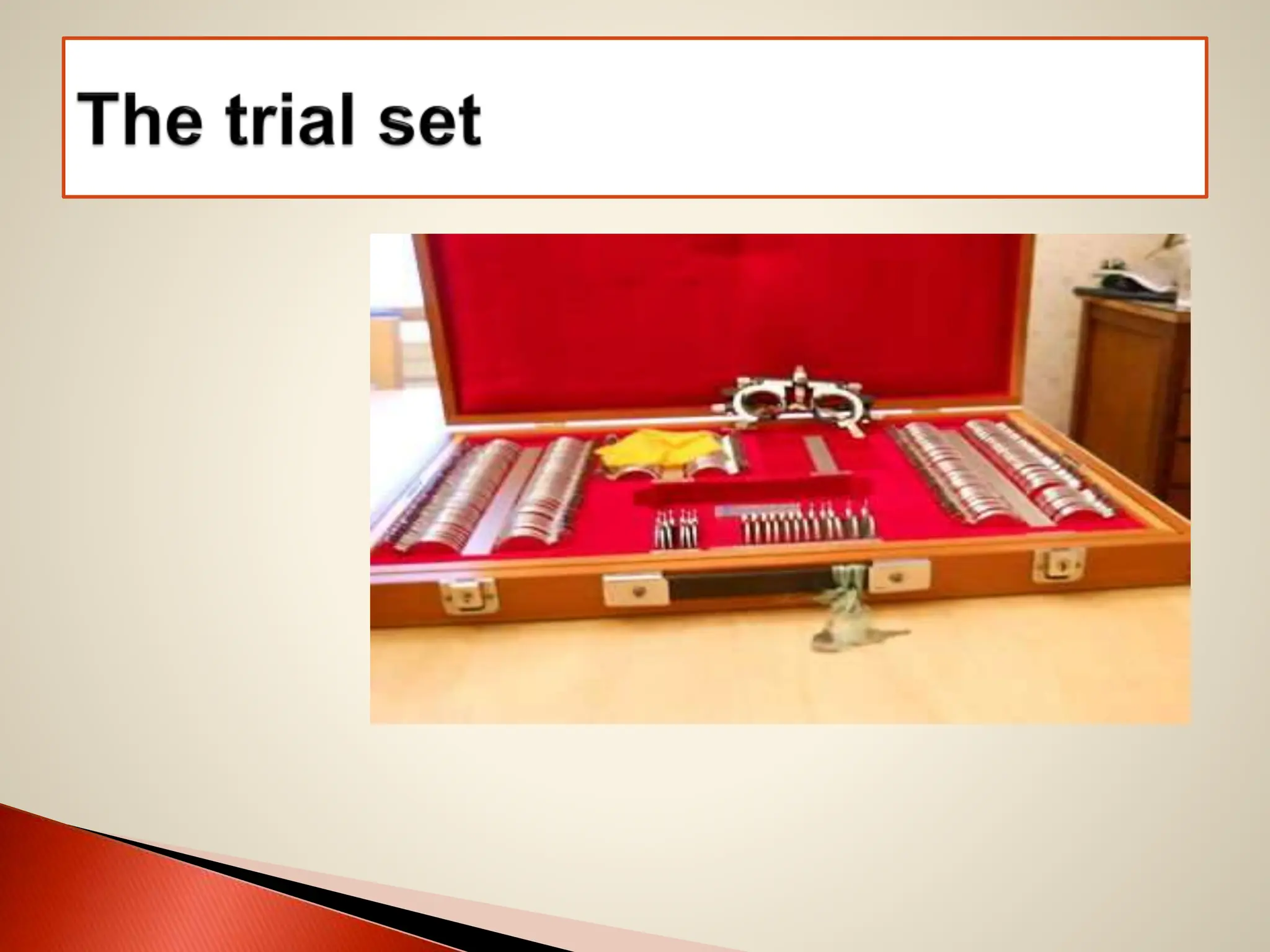
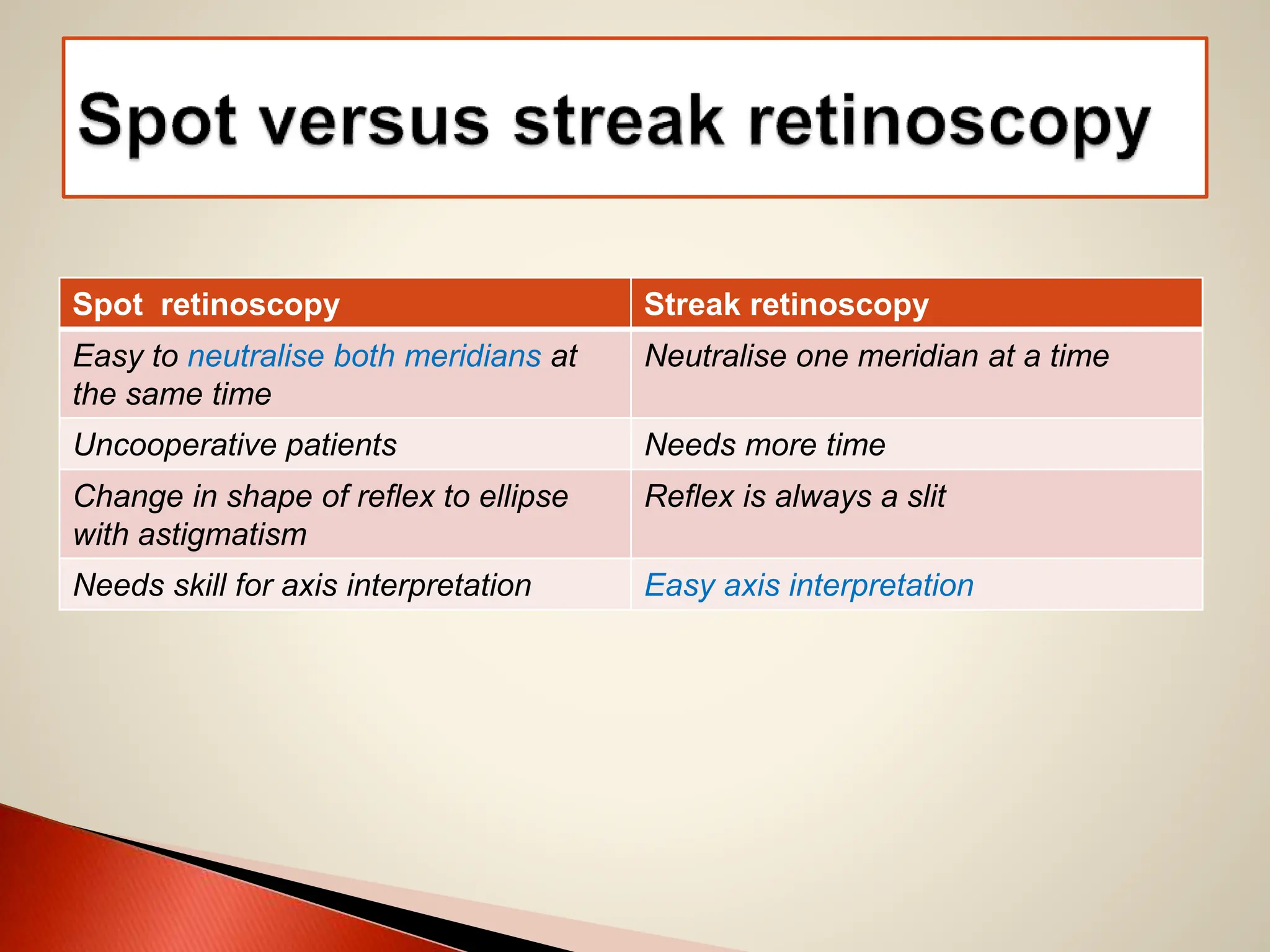
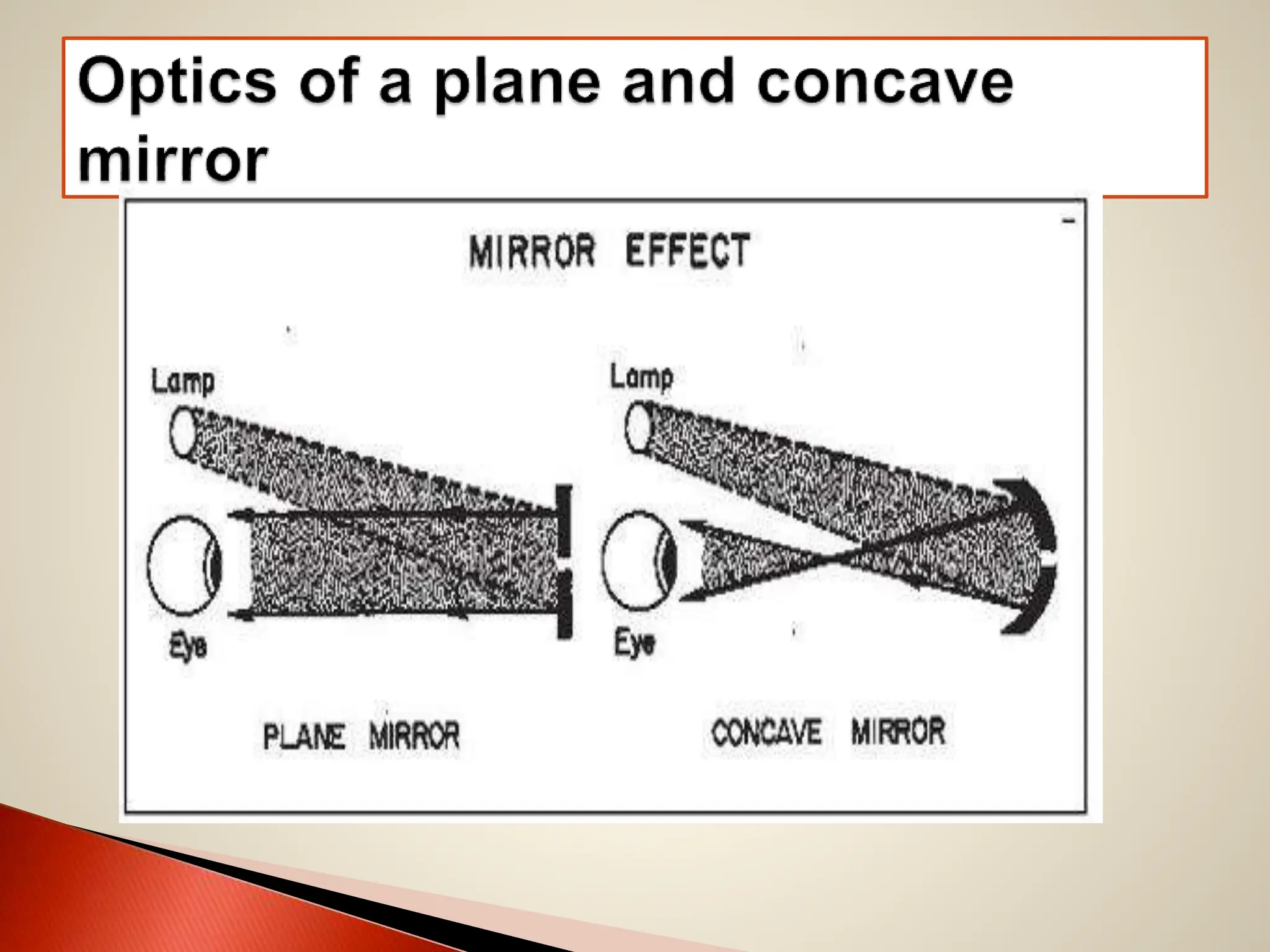
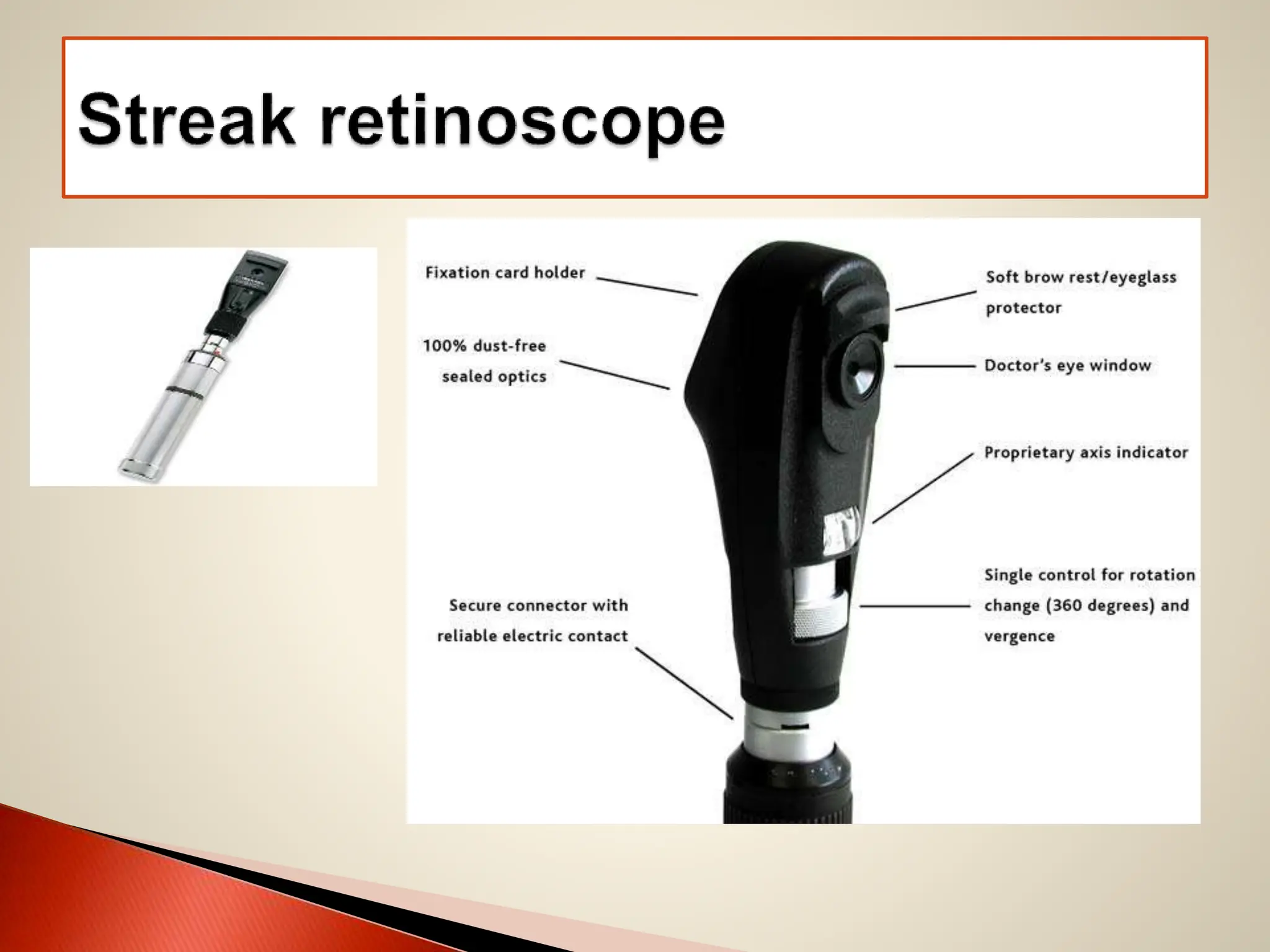
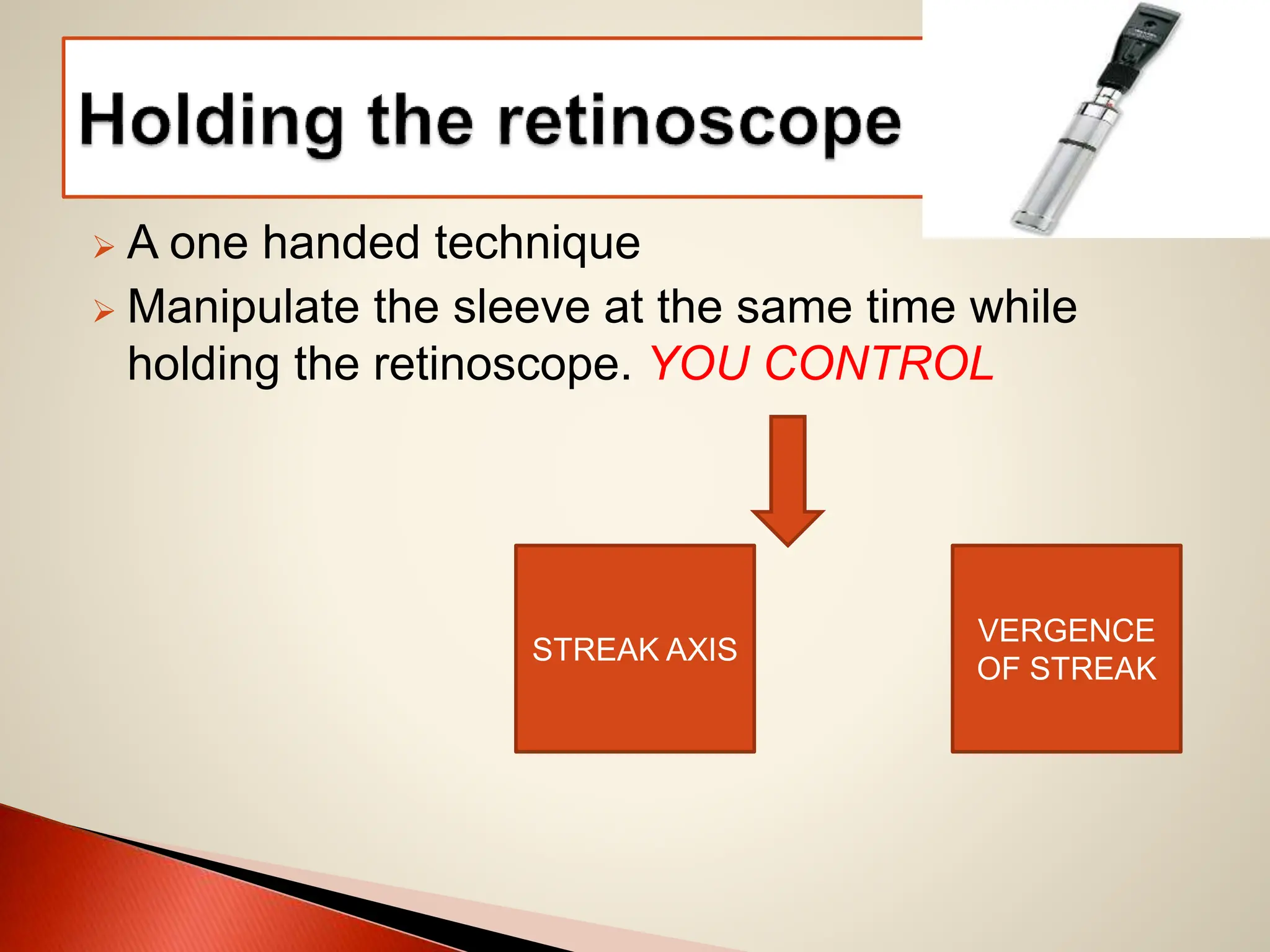
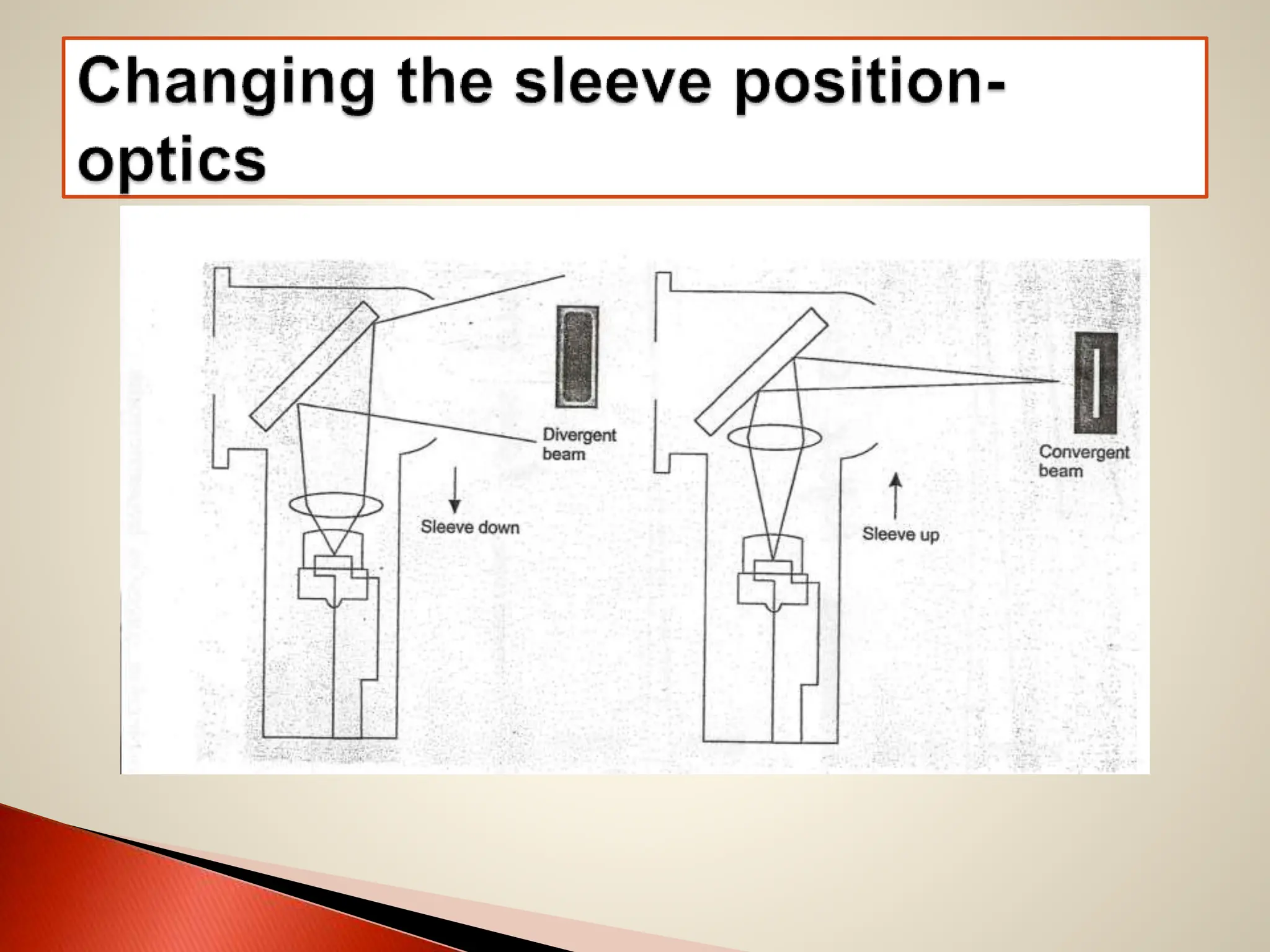
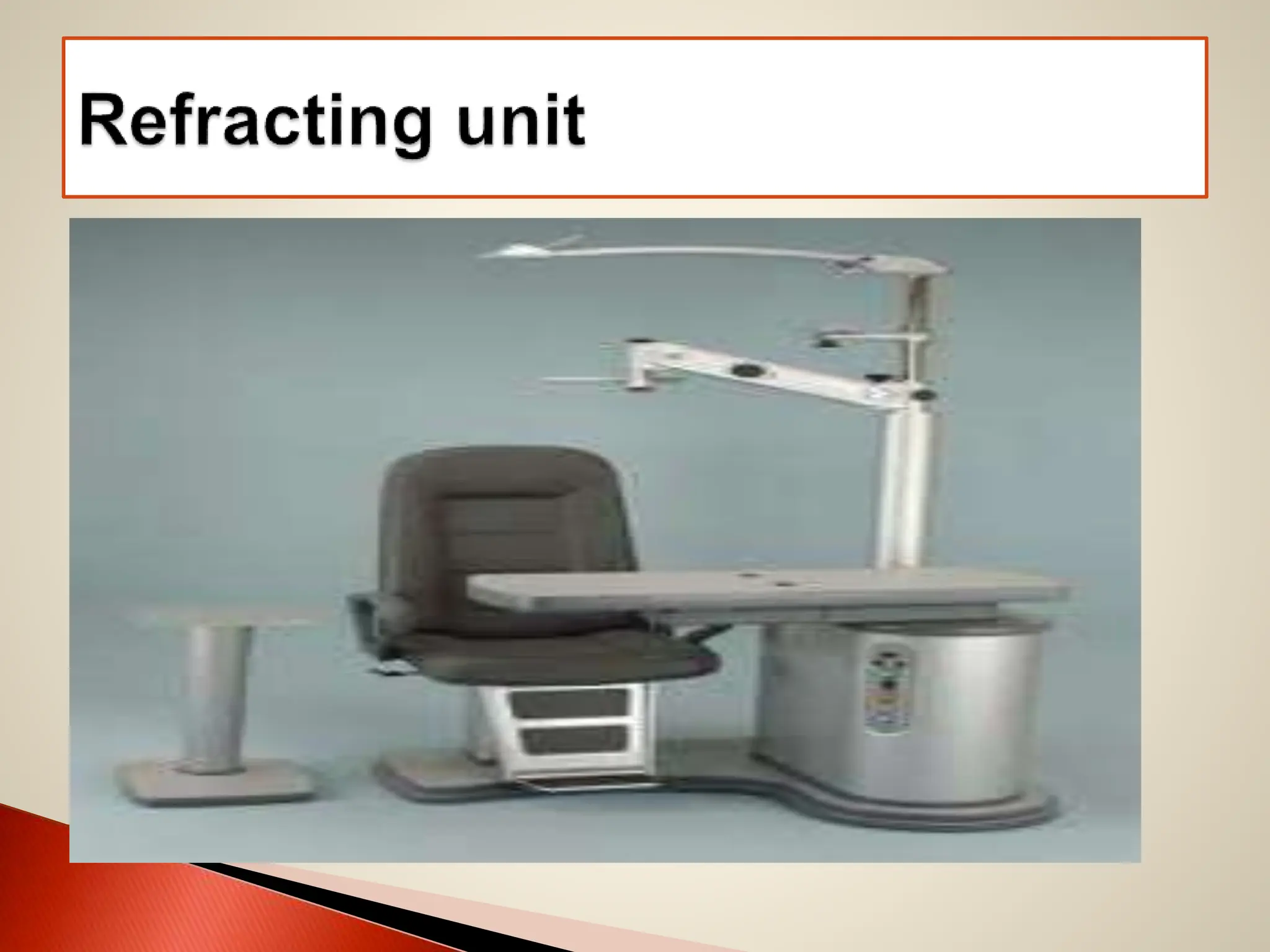
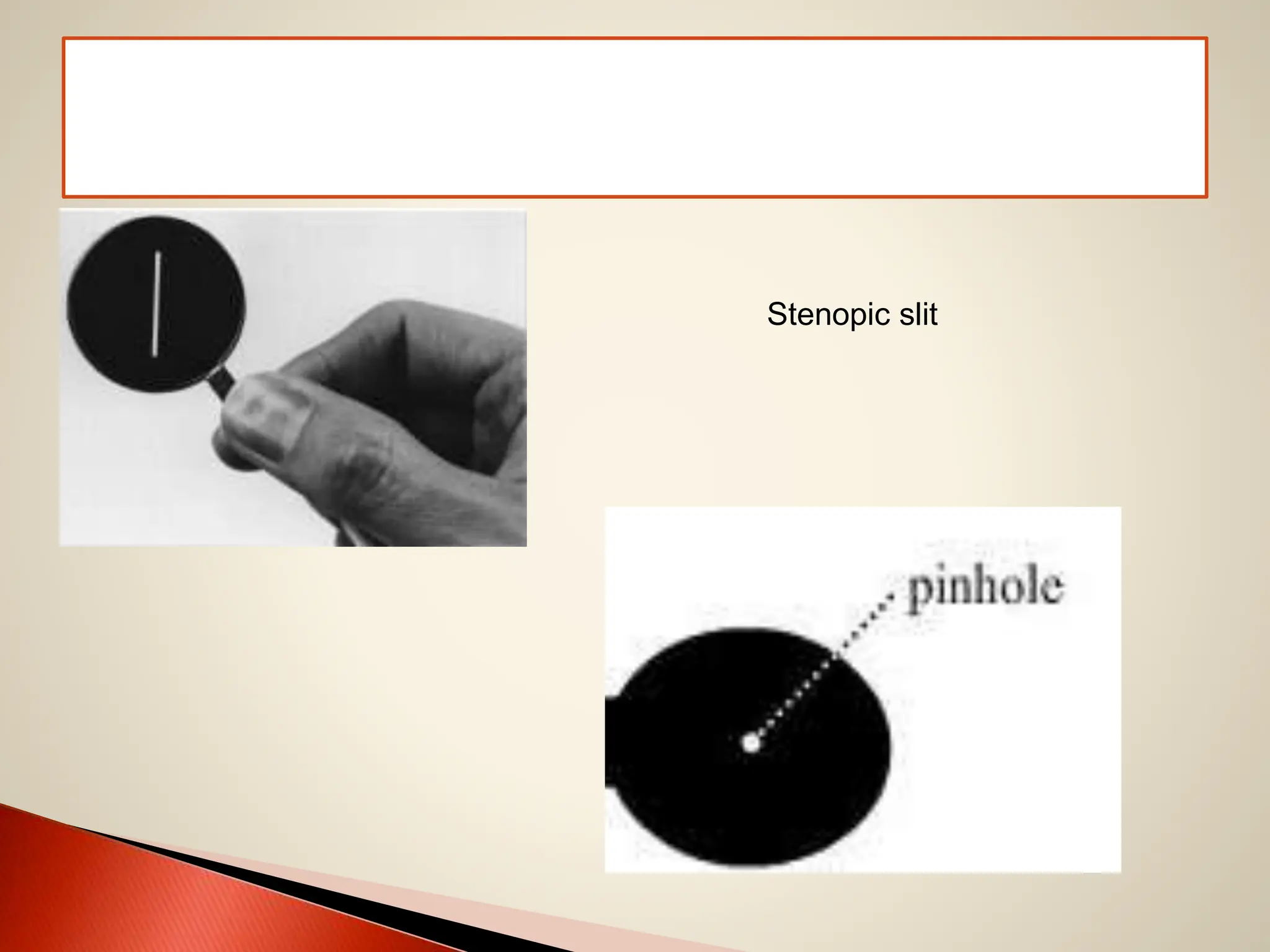
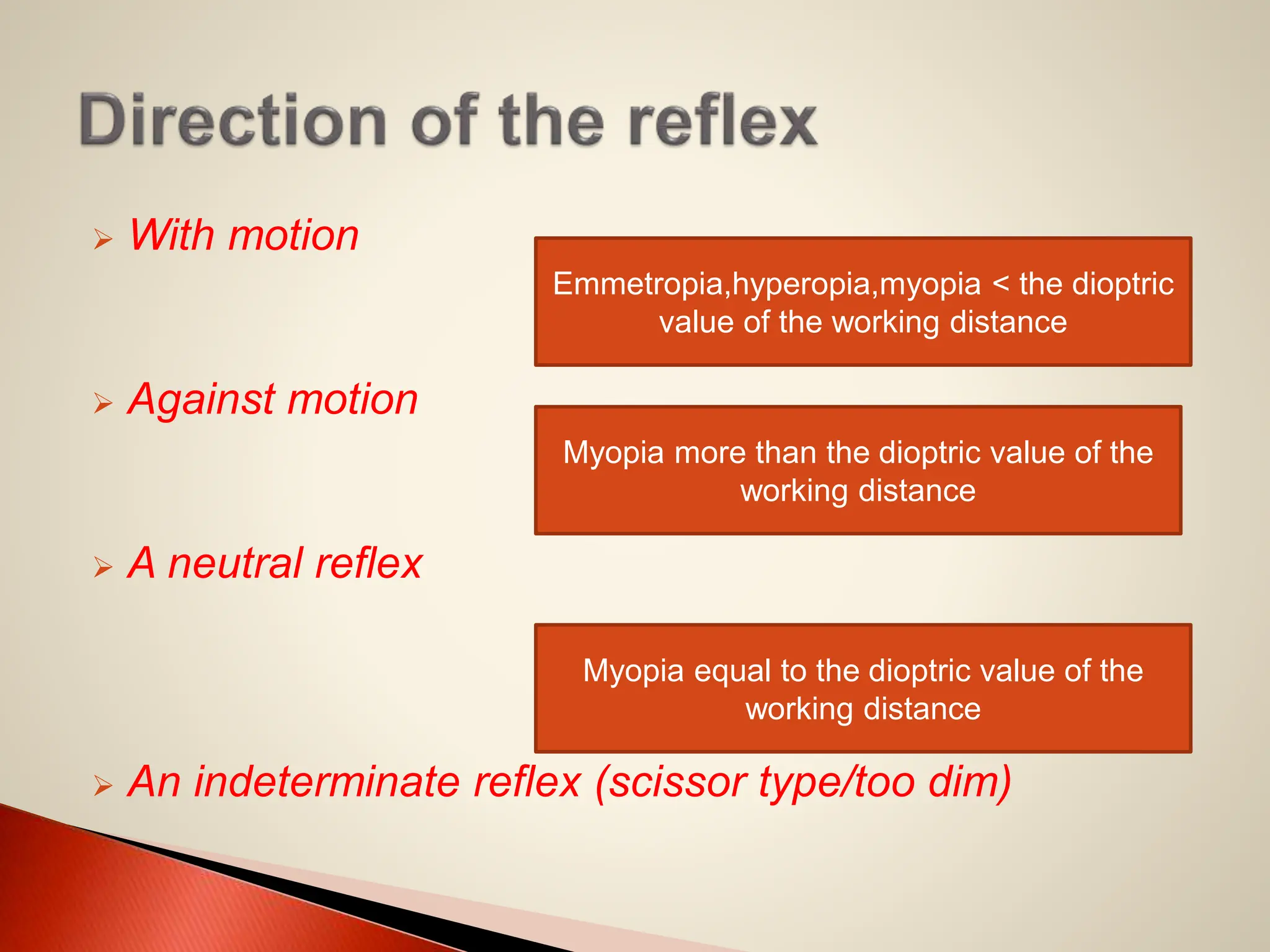
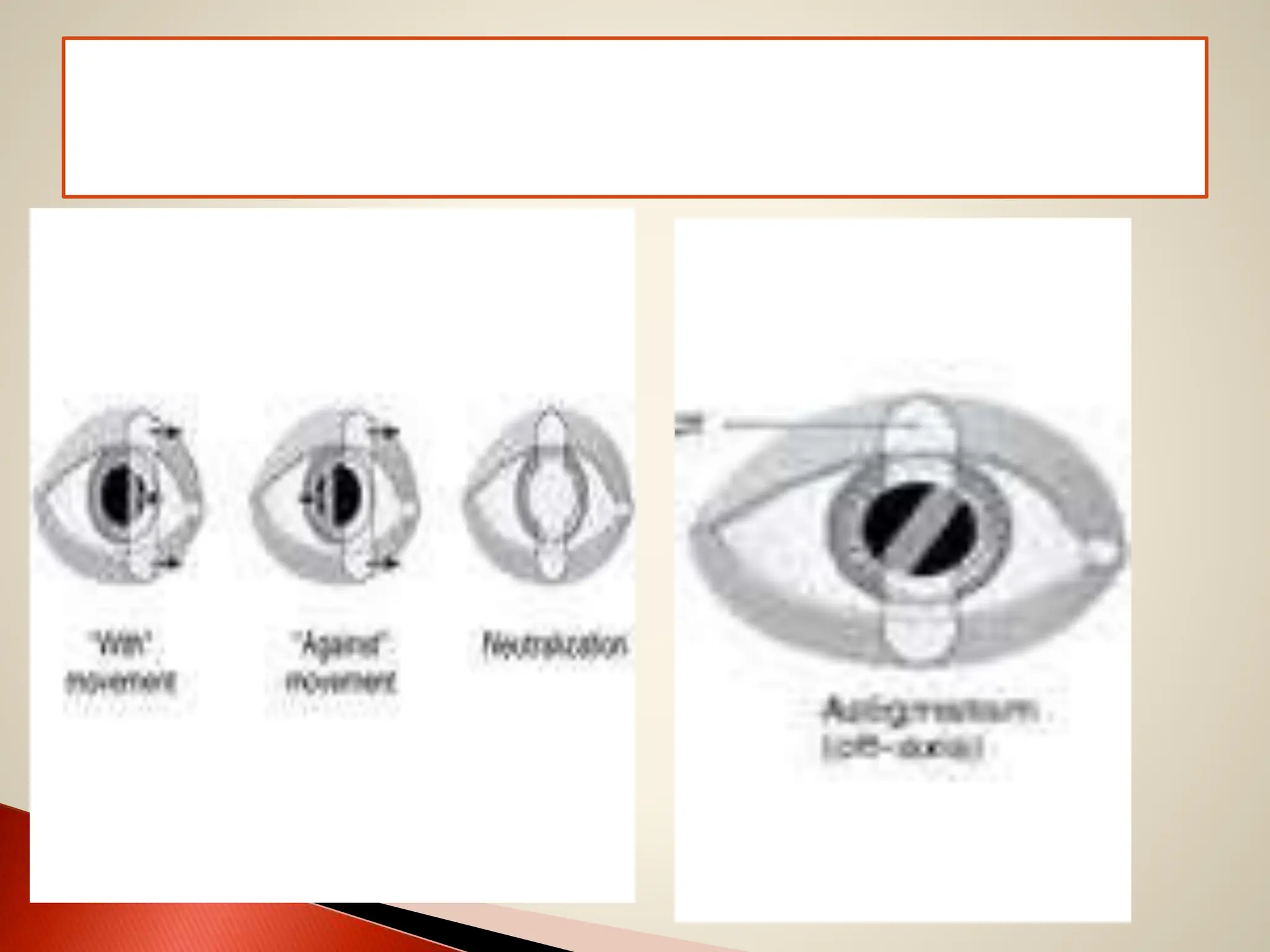
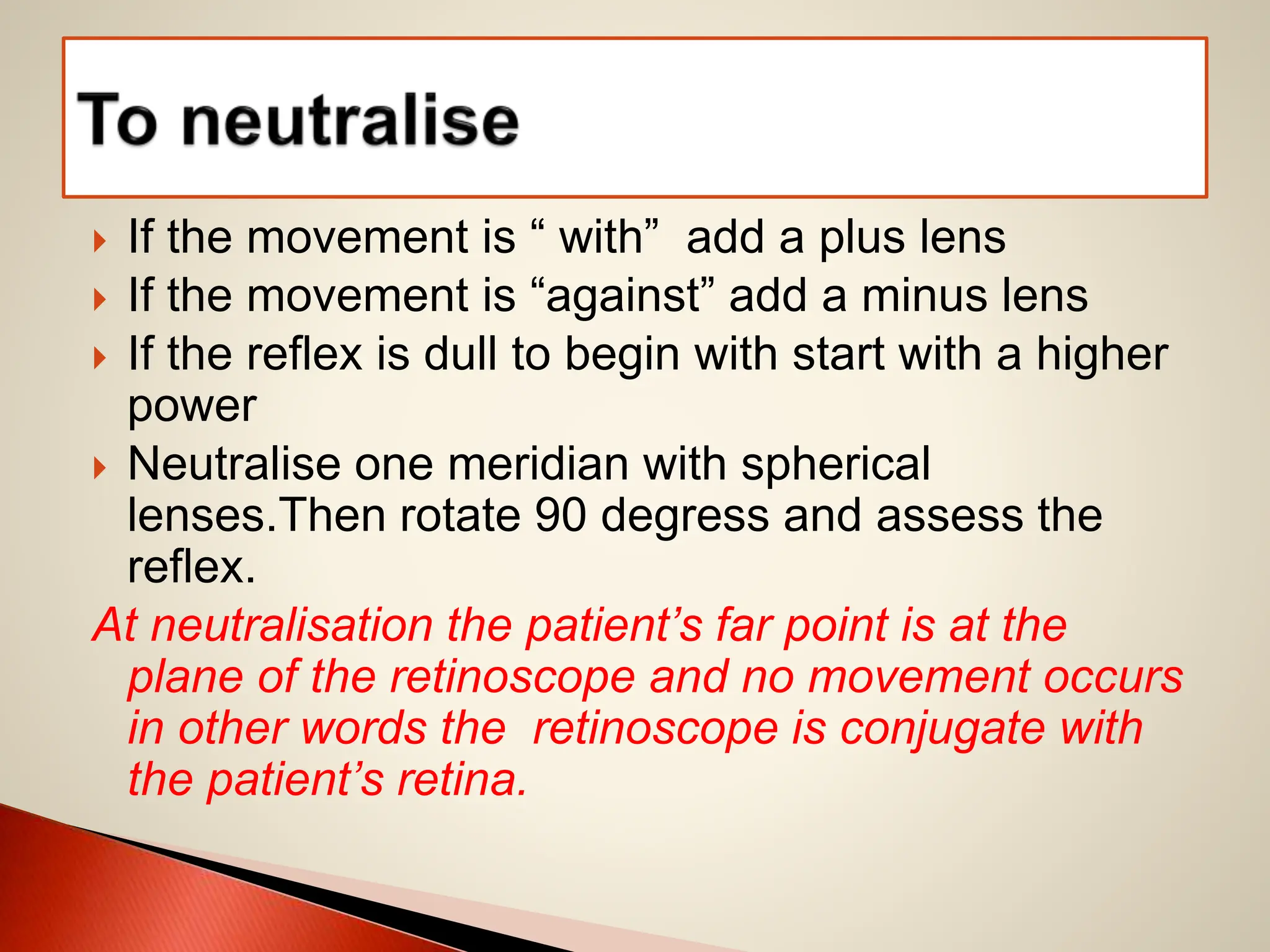
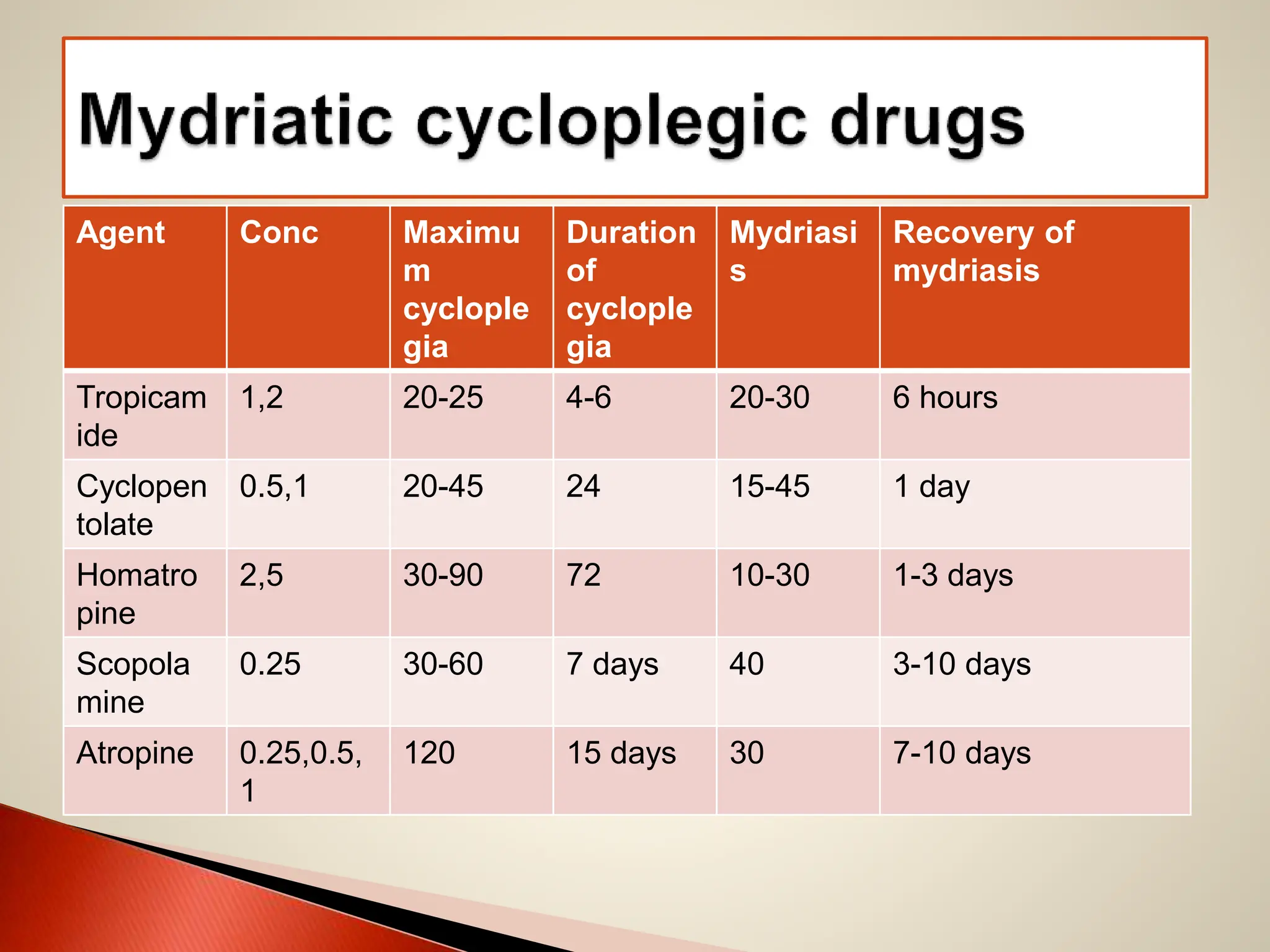
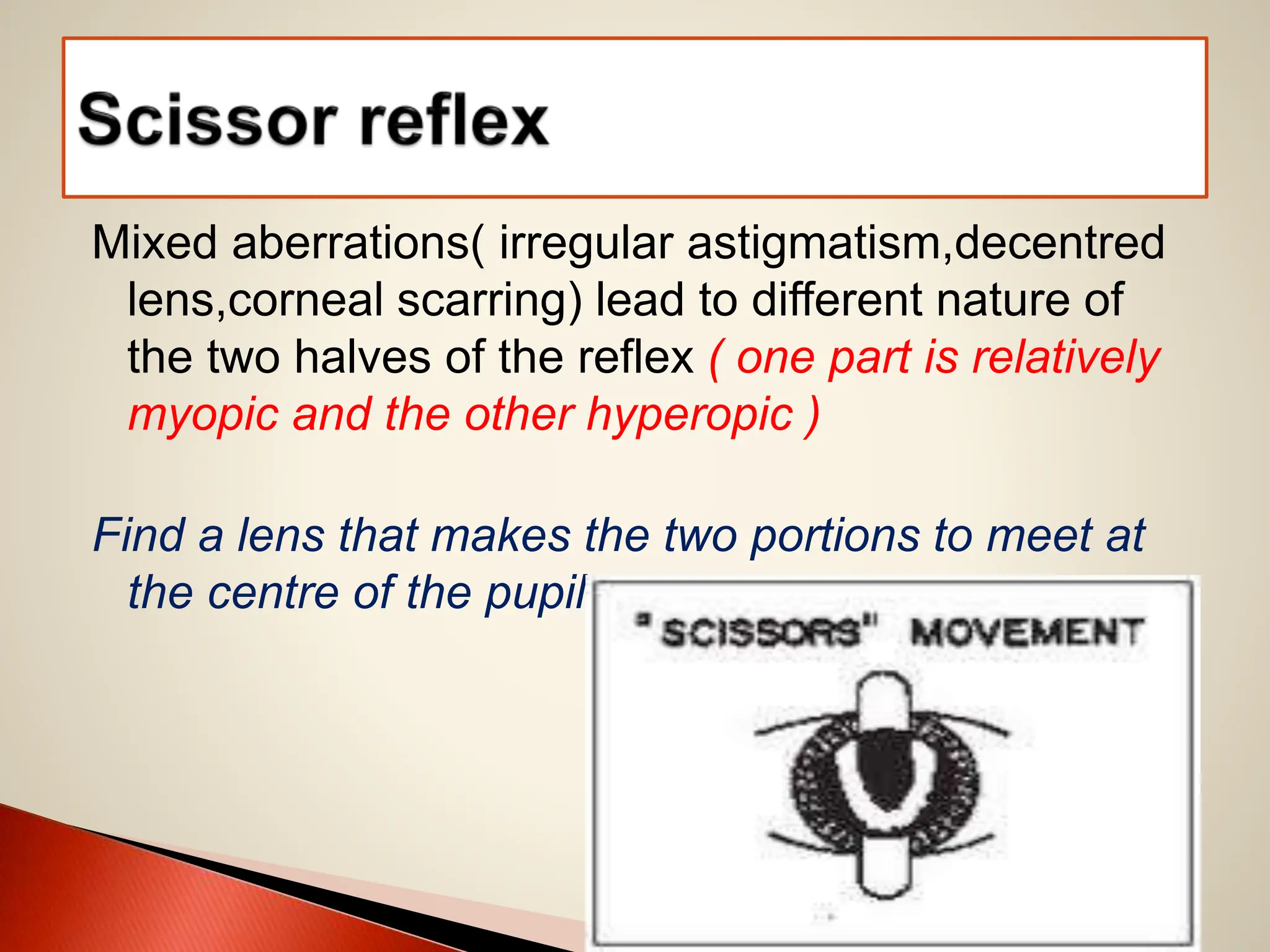
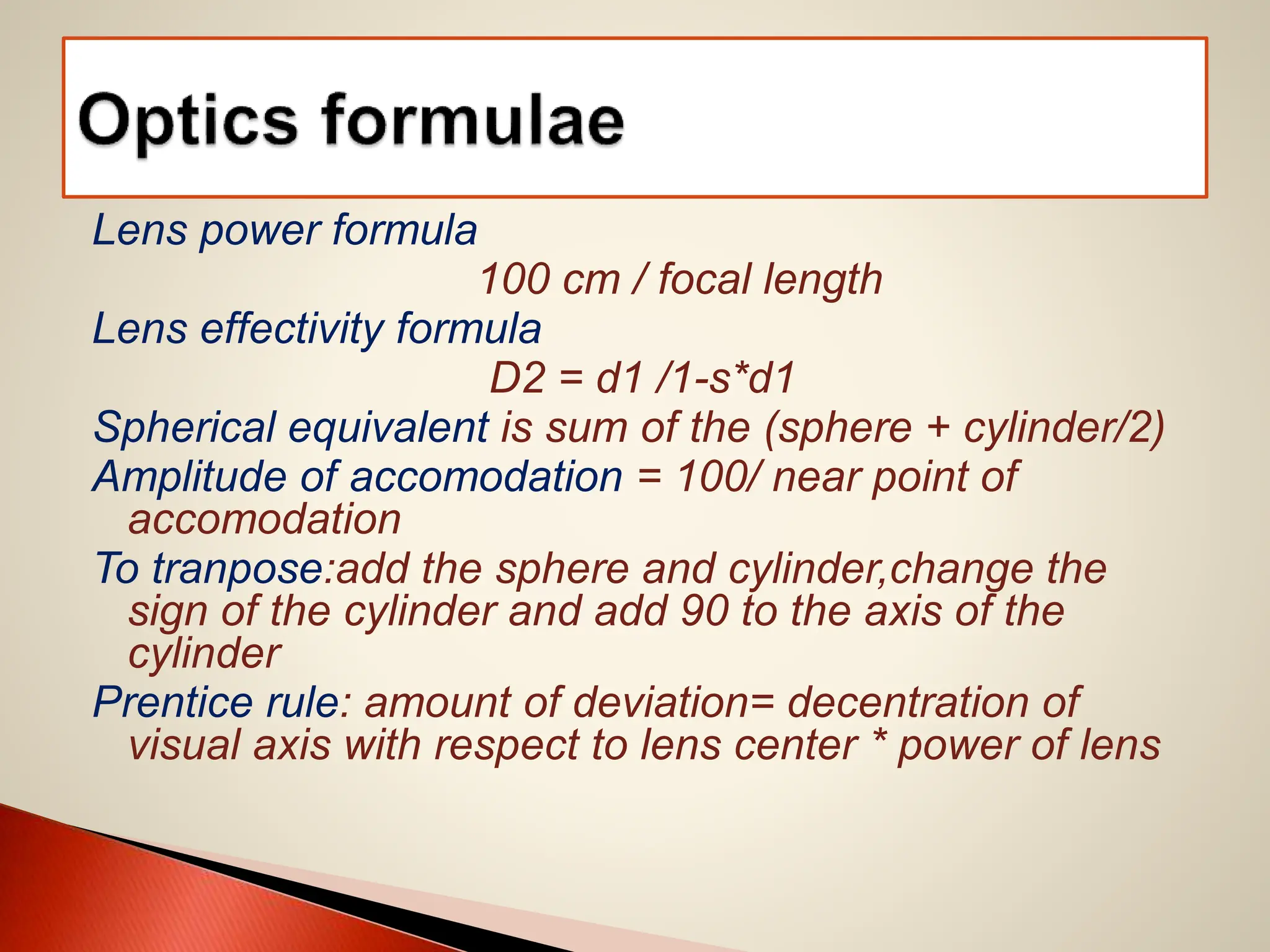
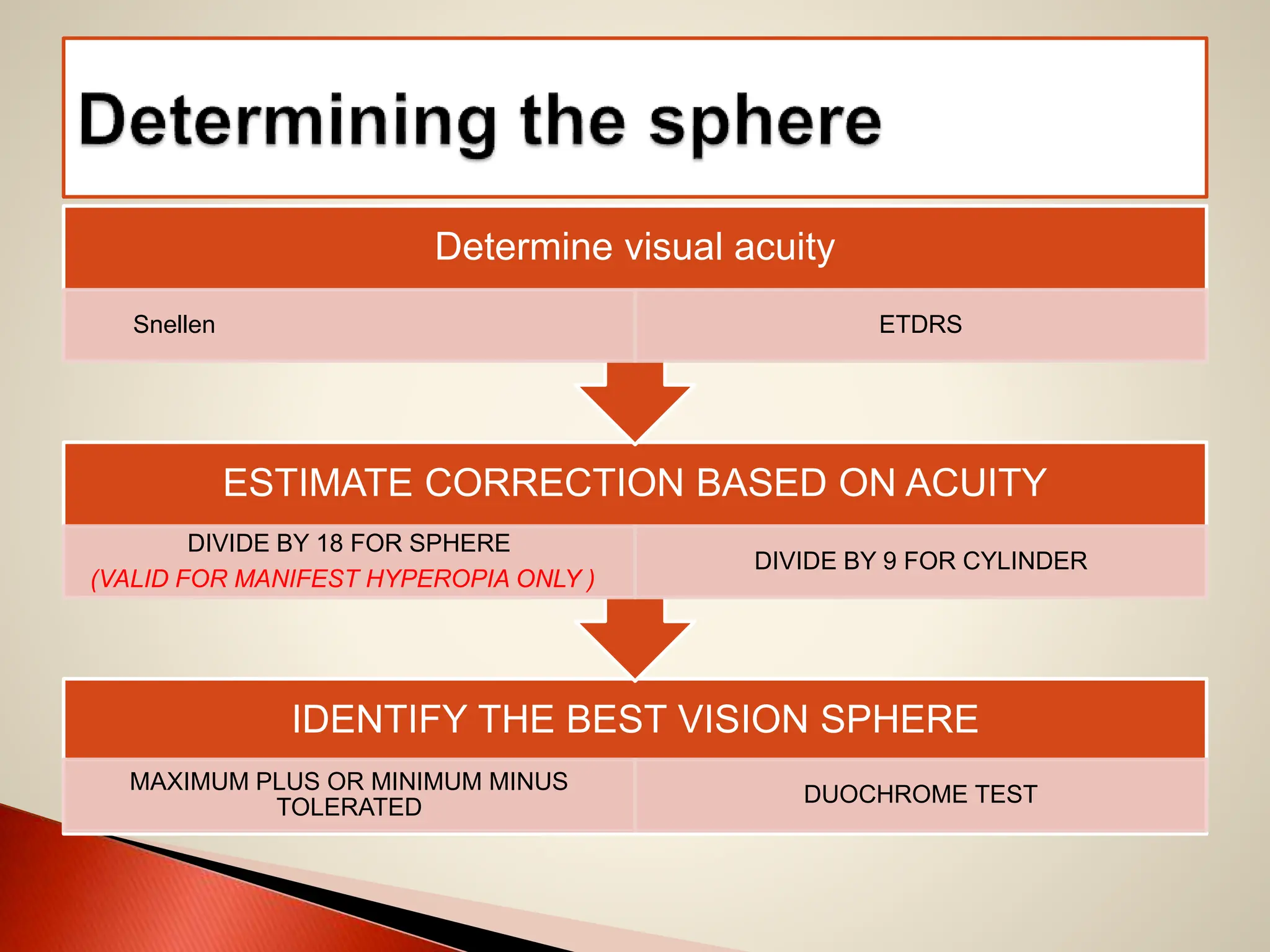
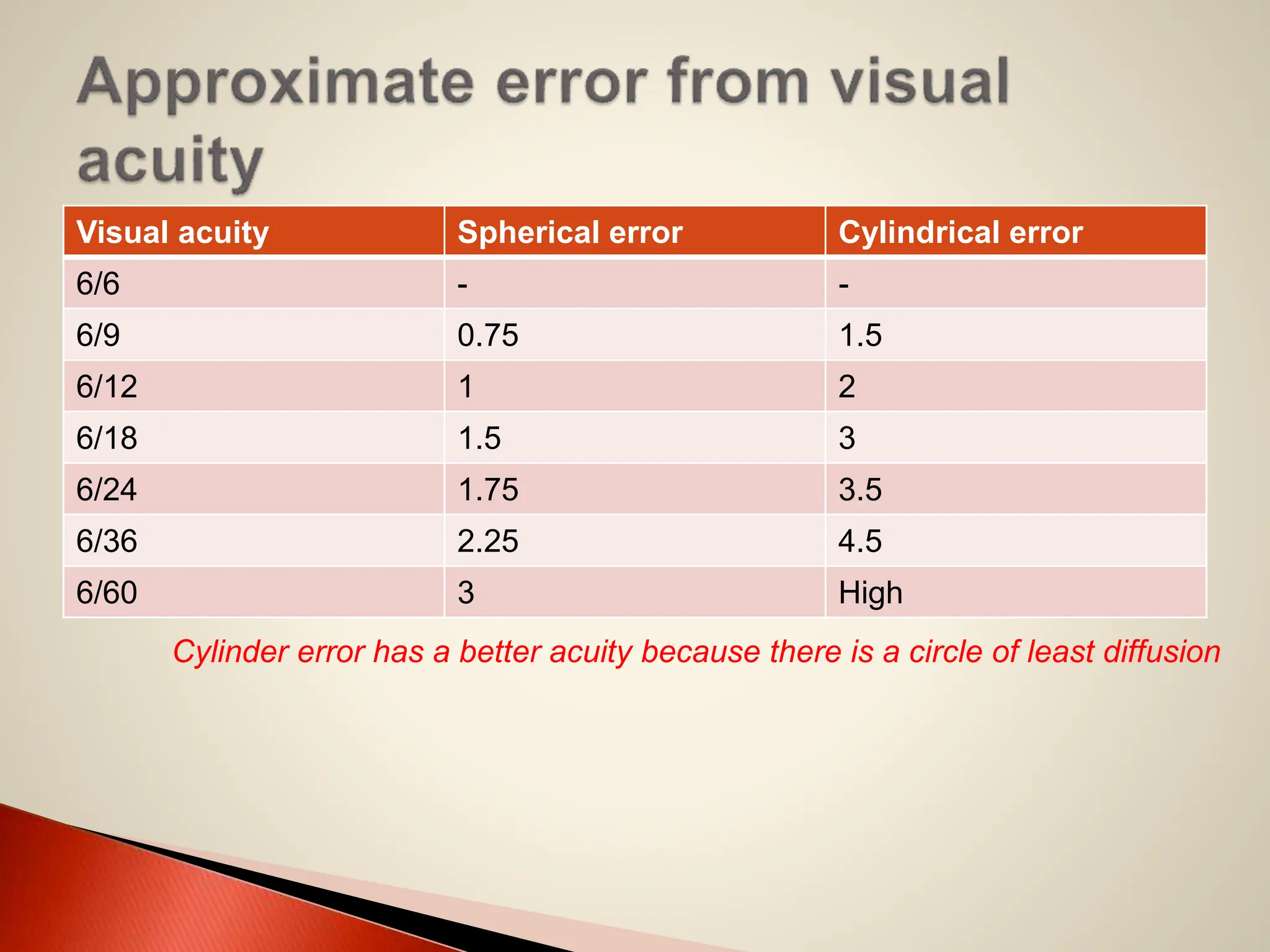
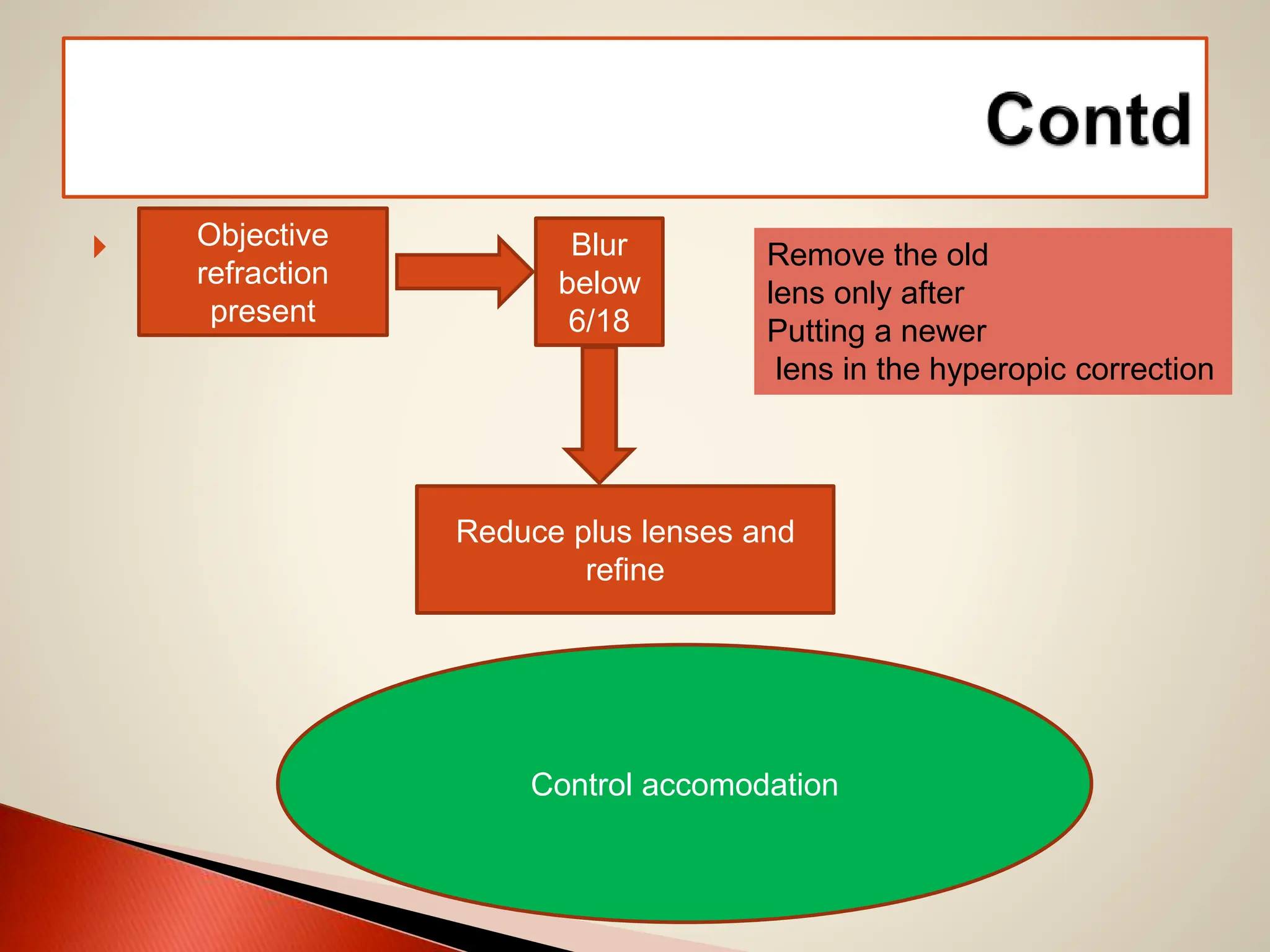
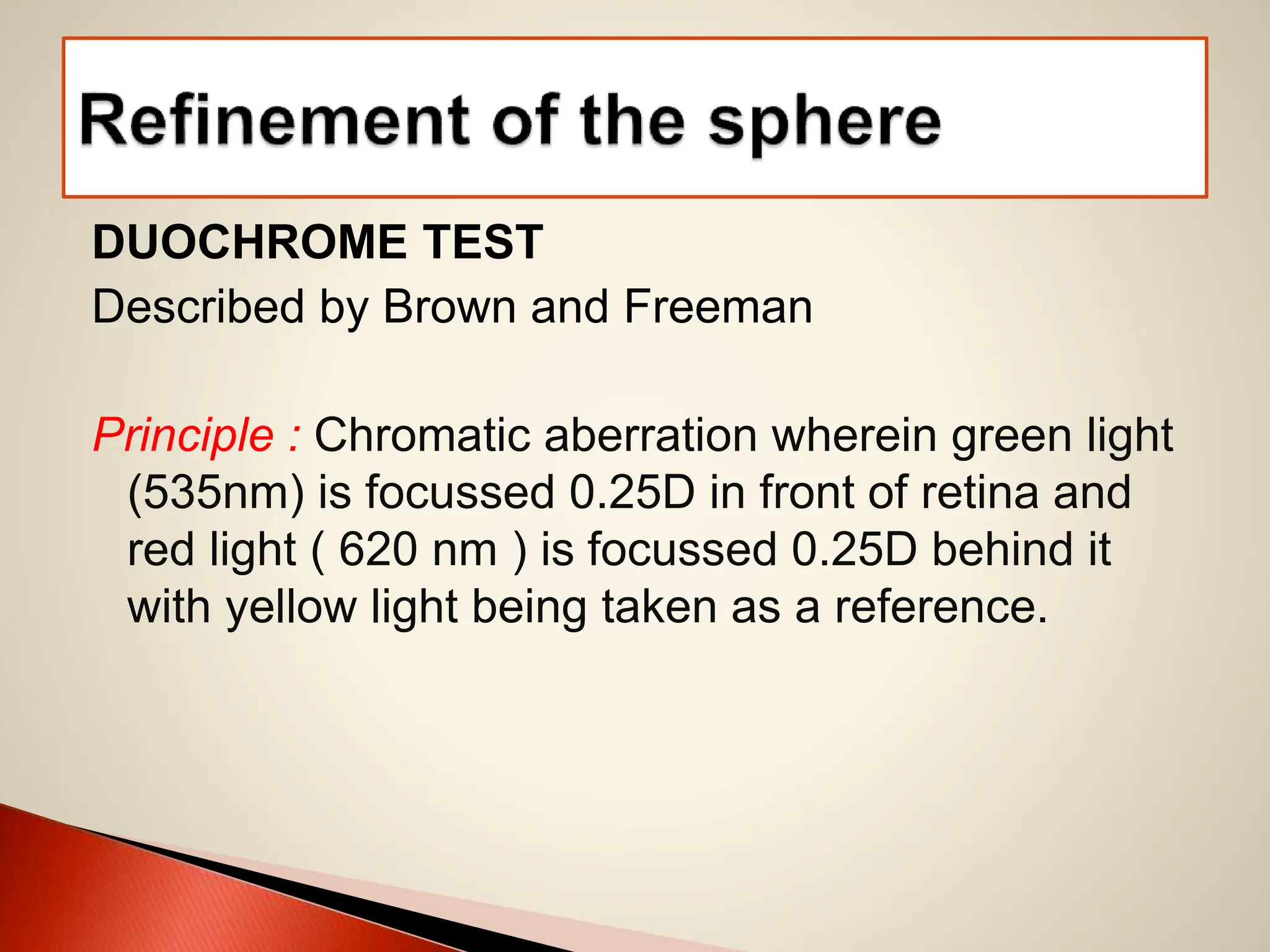
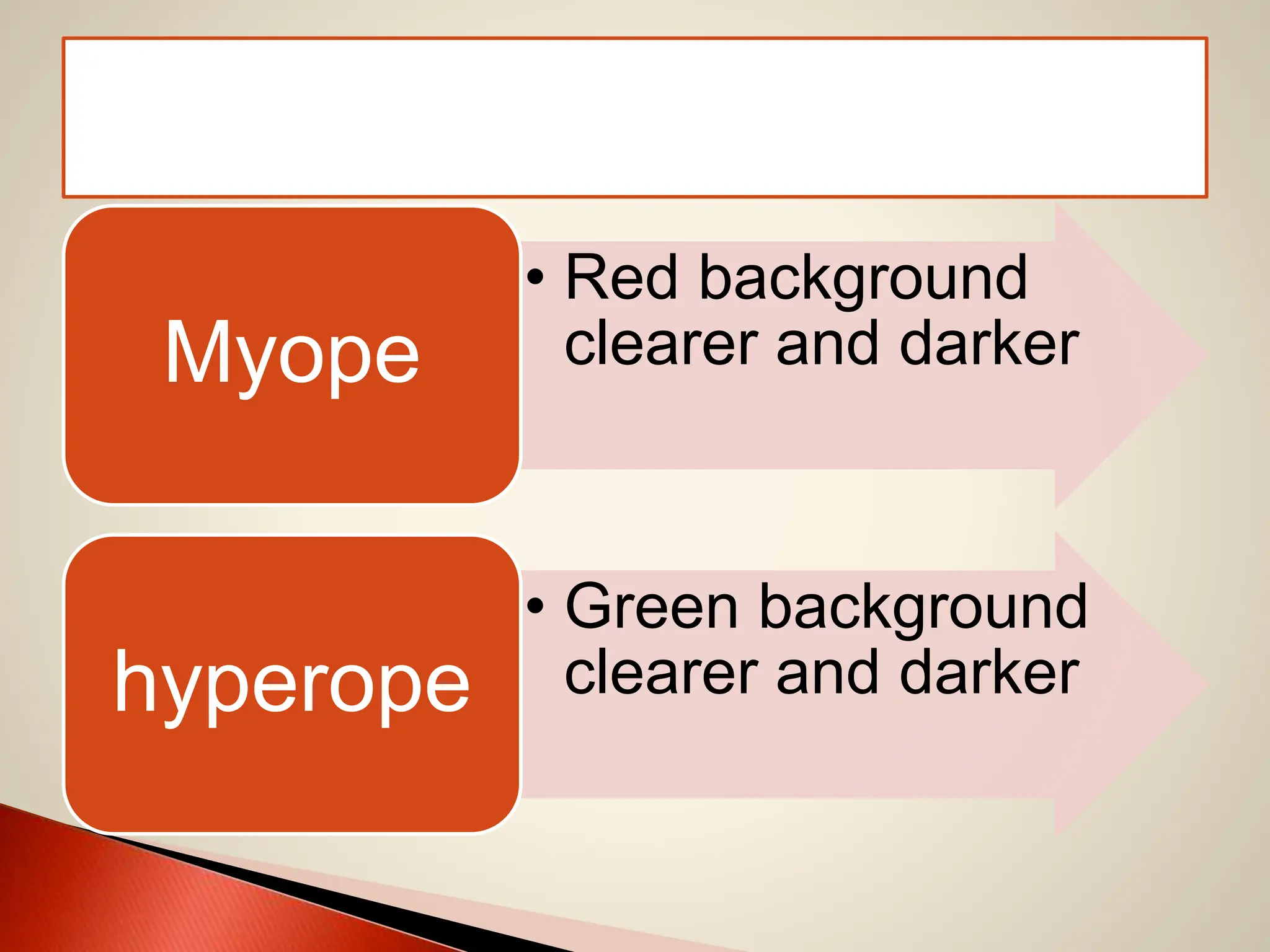
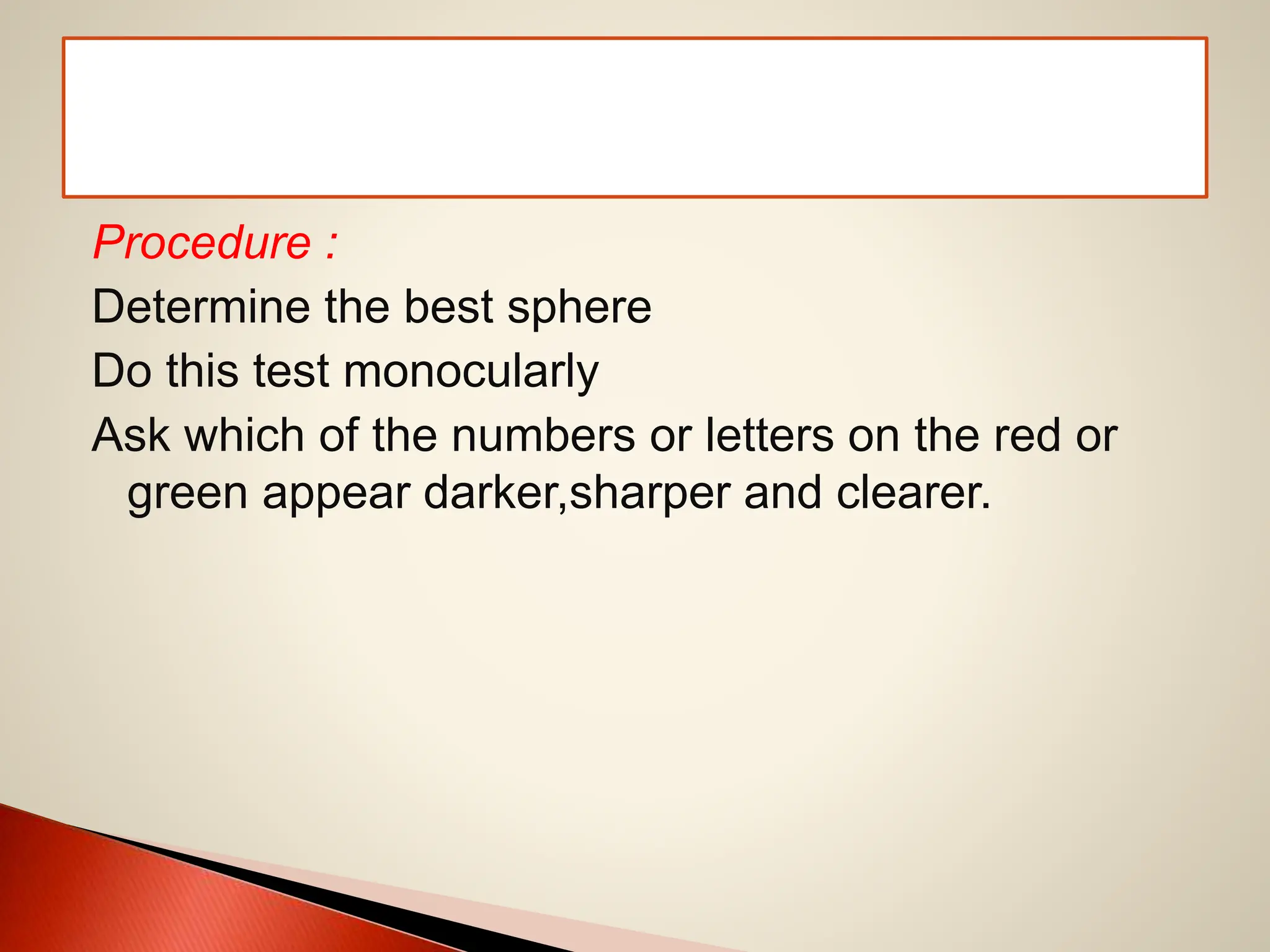
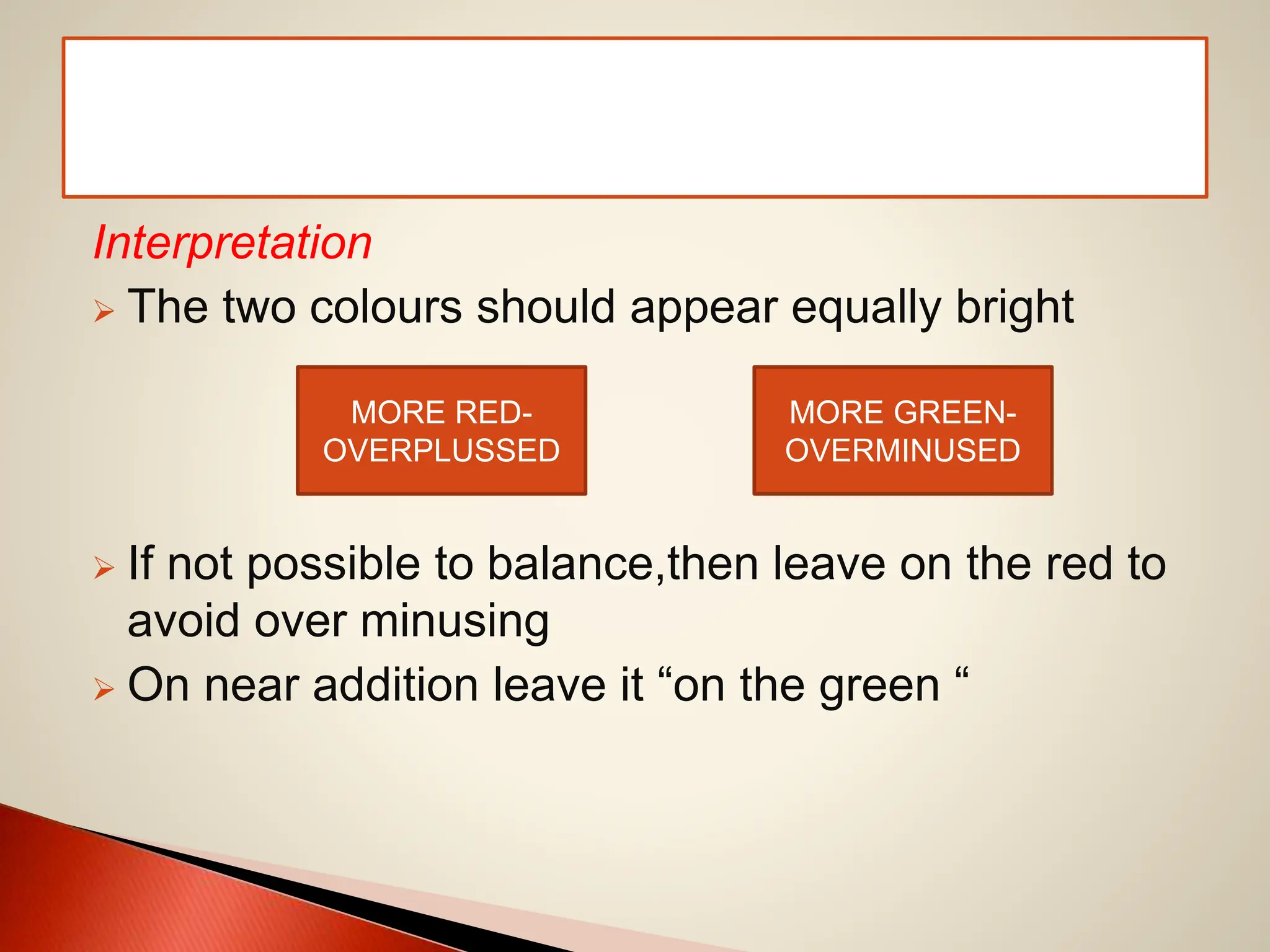
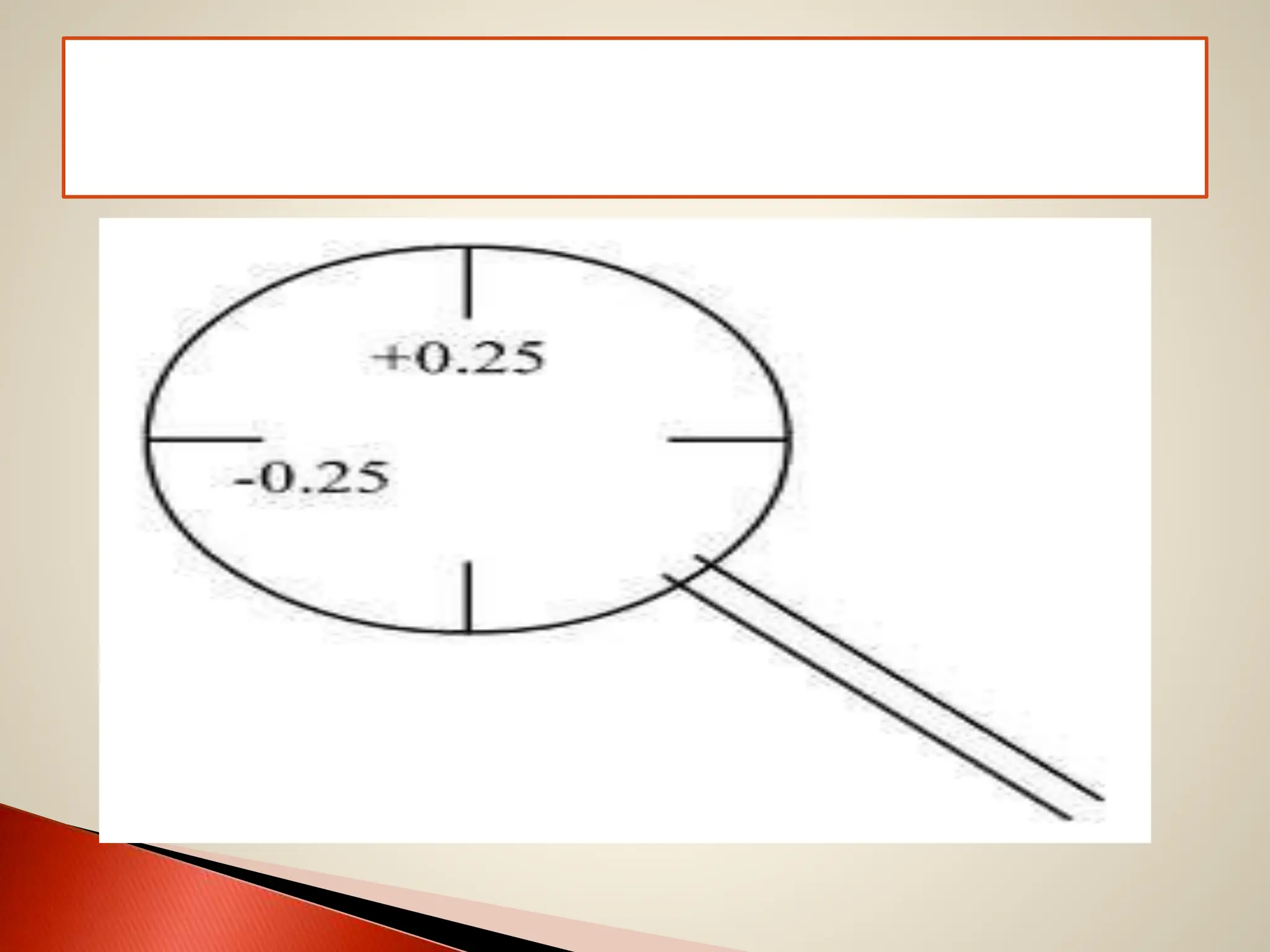
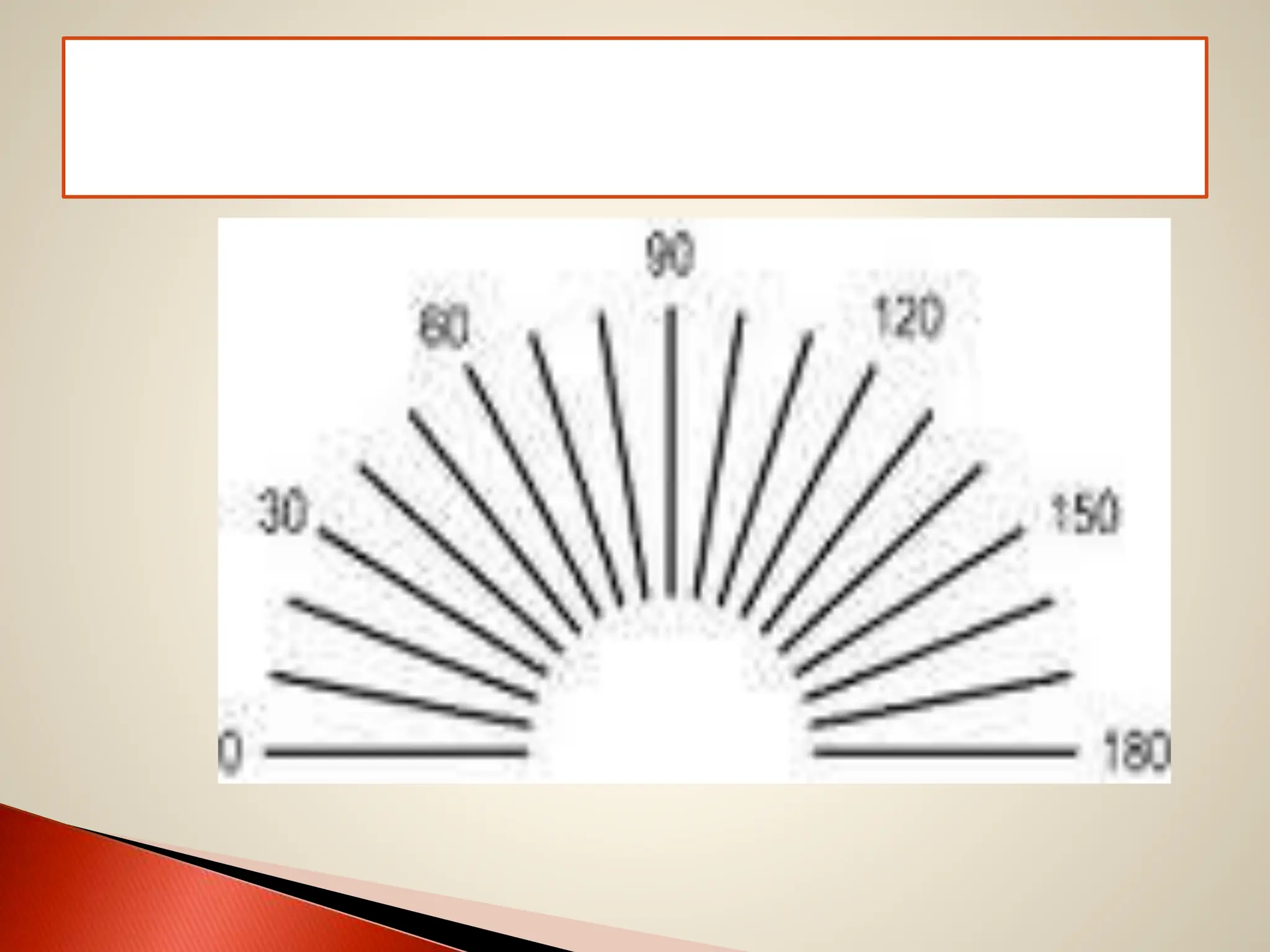
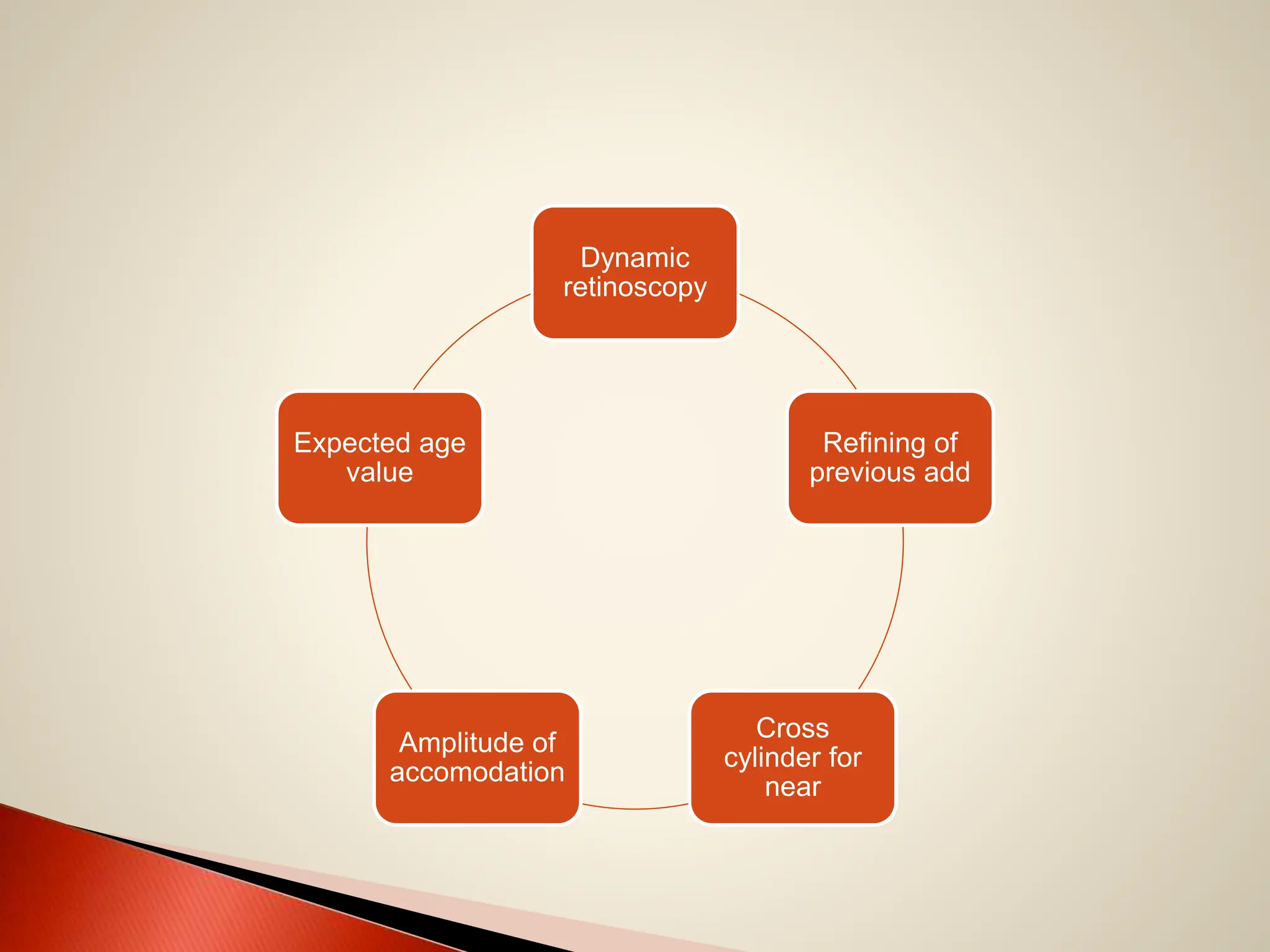
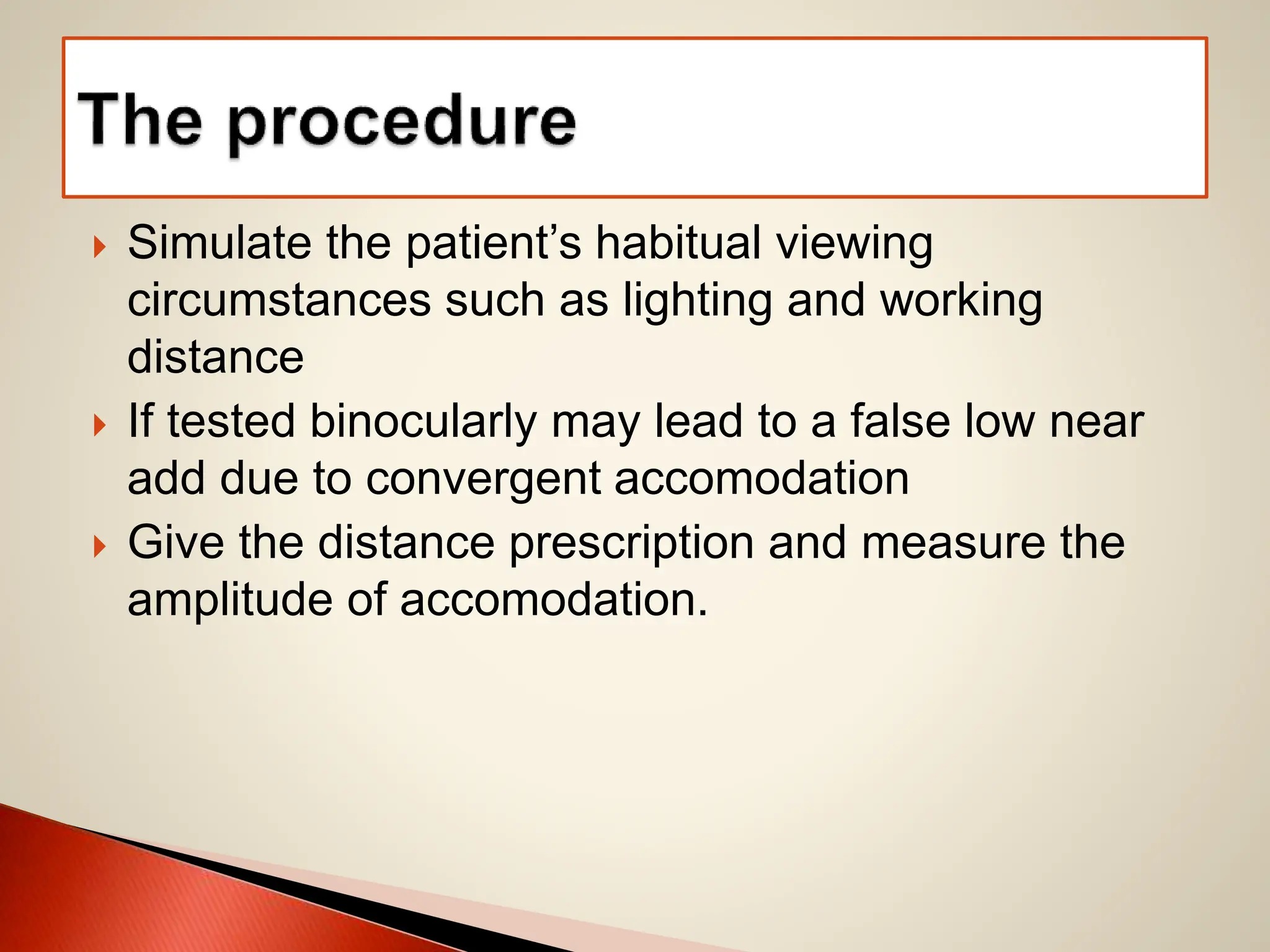
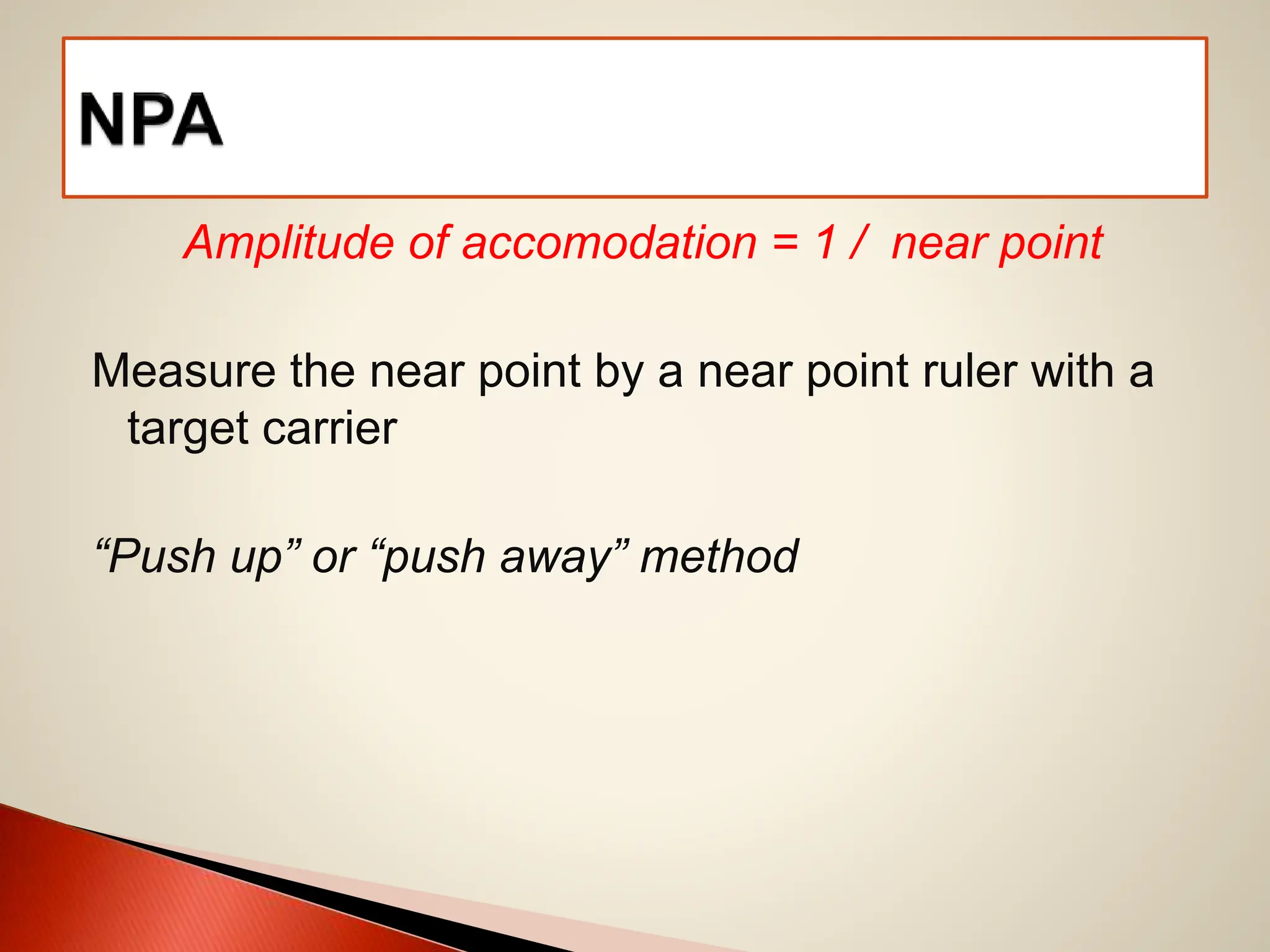
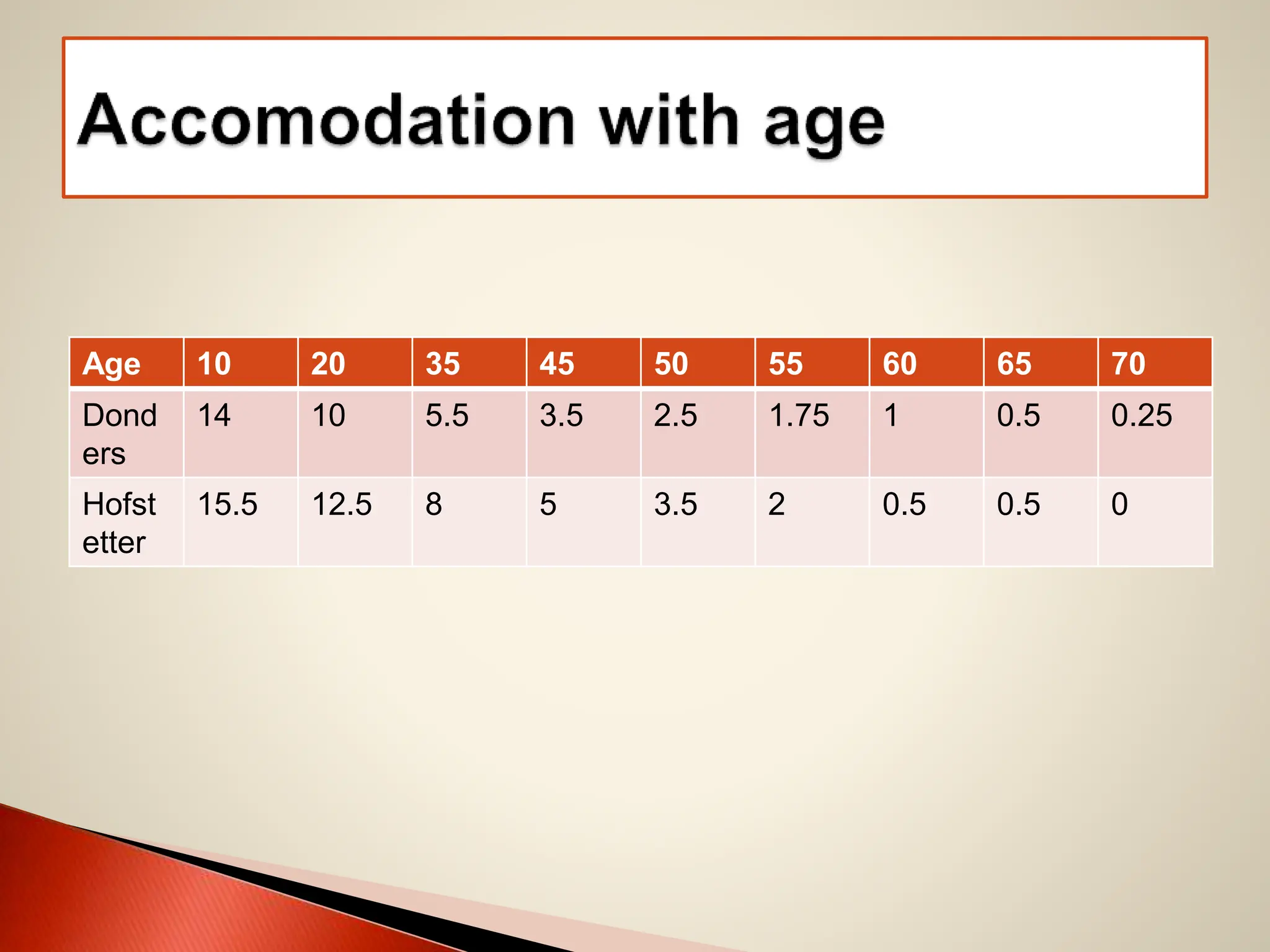
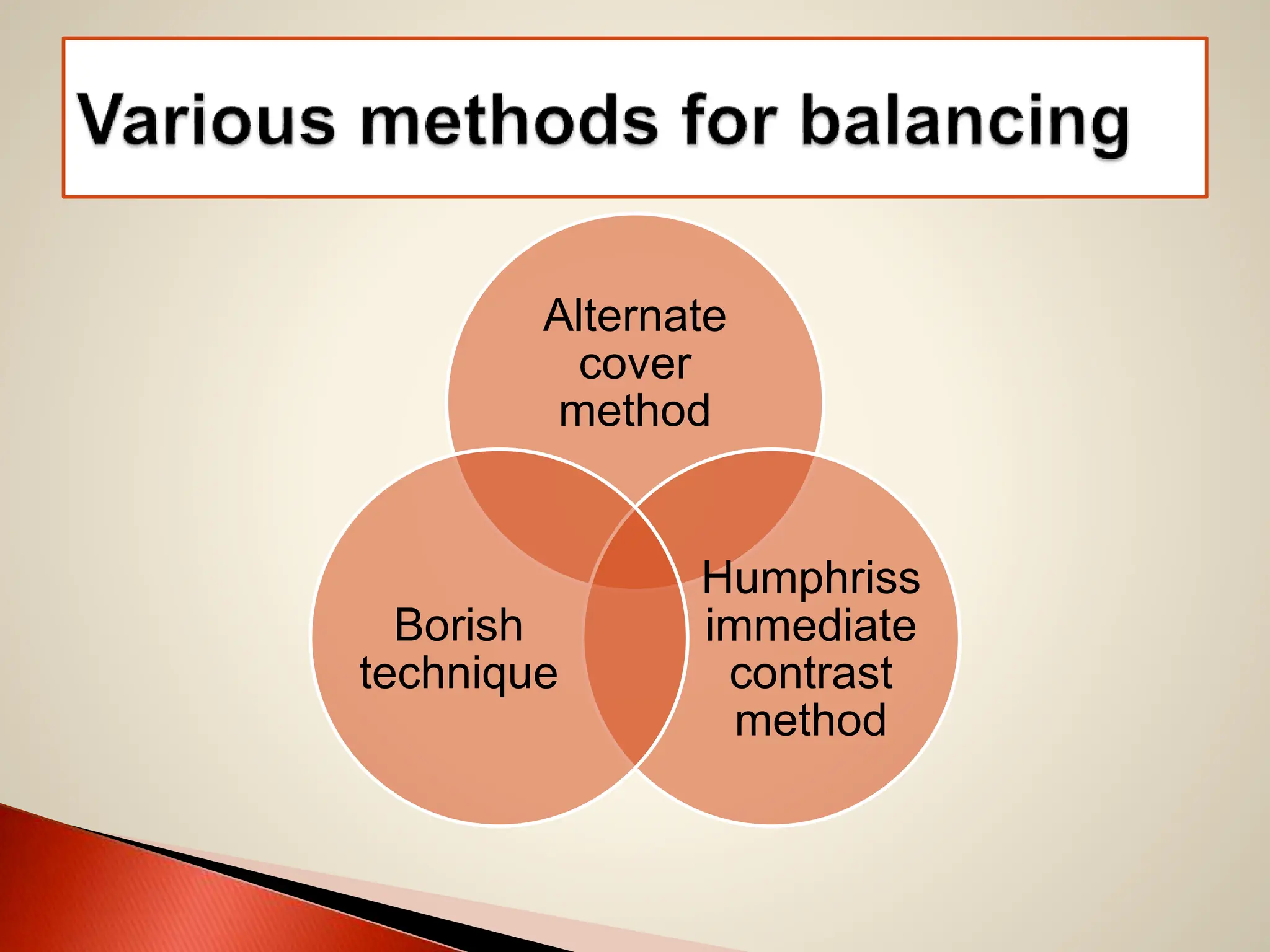
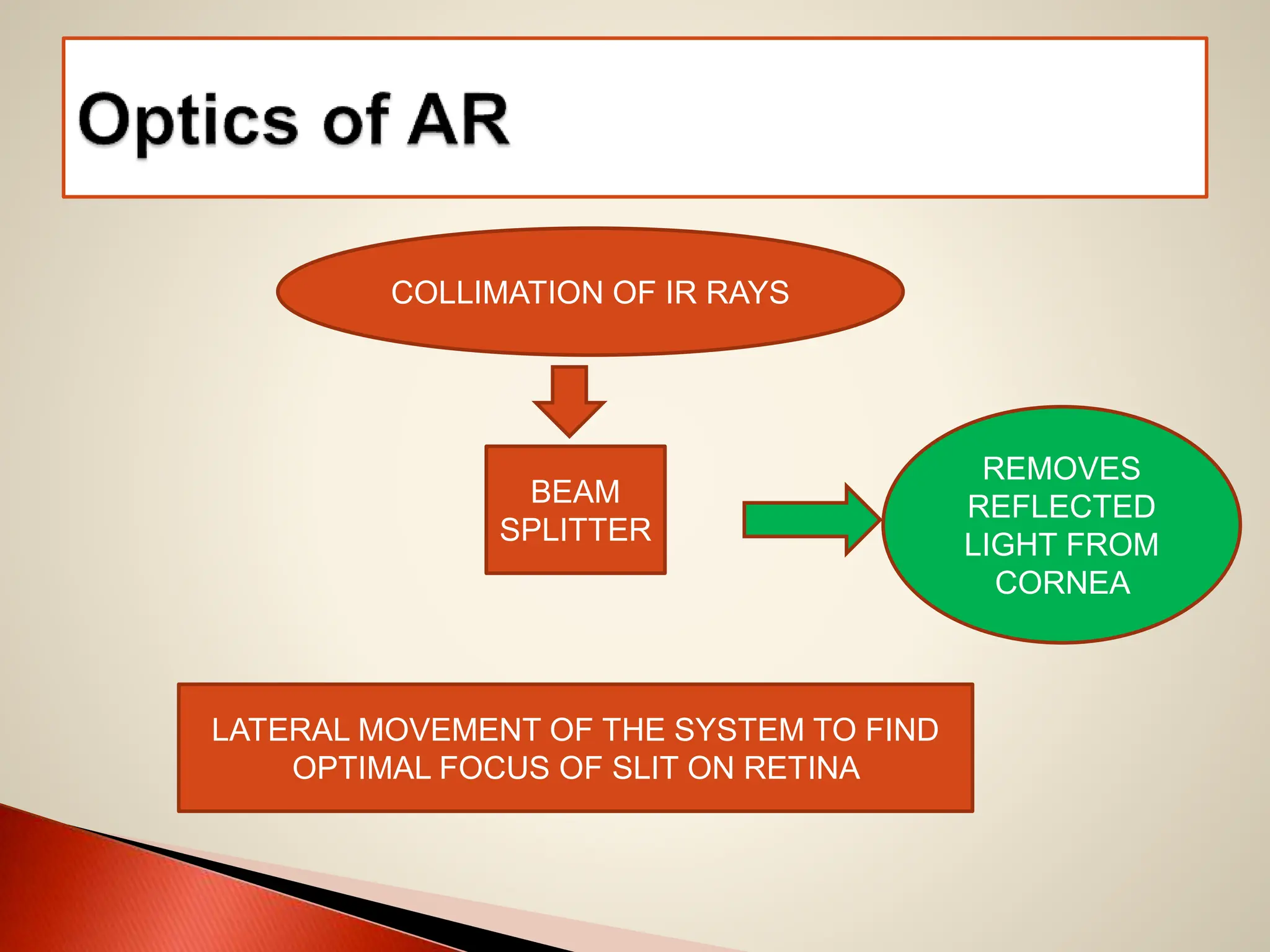
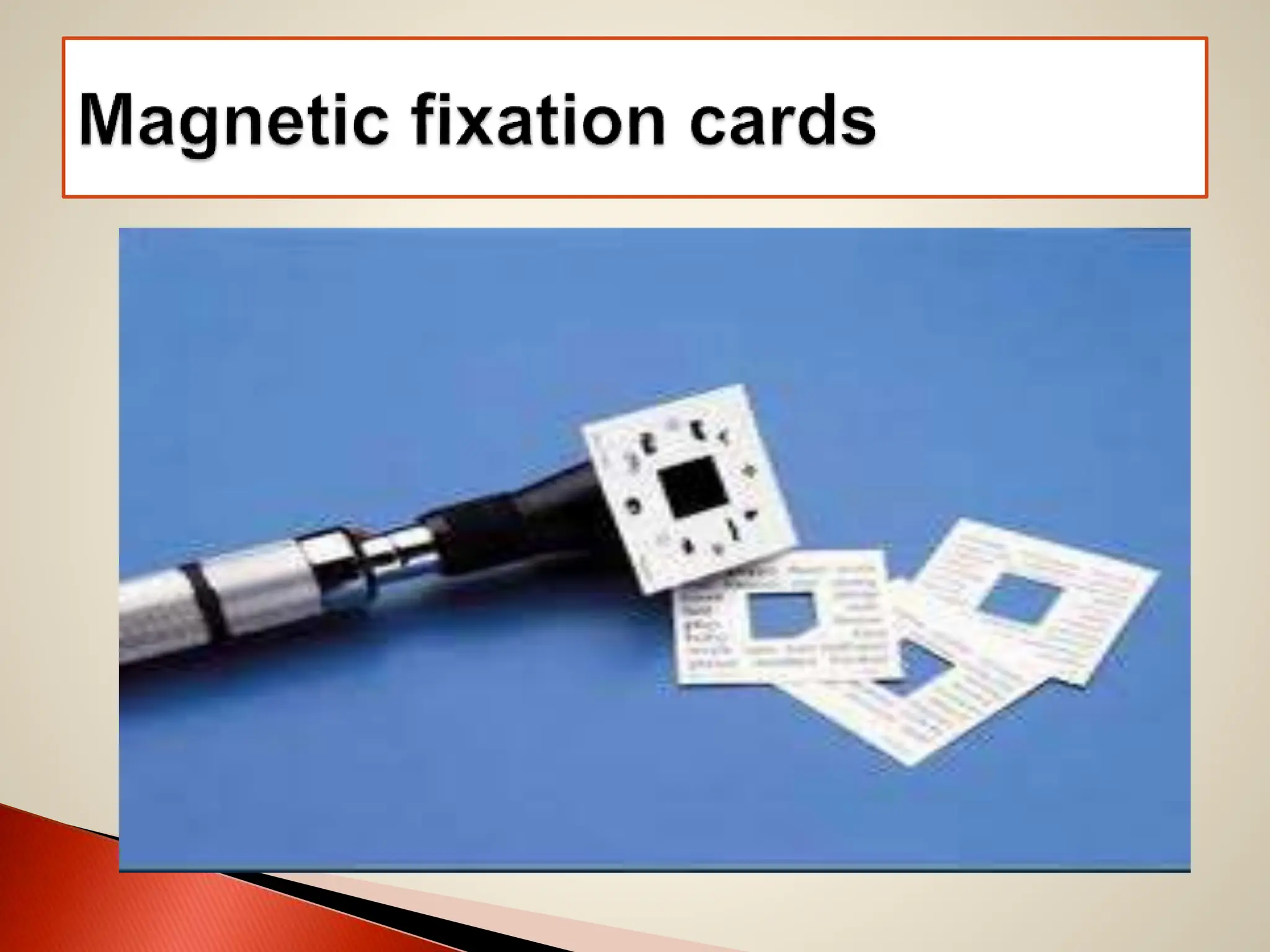
The document provides a comprehensive overview of retinoscopy, including its history, techniques, and equipment required for effective practice. Key sections cover objective and subjective retinoscopy methods, types of lenses used, and various tests like the duochrome test and Jackson cross cylinder for refining refraction. It also discusses the importance of accurately assessing and correcting refractive errors in patients, highlighting the relevance of both subjective and objective measurements in optometry.