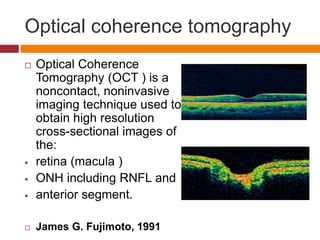
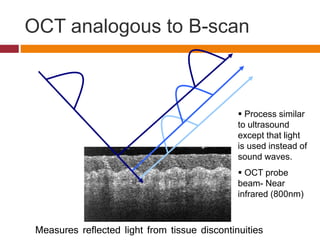
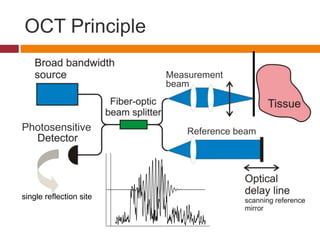
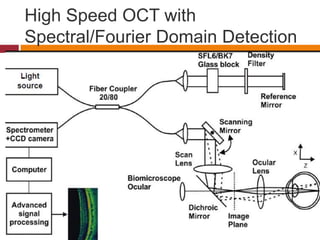
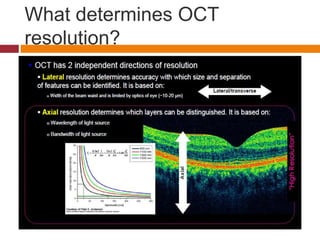
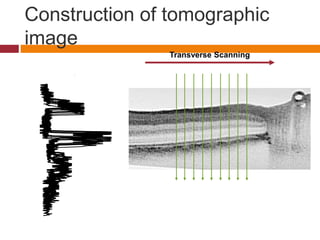
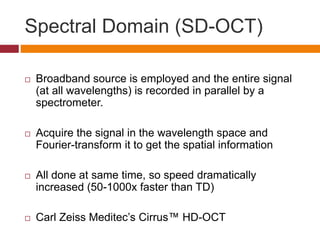
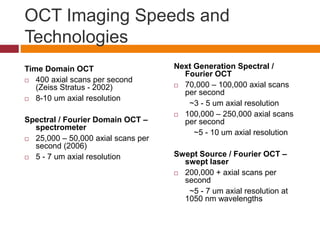
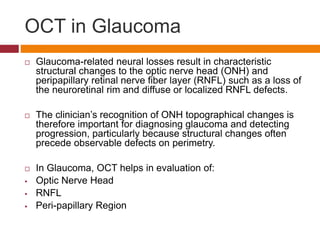
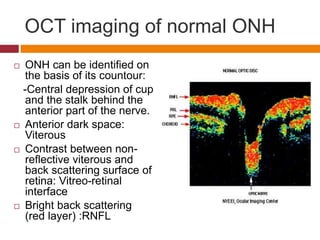
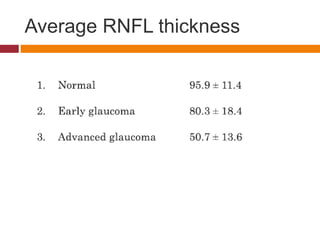
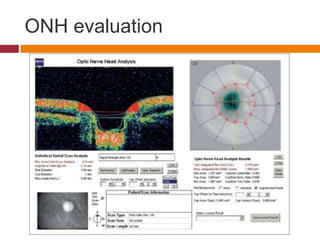
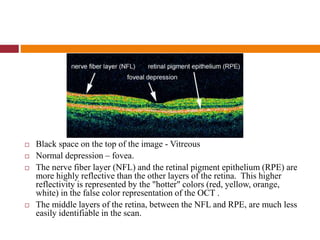
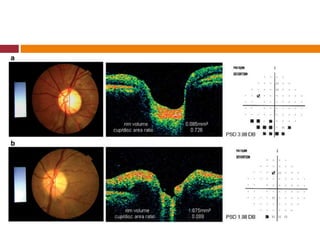
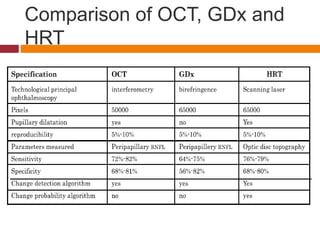
This document discusses optical coherence tomography (OCT) and its use in evaluating the optic nerve head (ONH). It provides details on OCT technology, including how OCT creates high resolution cross-sectional images of the retina and ONH using infrared light. The document compares time domain OCT and spectral domain OCT, and describes applications of OCT such as glaucoma evaluation by examining the ONH, retinal nerve fiber layer, and peripapillary region. Examples of OCT images of the normal ONH and glaucomatous ONH are also presented.