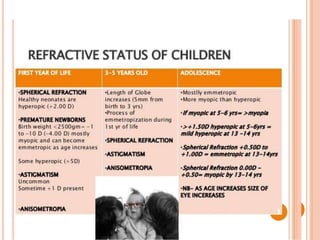
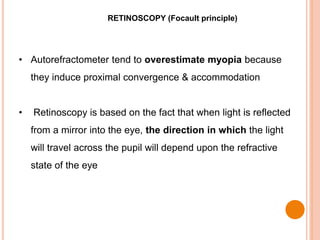
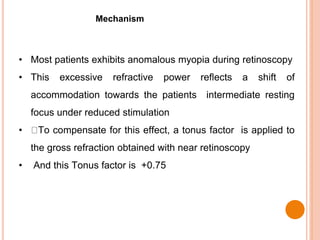
1. This document provides guidelines for prescribing glasses in children, including defining refractive errors, development aspects, and types of retinoscopy.
2. Key points include that cycloplegic refraction is mandatory in children to fully relax accommodation, and that significant refractive errors over ±4D or astigmatism over -1.5D are considered amblyogenic.
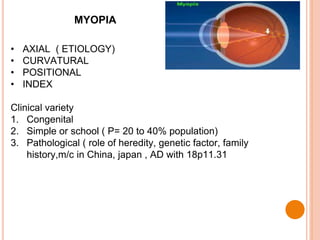
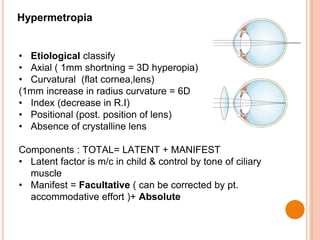
3. Guidelines specify that low hyperopia generally does not require correction unless esotropia is present, while moderate to high hyperopia and significant myopia should be fully corrected. The document outlines different approaches to managing myopia and hyperopia in children.