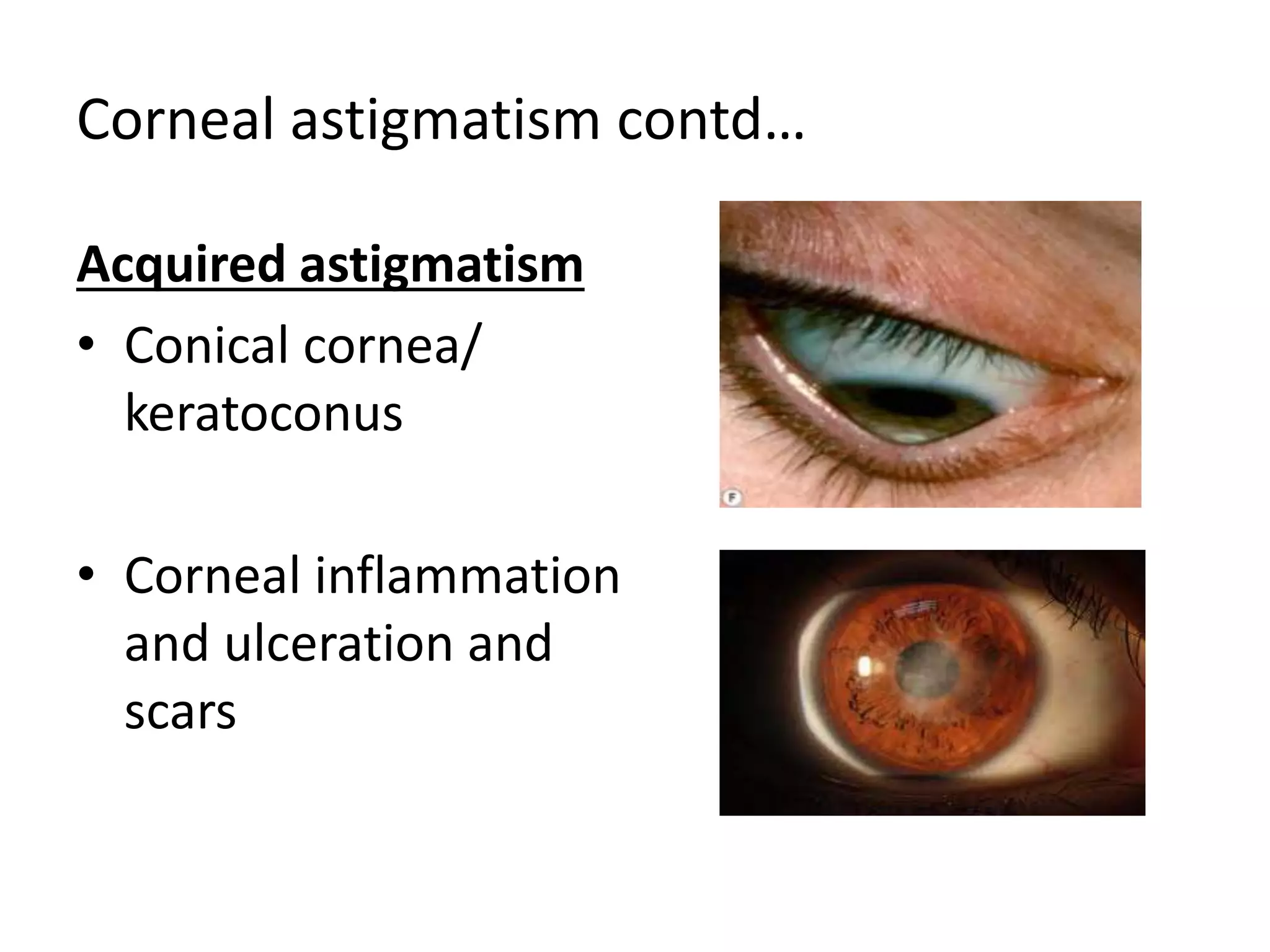
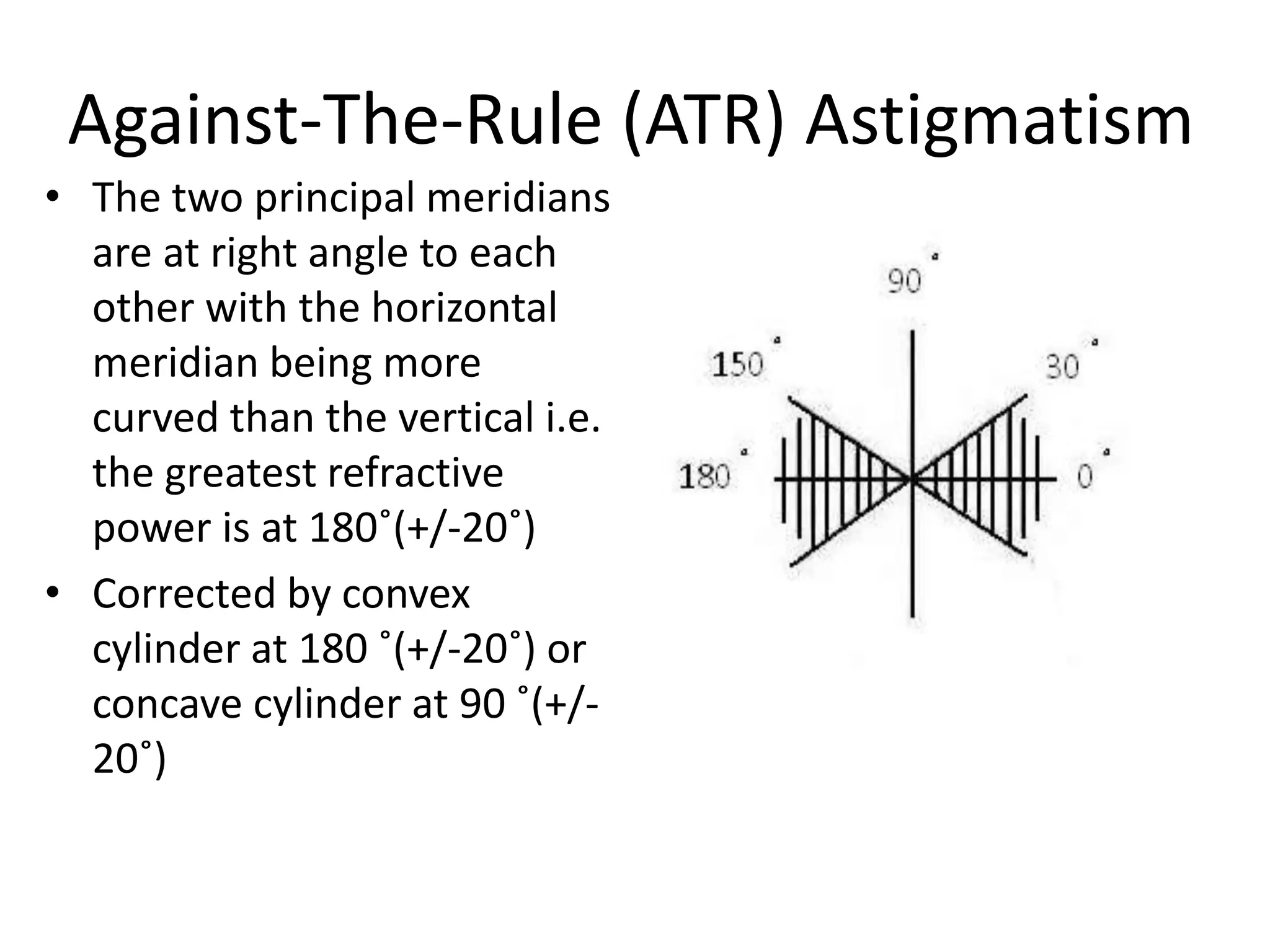
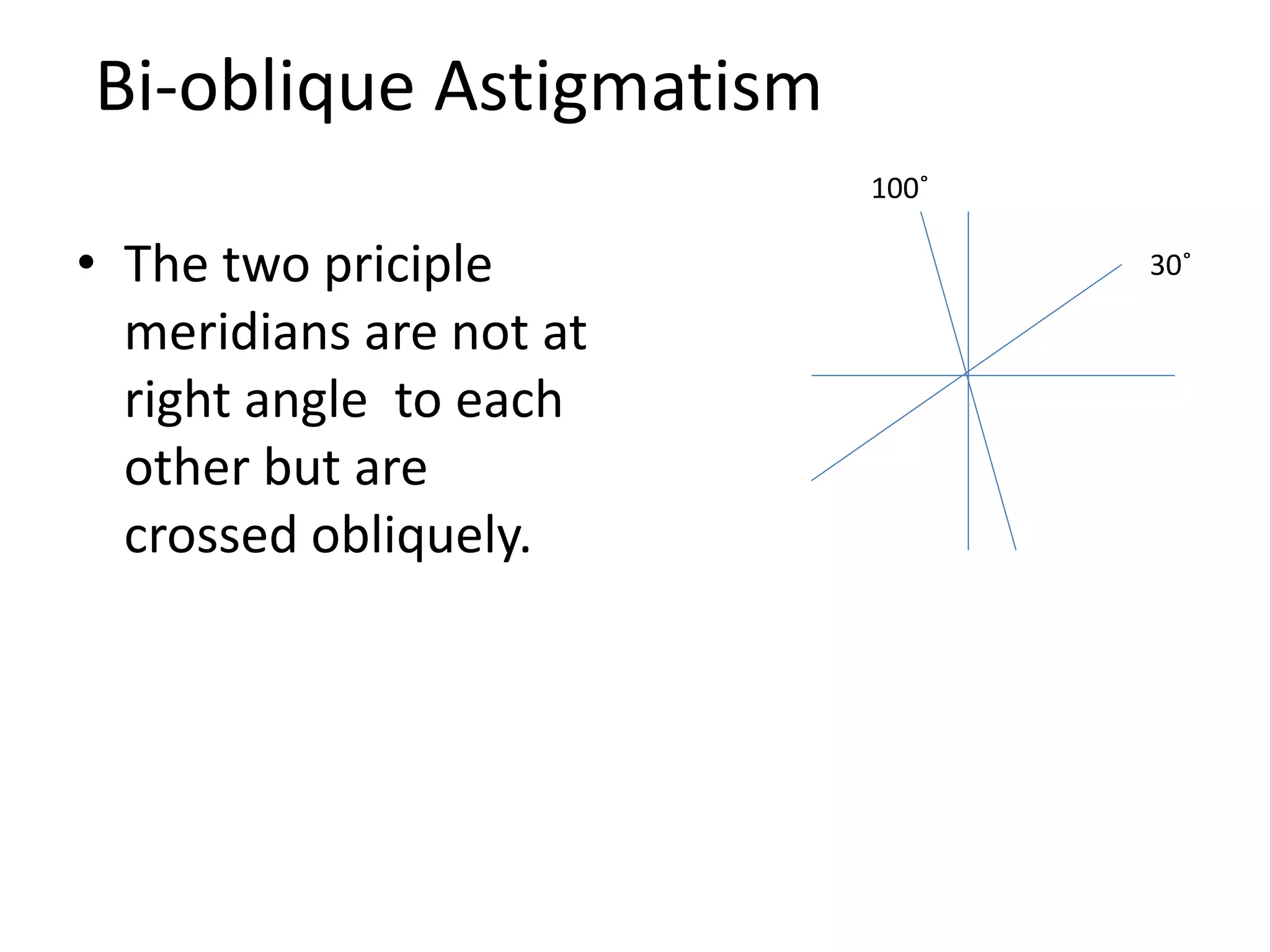
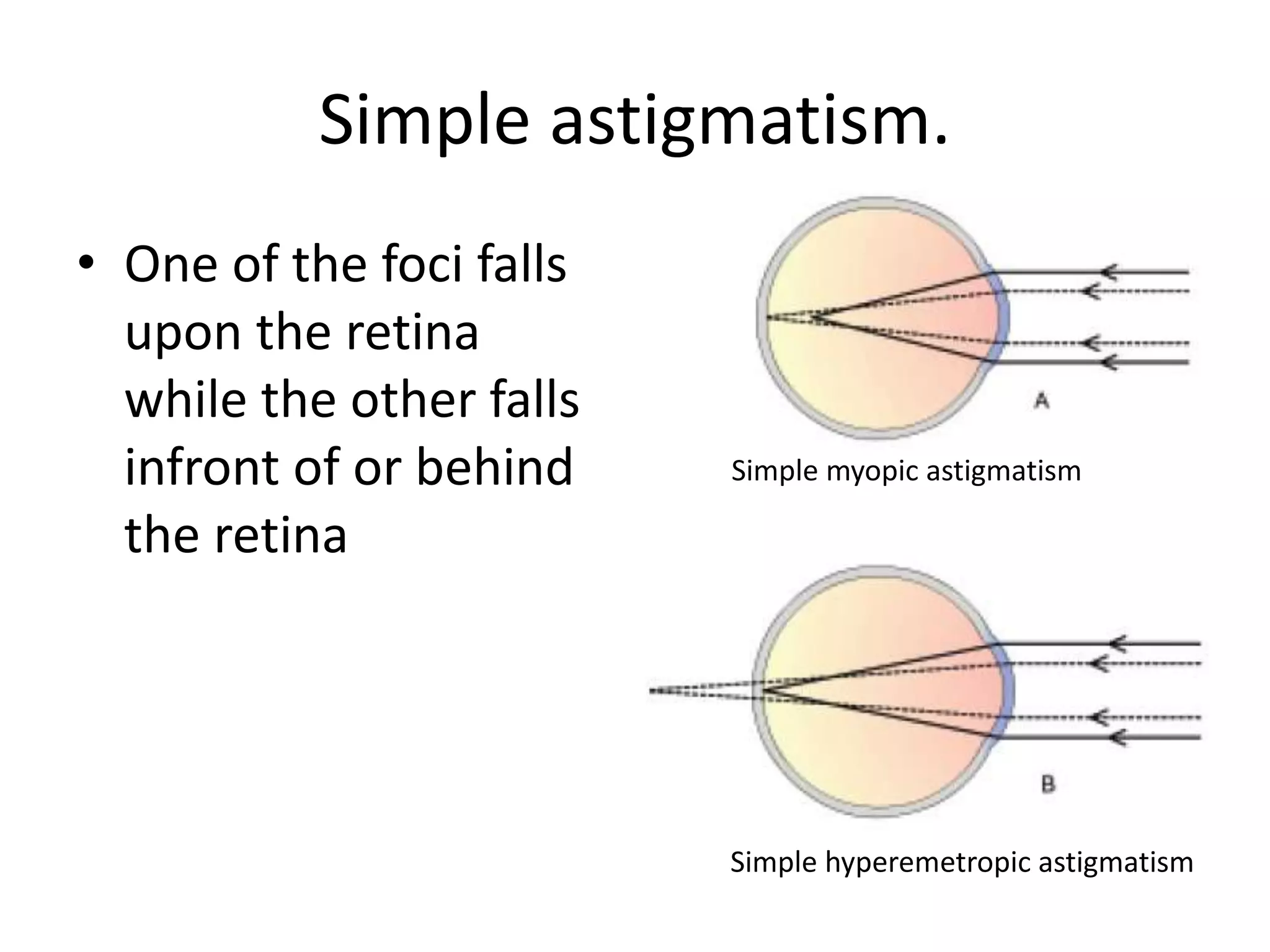
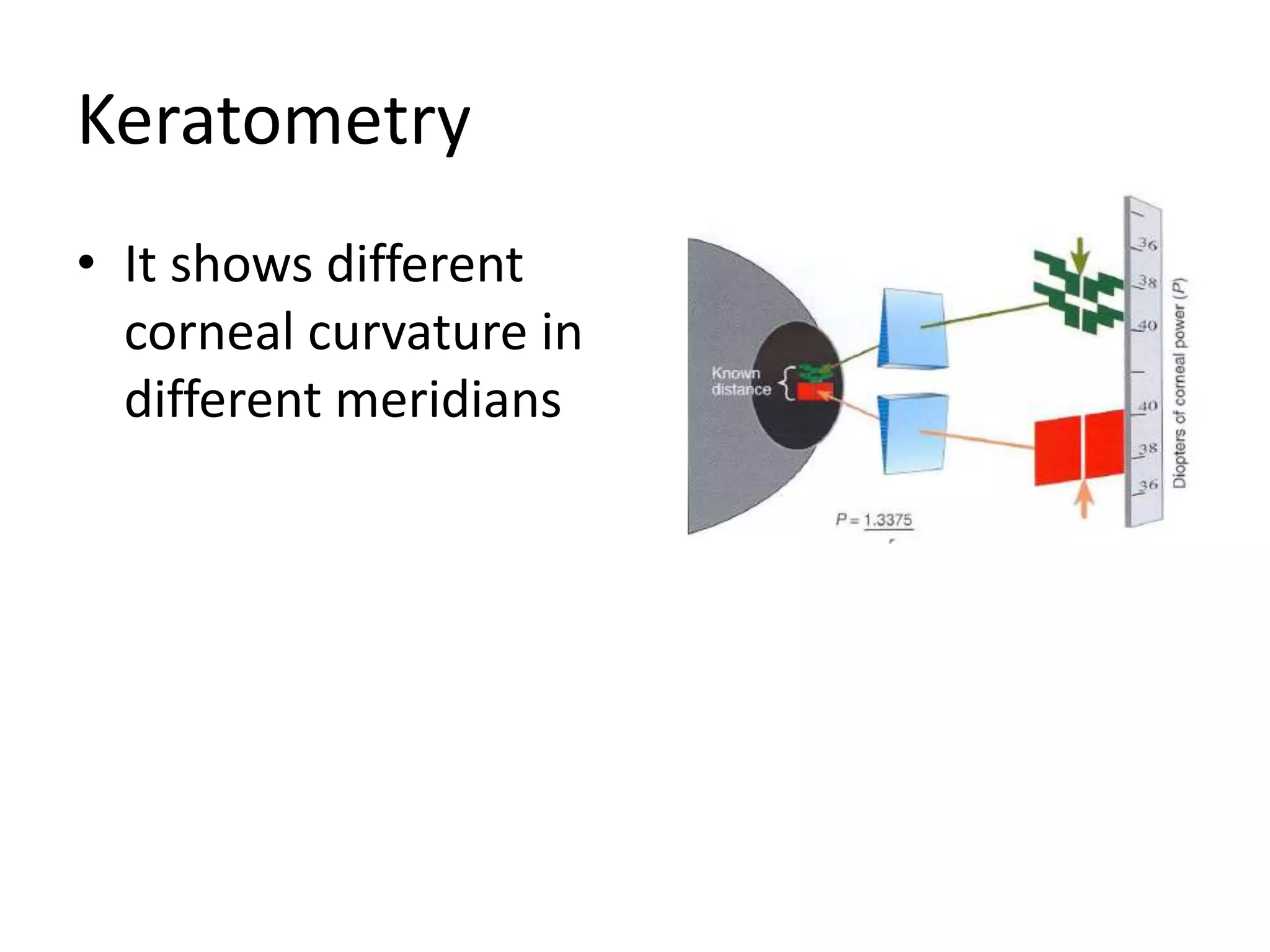
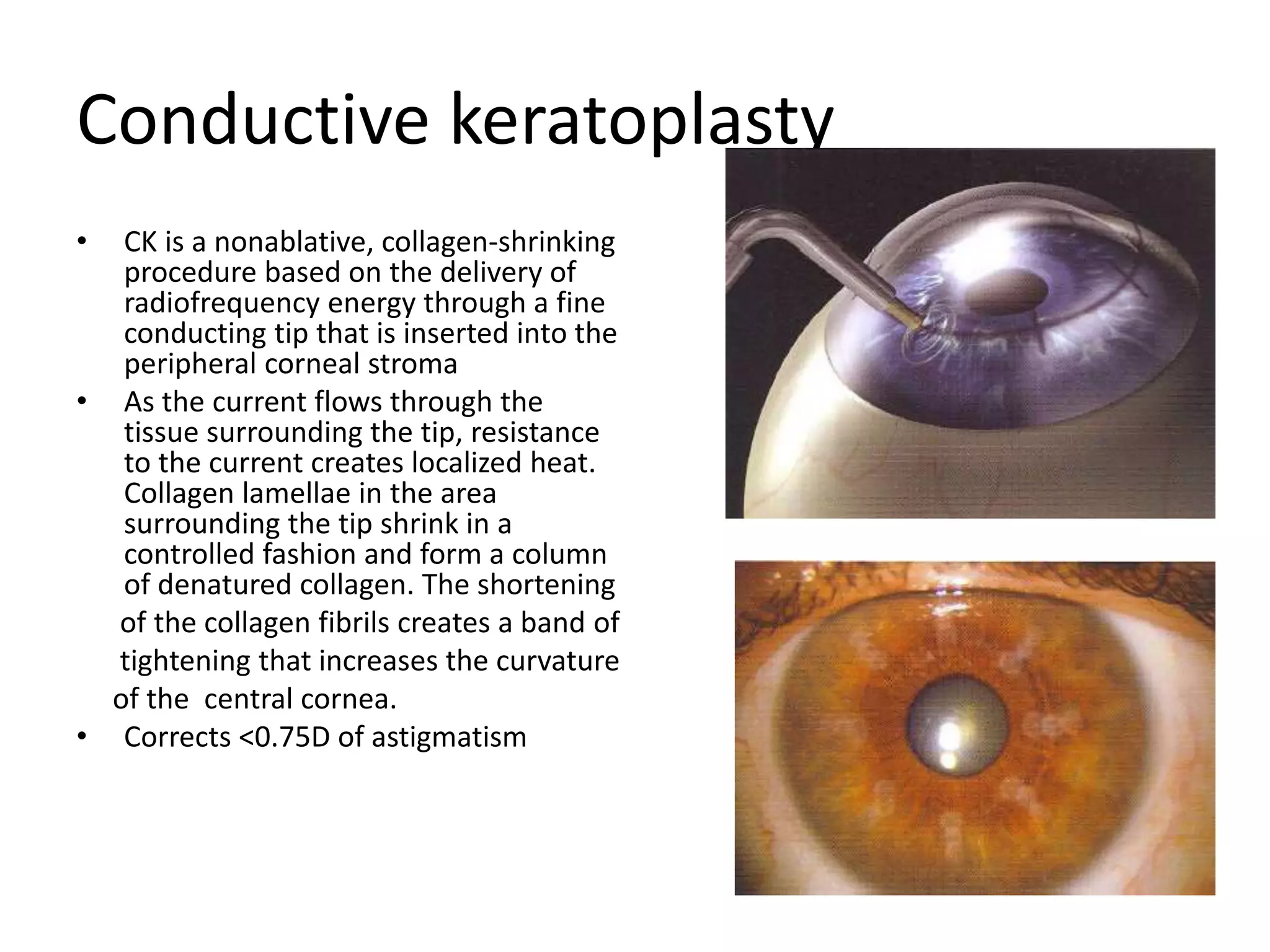
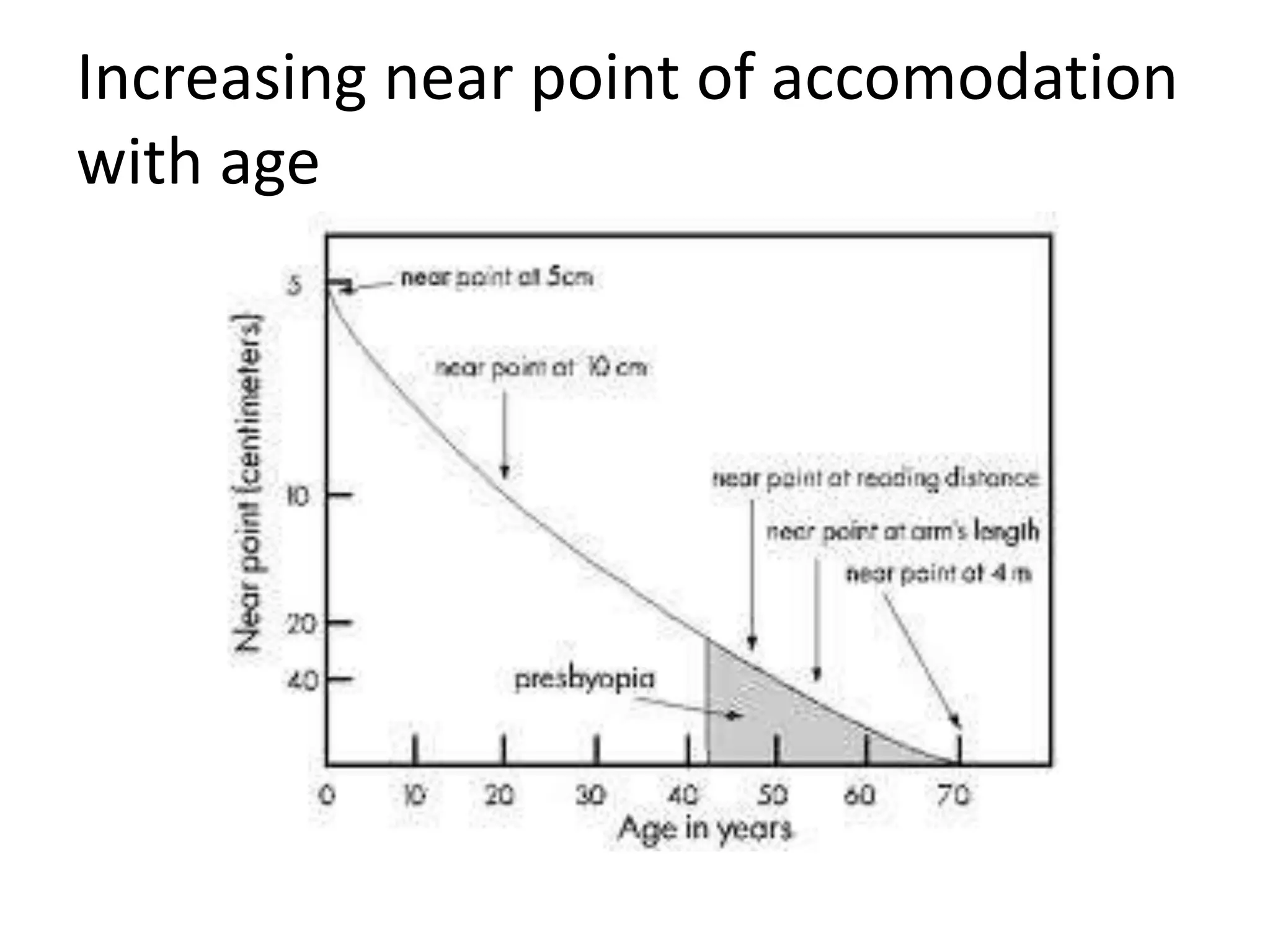
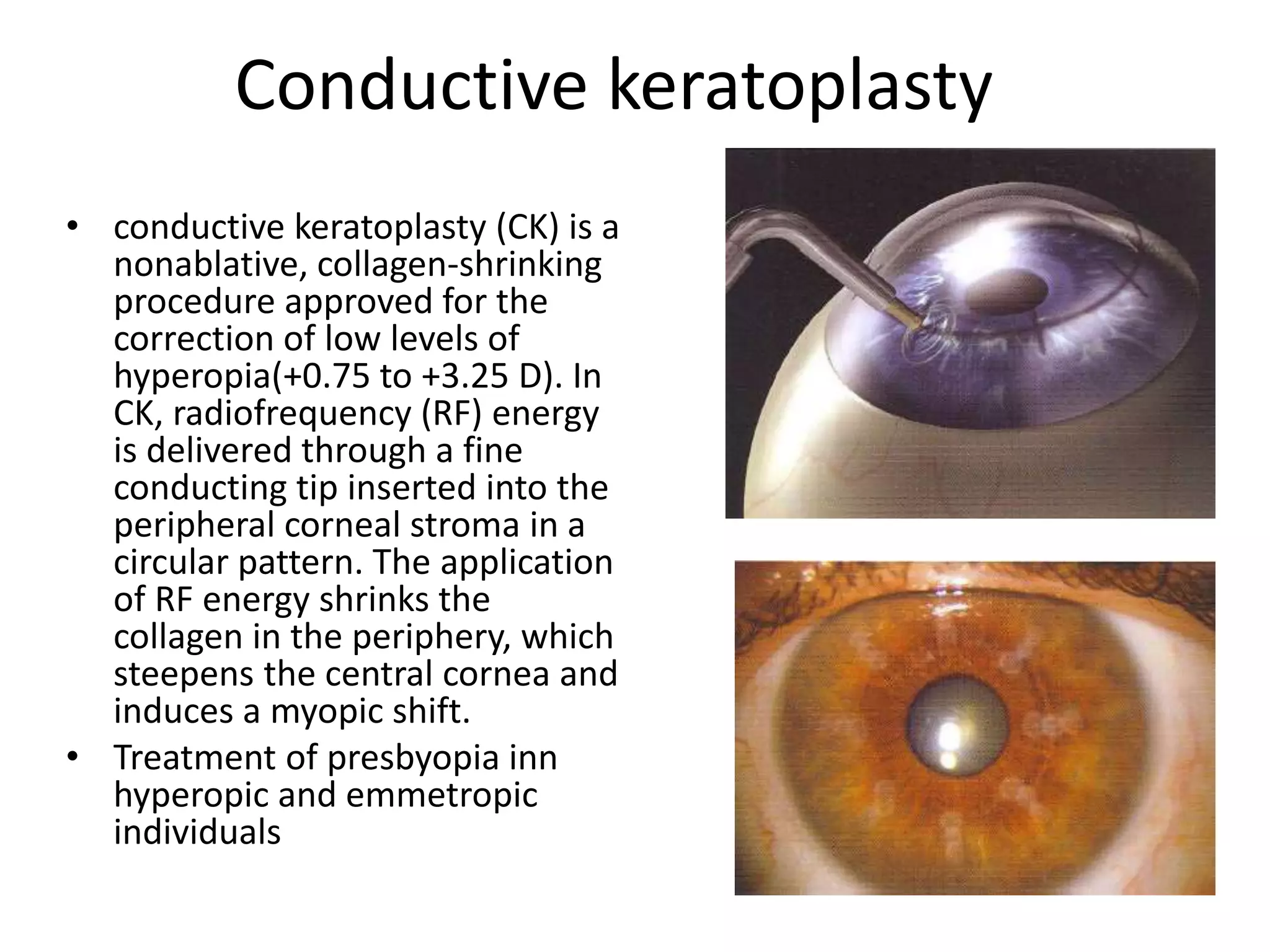
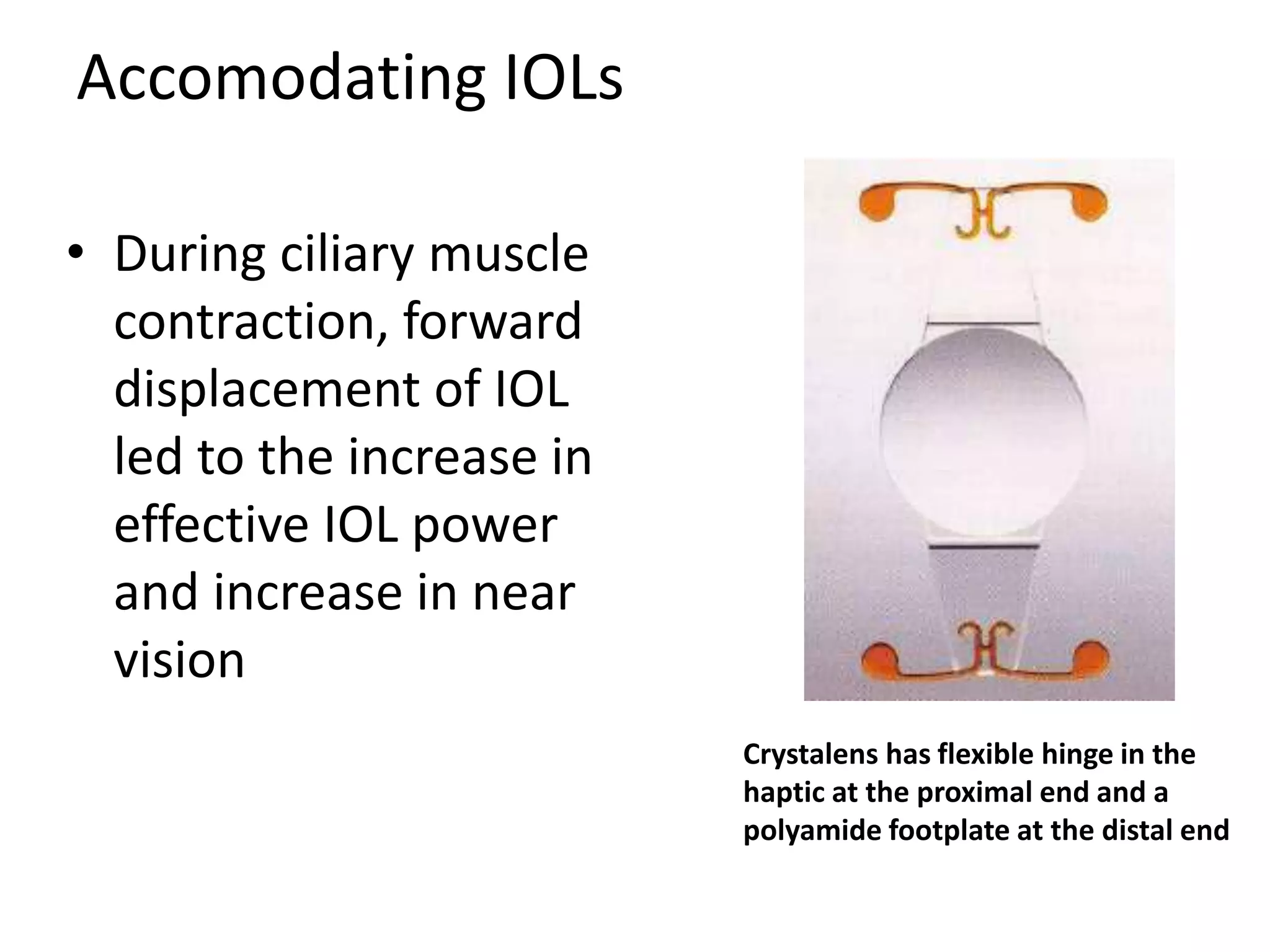
This document discusses astigmatism, presbyopia, and aphakia. It defines these conditions and describes their causes, symptoms, diagnosis, and treatment options. For astigmatism, it covers the different types including regular and irregular astigmatism. It discusses tests like keratometry and retinoscopy. Treatment includes optical correction with lenses, refractive surgery procedures, and intraocular lenses. For presbyopia, it defines the condition as age-related loss of accommodation. Symptoms and onset with age are described. Treatment involves optical correction with single vision, bifocal, or multifocal lenses as well as contact lenses and refractive surgery options.