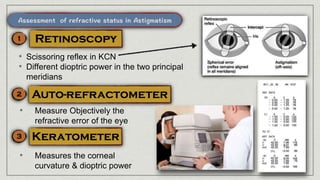
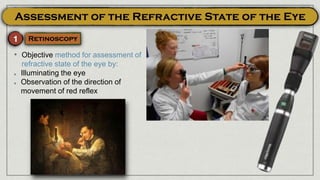
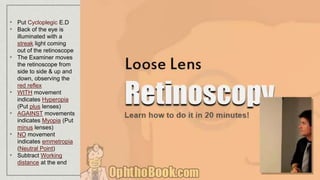
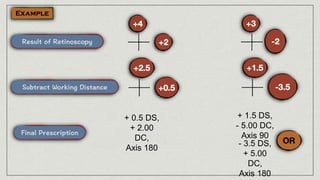
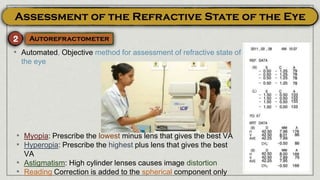
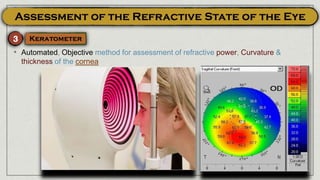
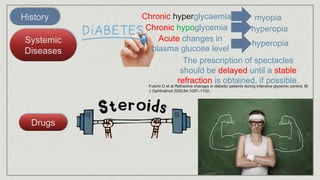
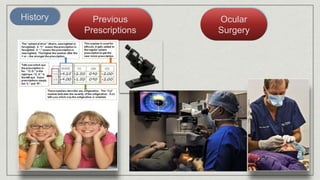
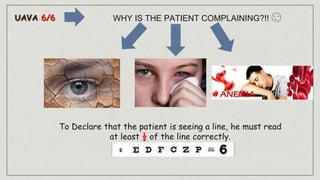
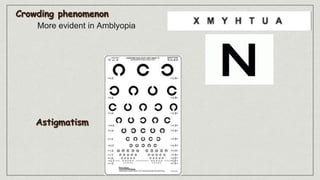
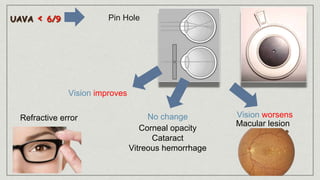
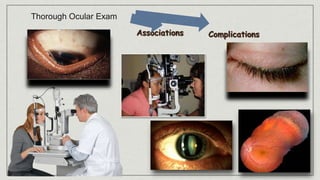
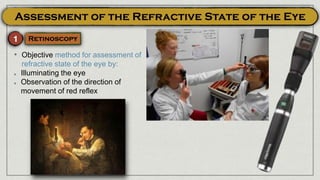
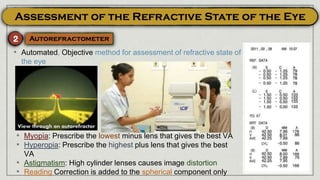
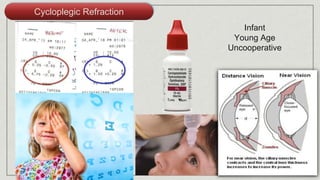
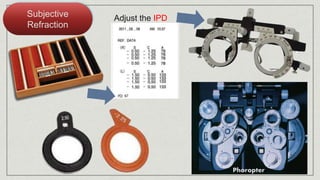
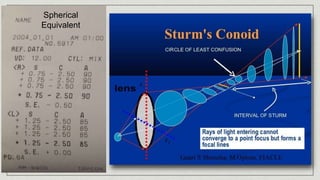
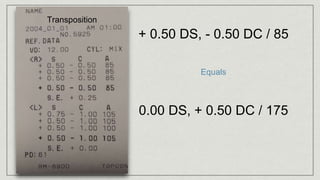
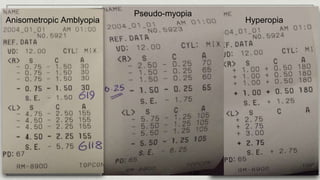
The document discusses assessment and correction of refractive errors. It provides information on objective refractive assessment tools like retinoscopy and autorefraction. It also discusses subjective refraction techniques and considerations for different patient types. Key points include using cycloplegic refraction for infants and uncooperative patients, adjusting IPD with the phoropter, and transposing cylinders to determine the spherical equivalent.