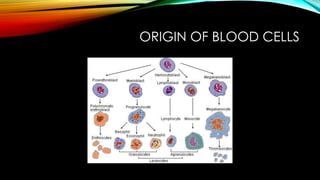
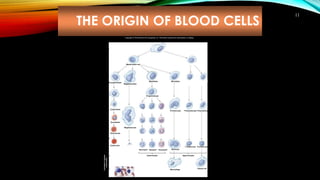
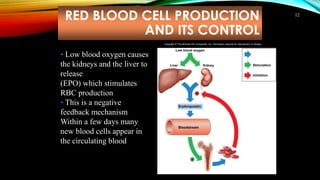
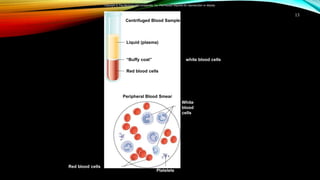
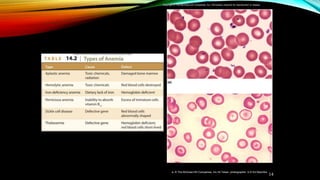
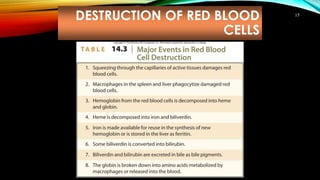
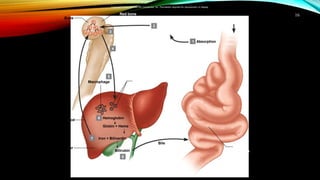
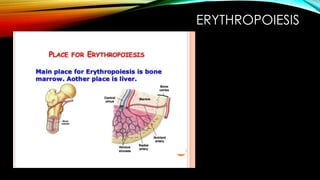
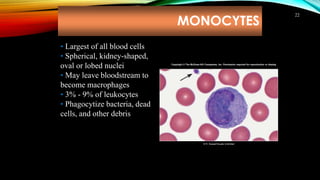
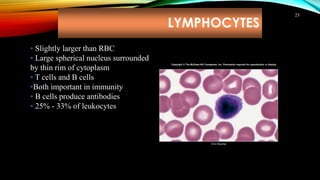
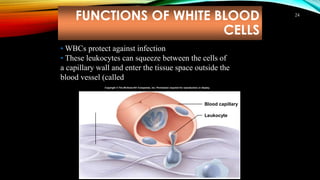
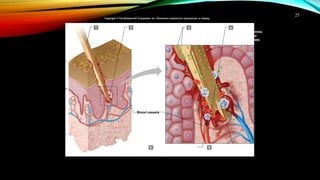
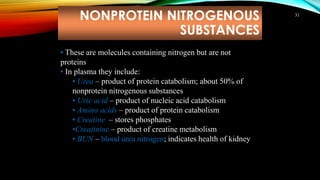
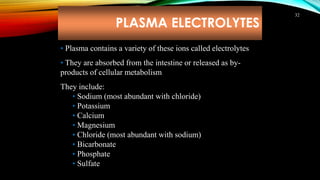
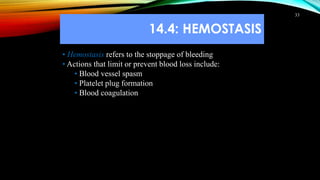
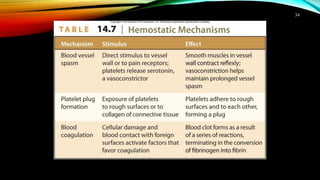
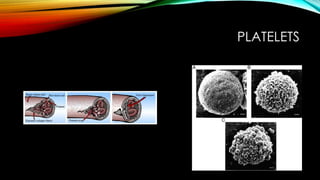
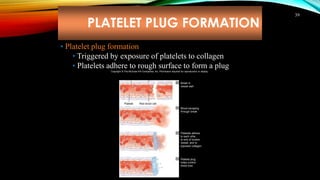
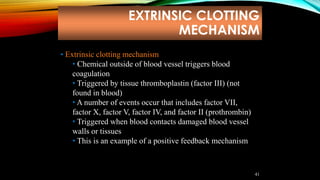
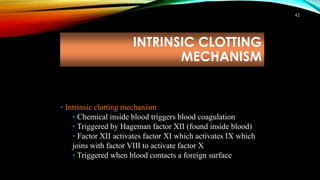
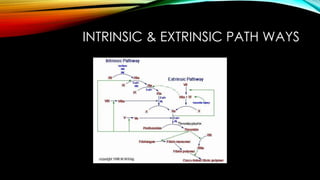
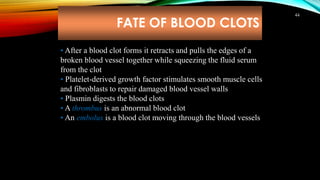
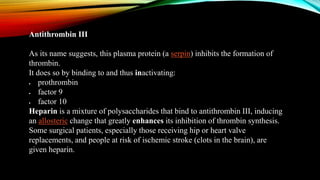
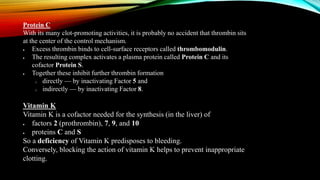
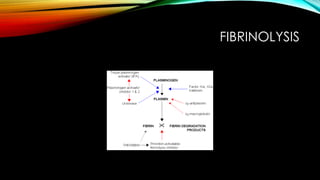
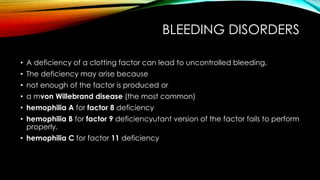
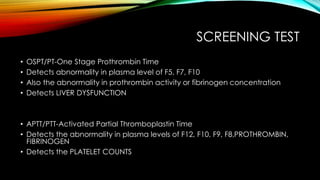
The document discusses the cardiovascular system, including its major components and functions. It describes the three main divisions of the cardiovascular system: the distribution system, perfusion system, and collecting system. It also discusses the origin and types of blood cells, the mechanisms of circulation and hemostasis, the coagulation cascade, and common screening tests used to detect abnormalities.