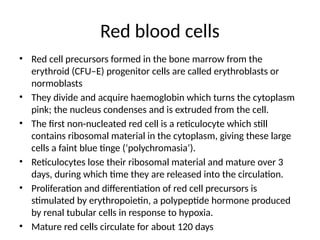
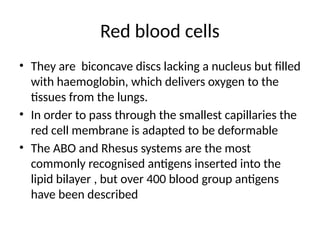
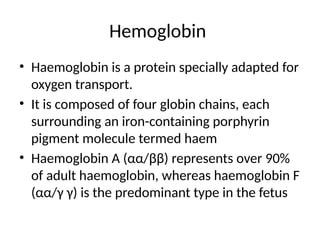
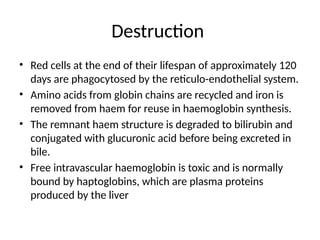
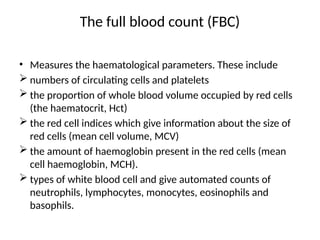
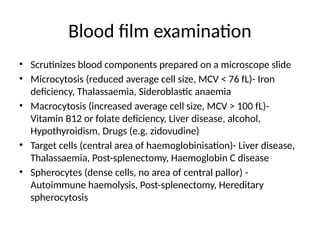
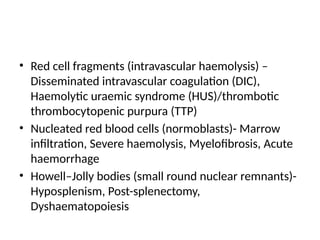
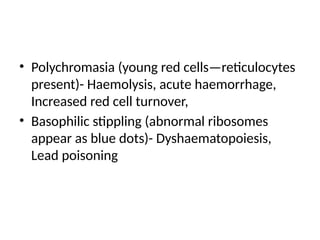
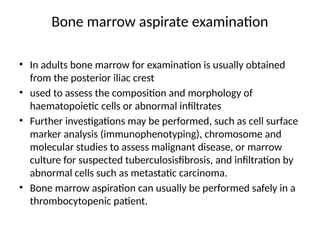
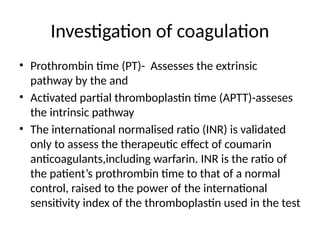
This document explores the structure and function of blood, detailing components like red blood cells, white blood cells, and platelets, as well as their formation and destruction. It highlights key processes including hematopoiesis, hemostasis, and the examination of blood and bone marrow for diagnostic purposes. The document also discusses blood pathology and various aspects of physical examination and laboratory investigations related to hematological health.