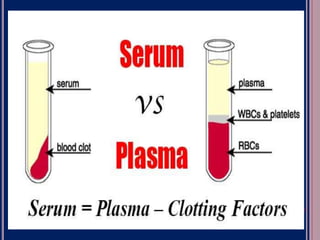
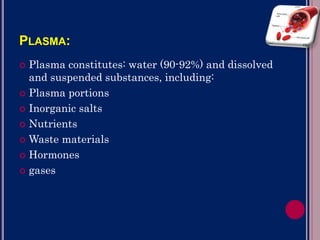
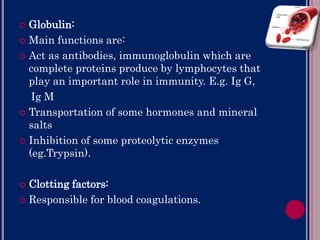
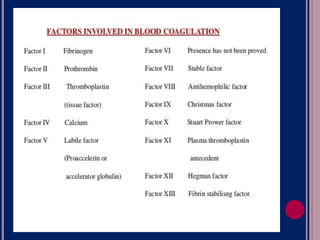
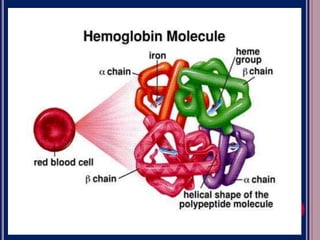
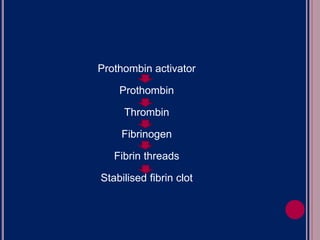
Blood is composed of plasma and blood cells suspended in plasma. Plasma is mostly water but also contains proteins, electrolytes, nutrients, waste products, hormones and gases. The three main types of blood cells are red blood cells, white blood cells, and platelets. Red blood cells contain hemoglobin and transport oxygen and carbon dioxide. White blood cells help fight infection. Platelets help with blood clotting to stop bleeding. Transfusions require matching blood types to avoid rejection reactions from antibodies in the plasma.