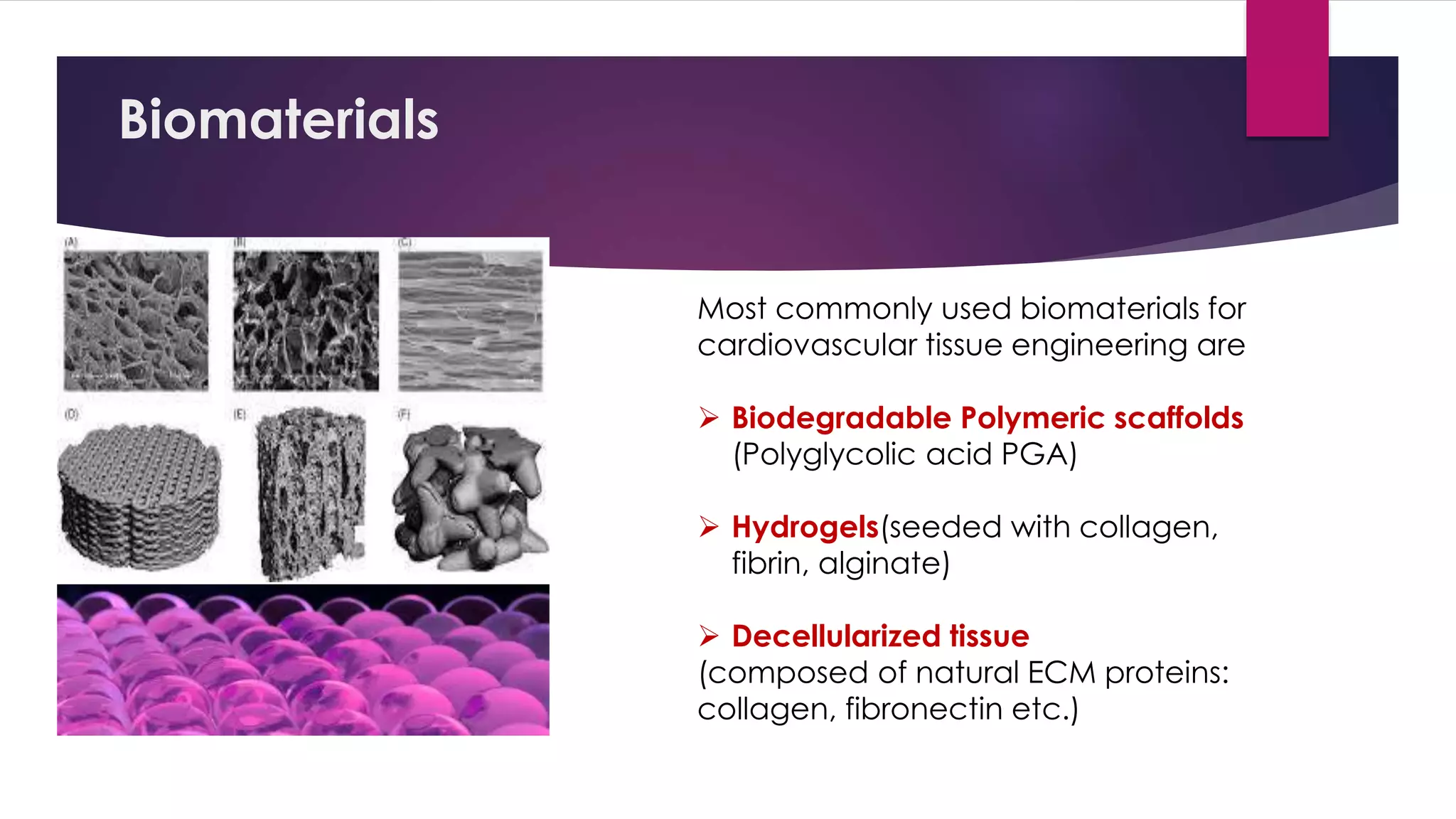
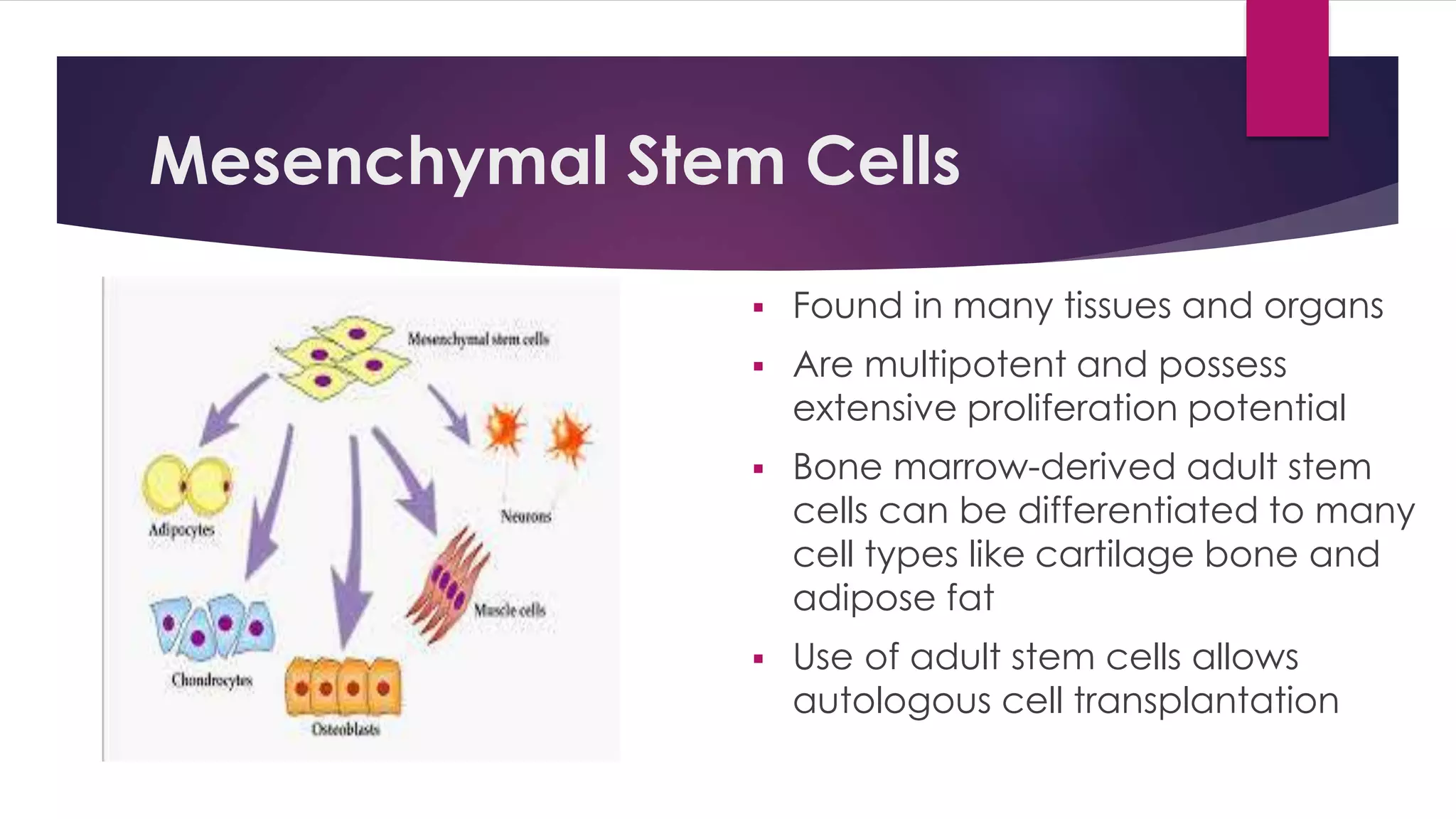
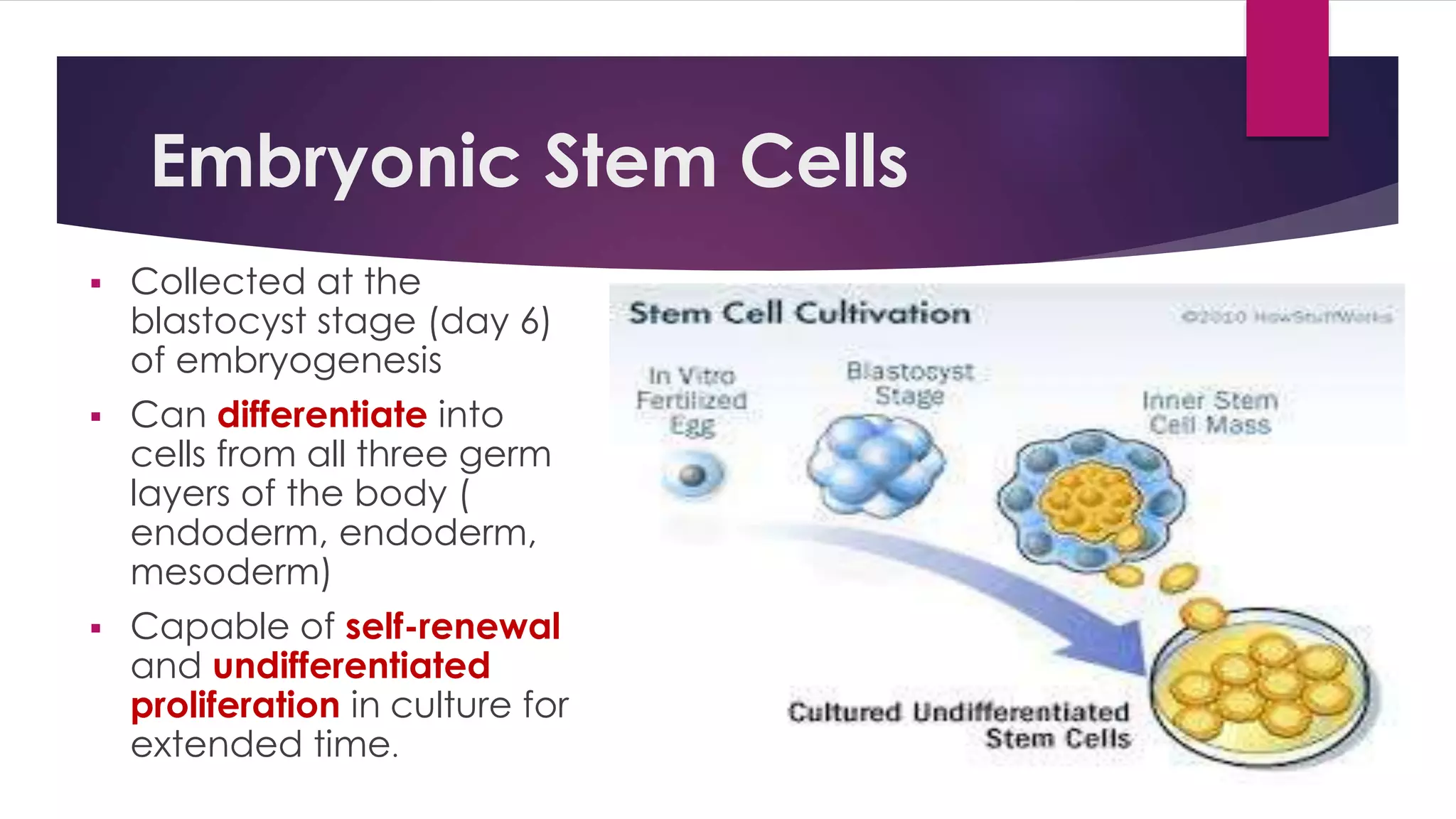
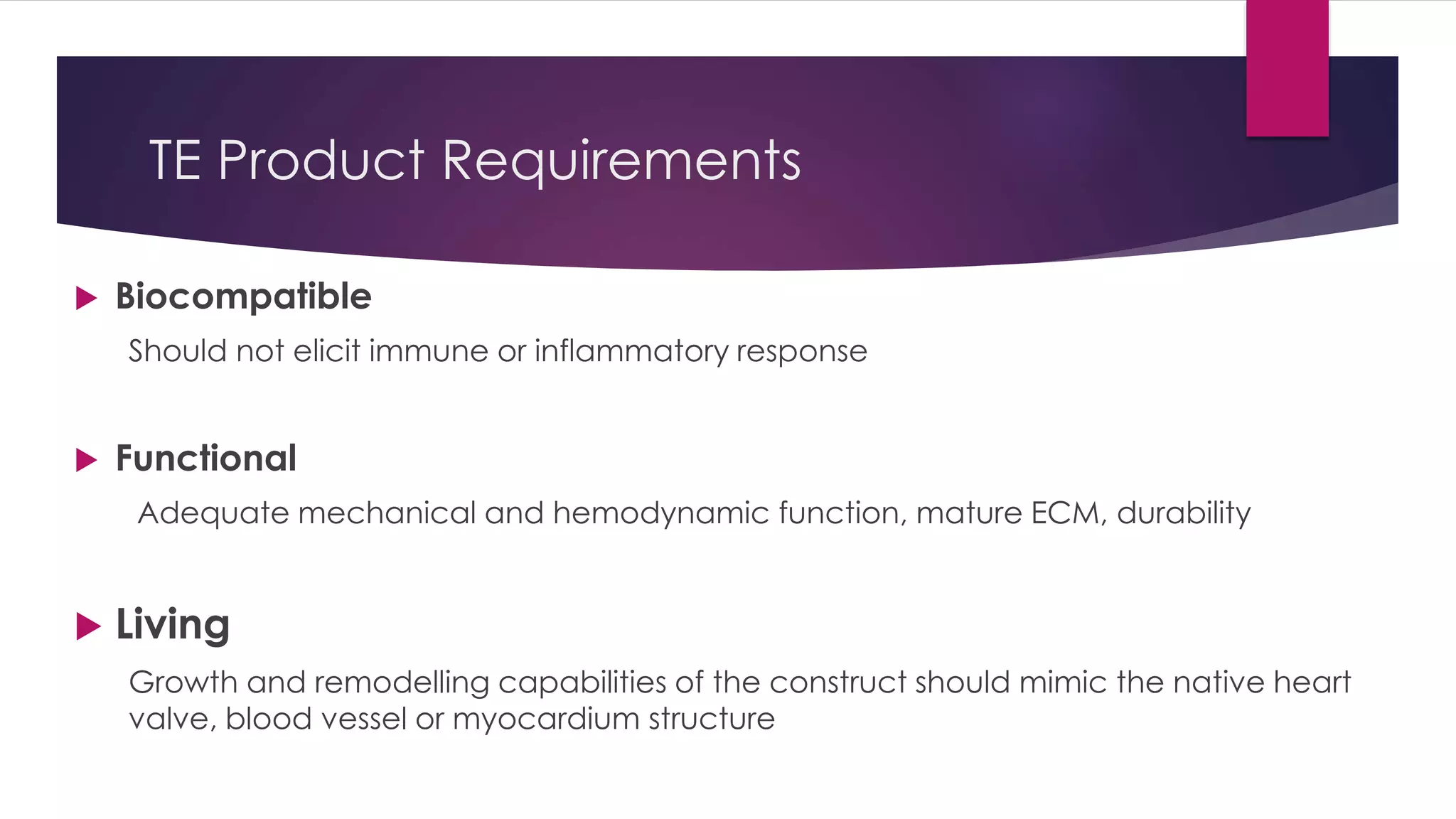
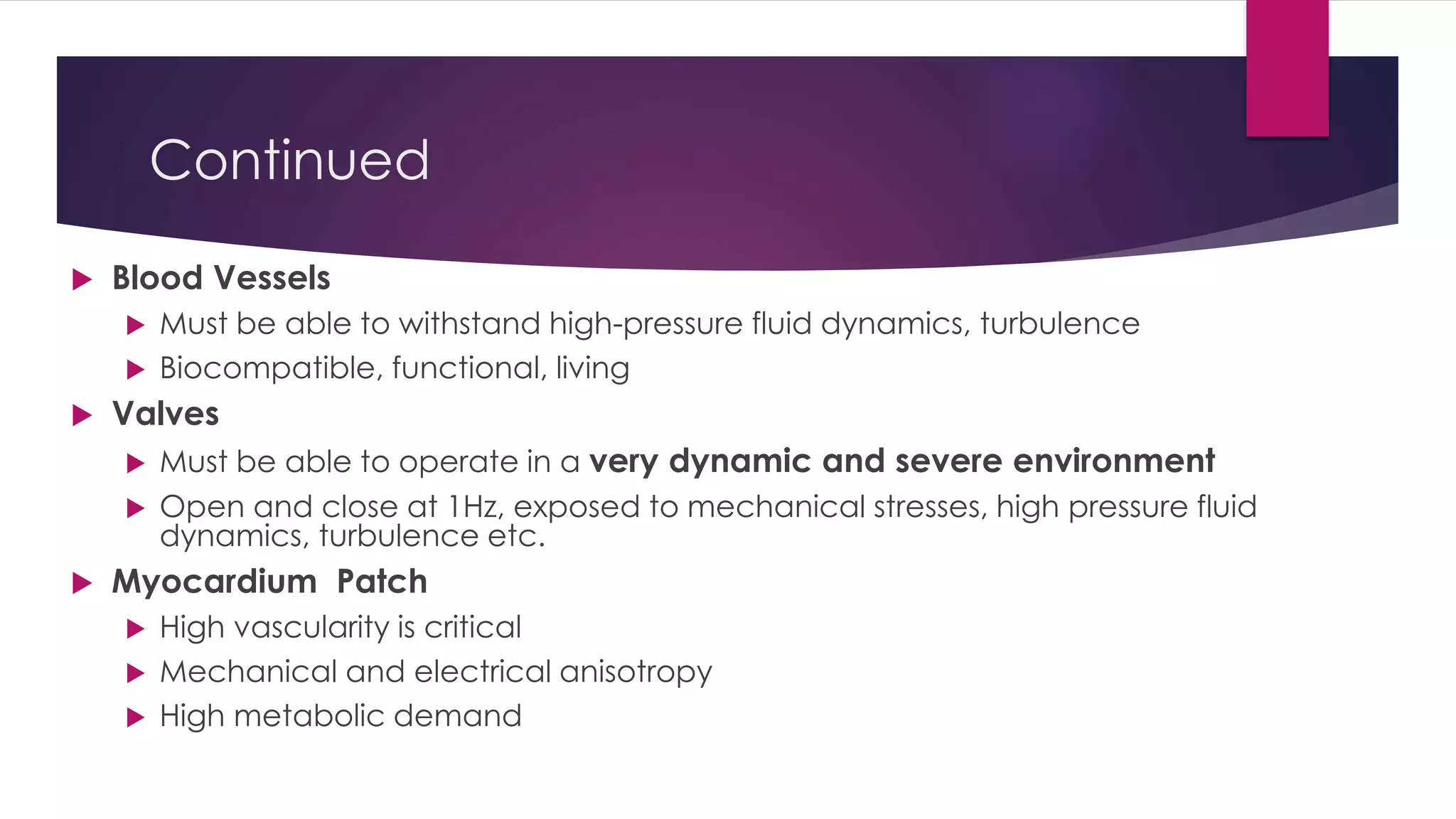
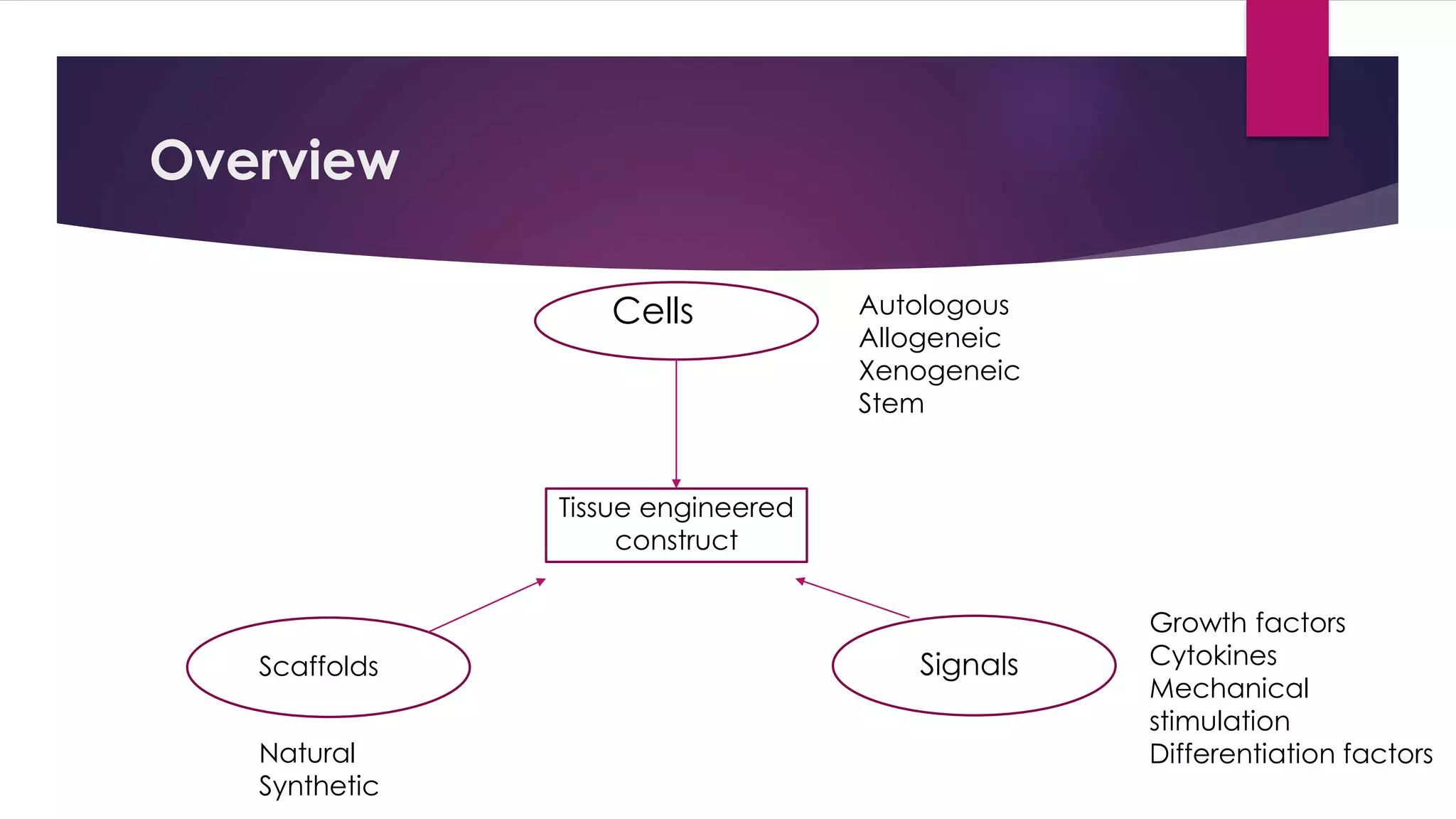
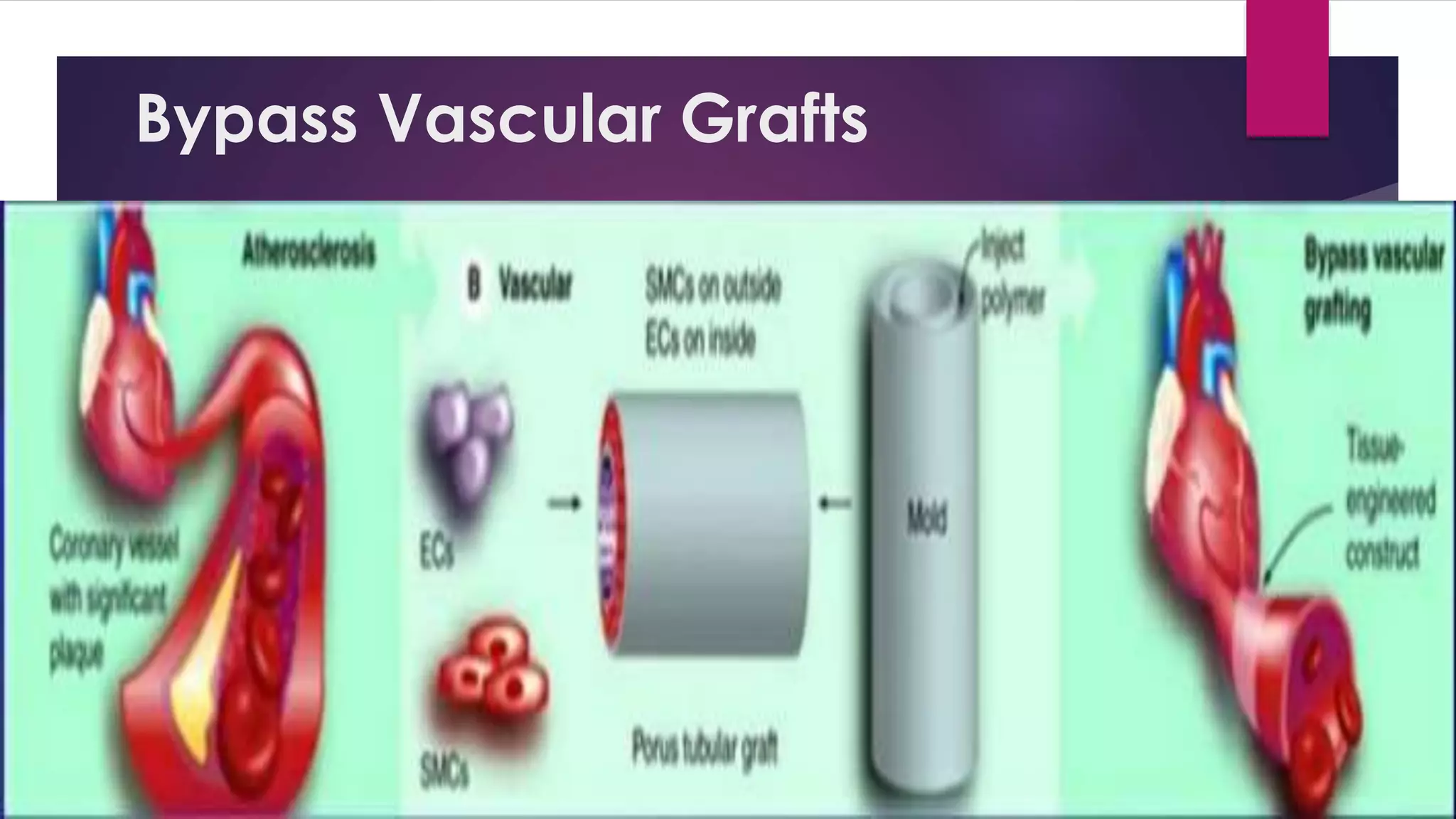
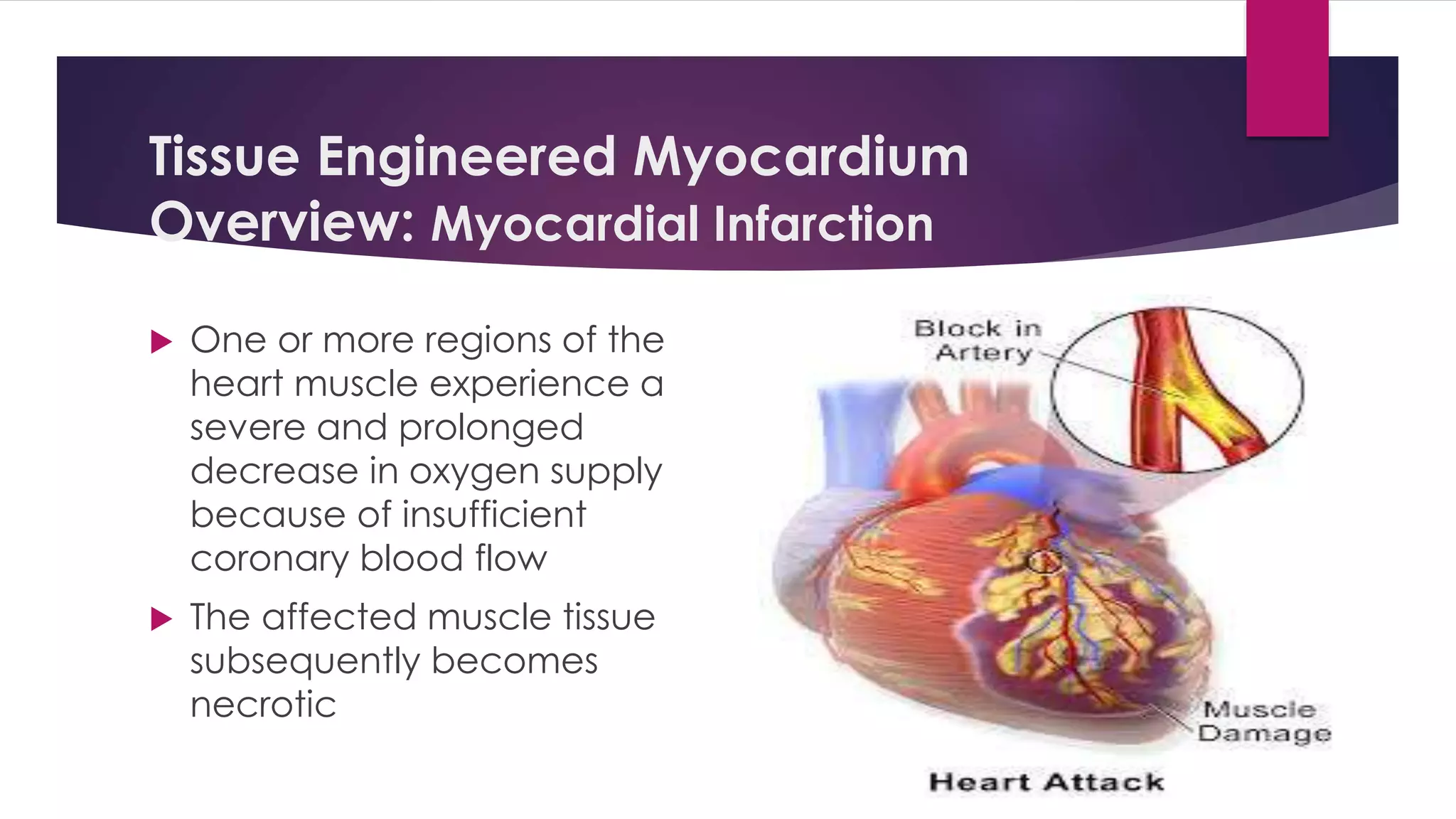
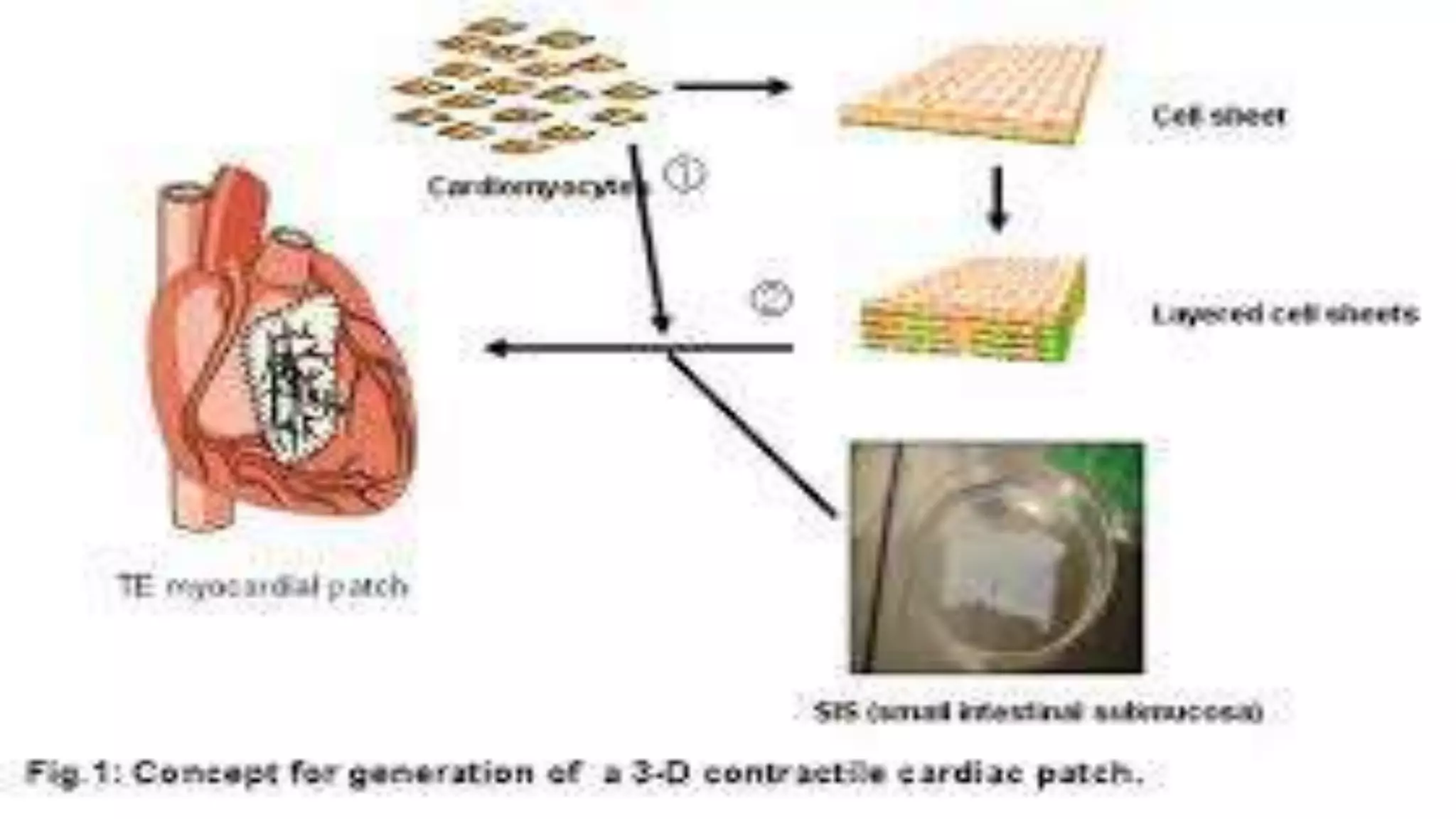
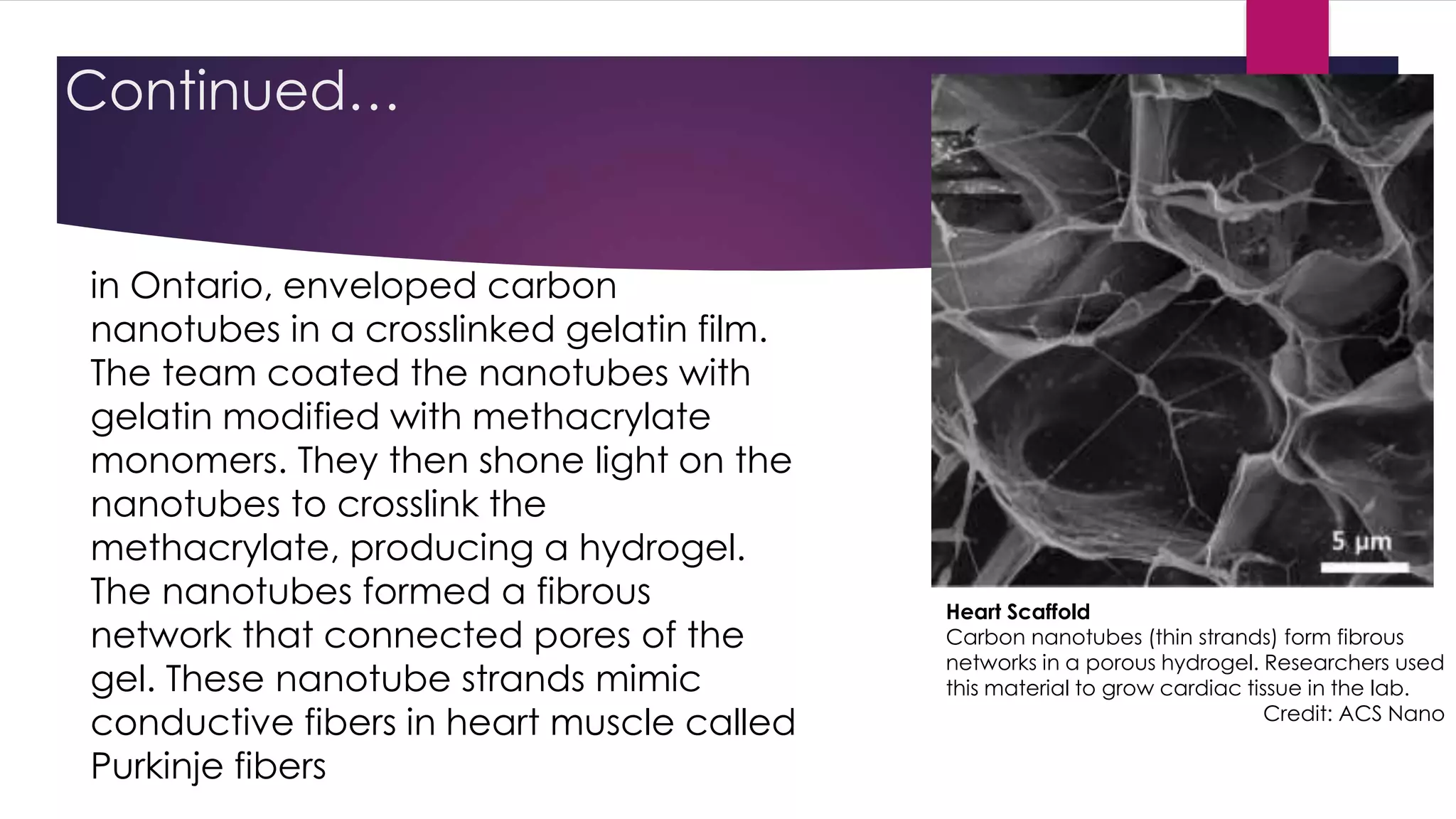
This document provides an overview of cardiac tissue engineering. It discusses the use of biomaterials like scaffolds and hydrogels to support cells for growing new cardiac tissue. Common cell types used include stem cells and differentiated cardiac cells. Tissue engineered constructs aim to be biocompatible, functional and living to replace damaged heart tissue like blood vessels, heart valves, and myocardial patches. Recent developments include engineered tissues that closely mimic heart muscle mechanics and biology.