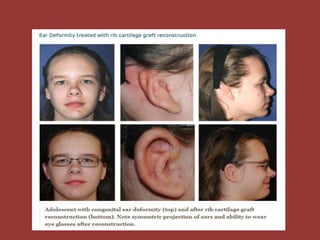
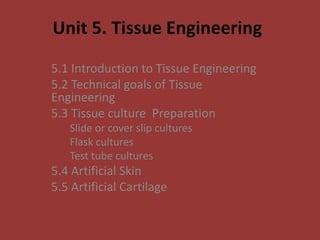
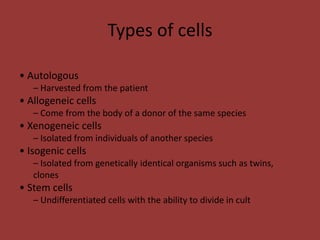
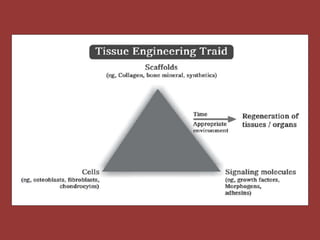
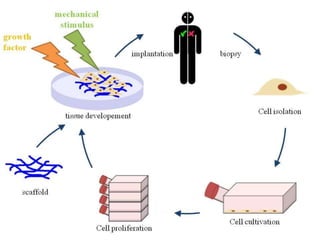
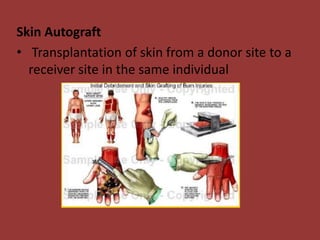
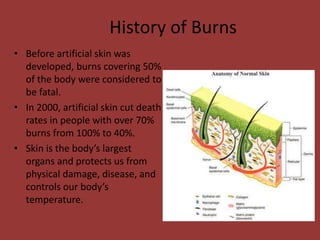
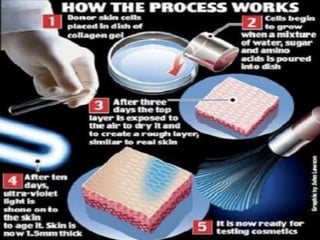
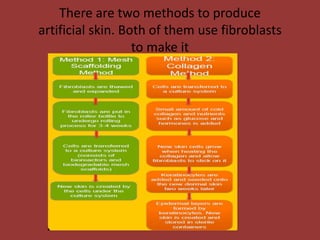
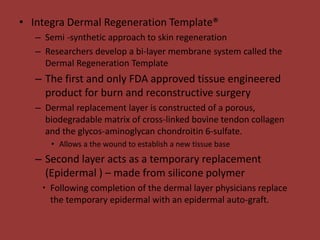
This document discusses tissue engineering and its applications in artificial skin and cartilage. It begins by defining tissue engineering as applying engineering and life science principles to develop biological substitutes that restore or improve tissue function. It then discusses the goals of tissue engineering, including restoring biomechanical and physiological function. The document outlines different types of cells used, including autologous, allogeneic, xenogeneic and stem cells. It provides details on different tissue culture techniques and goes on to describe artificial skin and cartilage, including their history, manufacturing processes, cell sources and advantages/disadvantages.