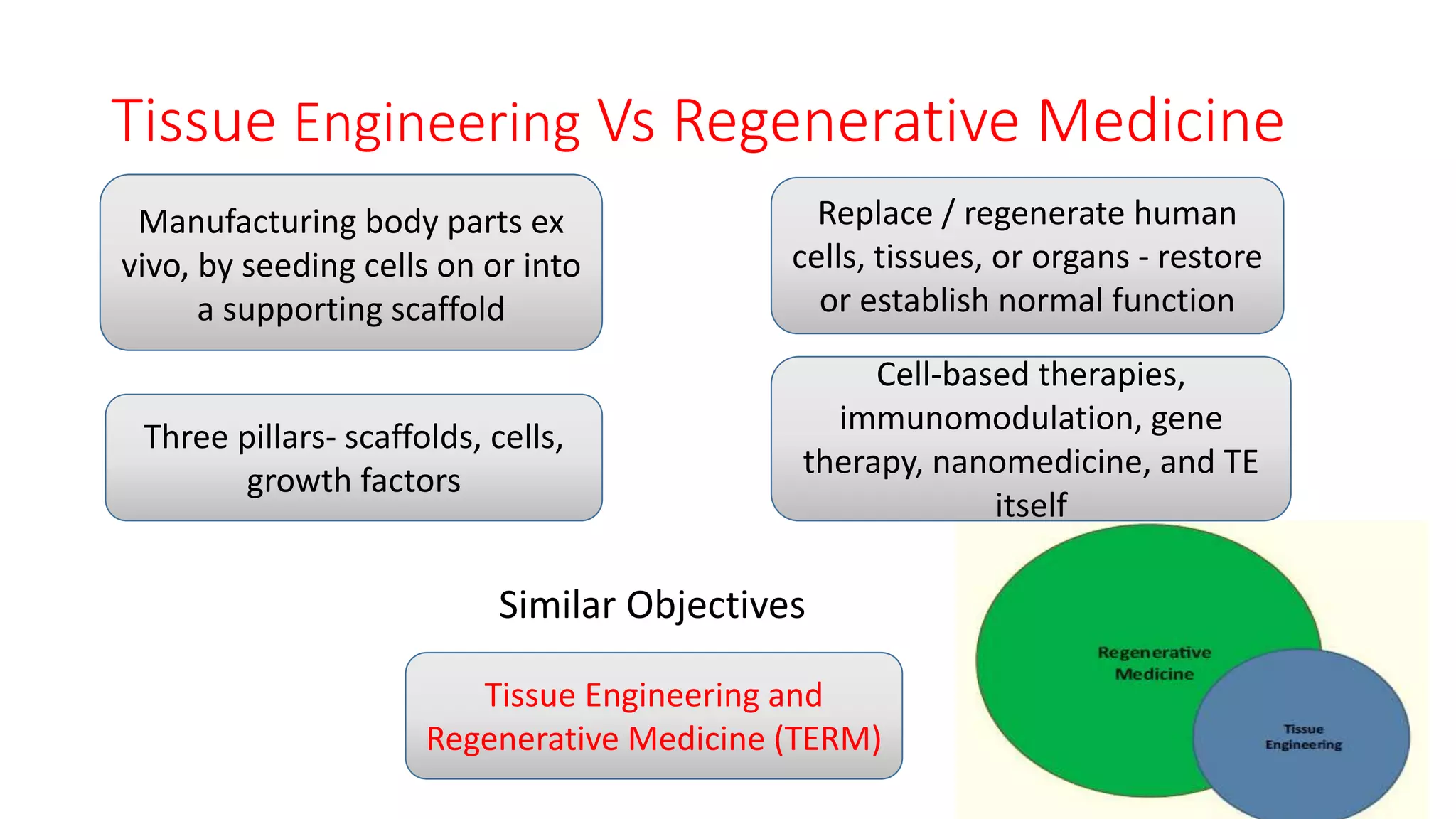
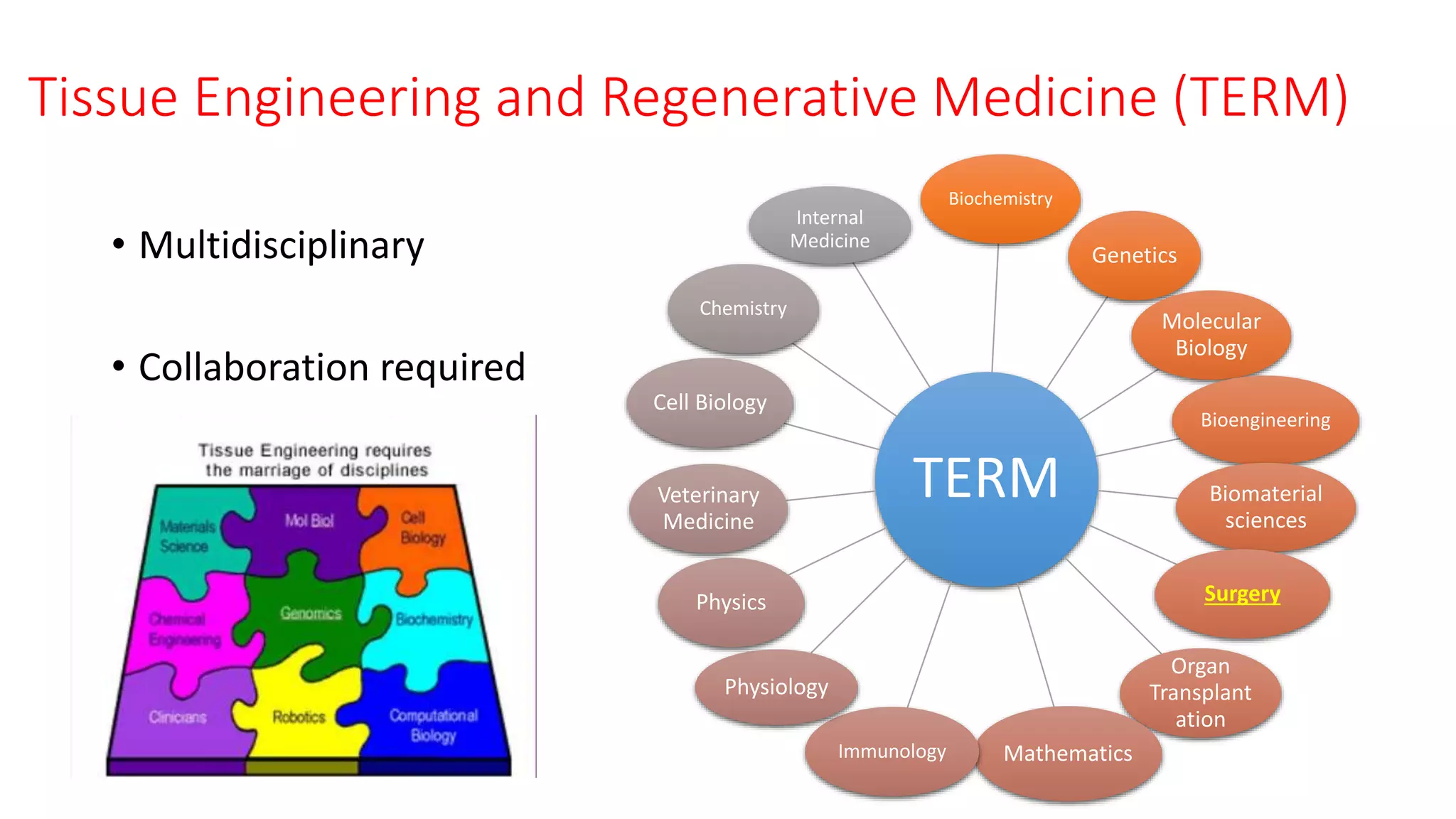
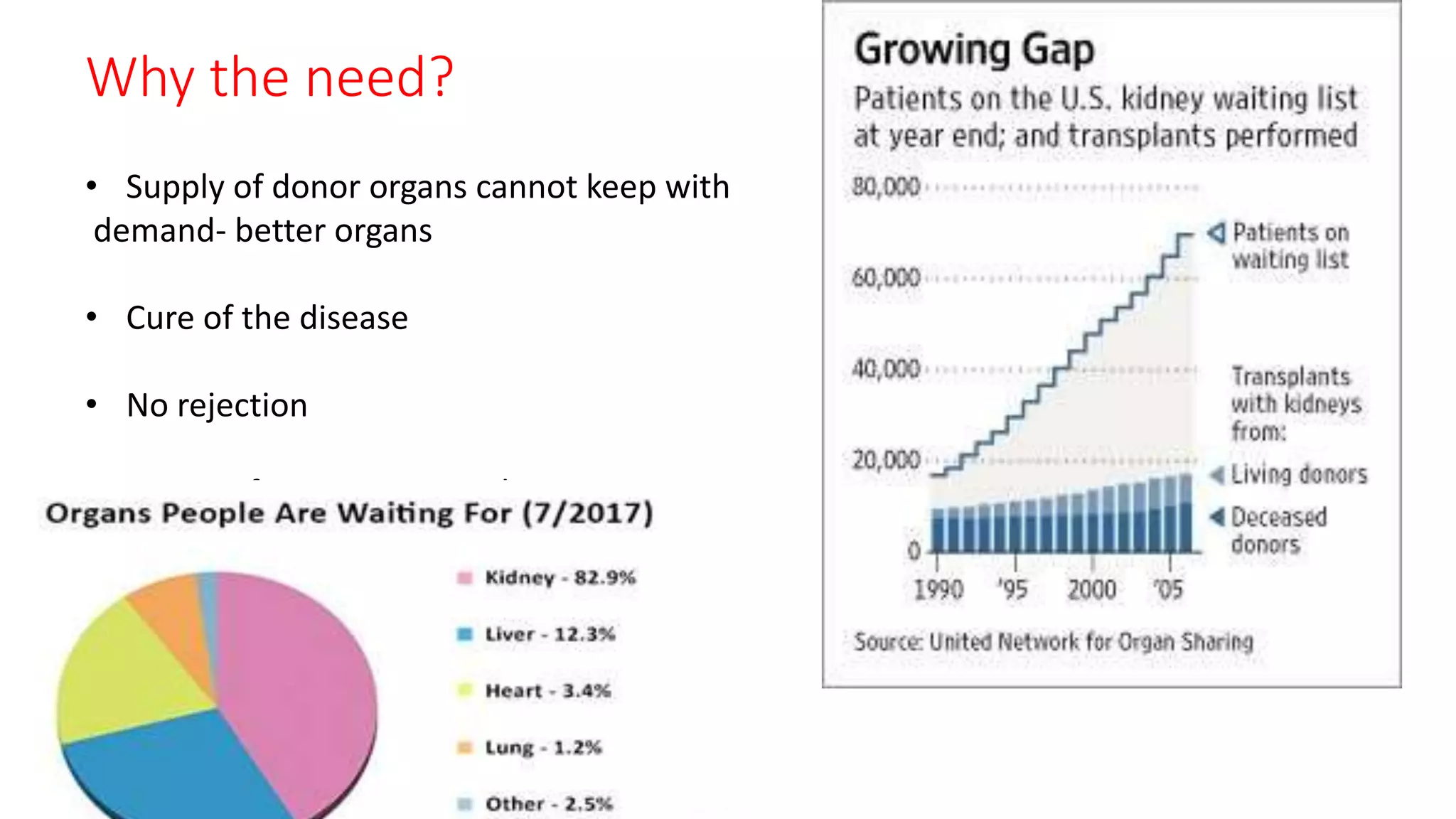
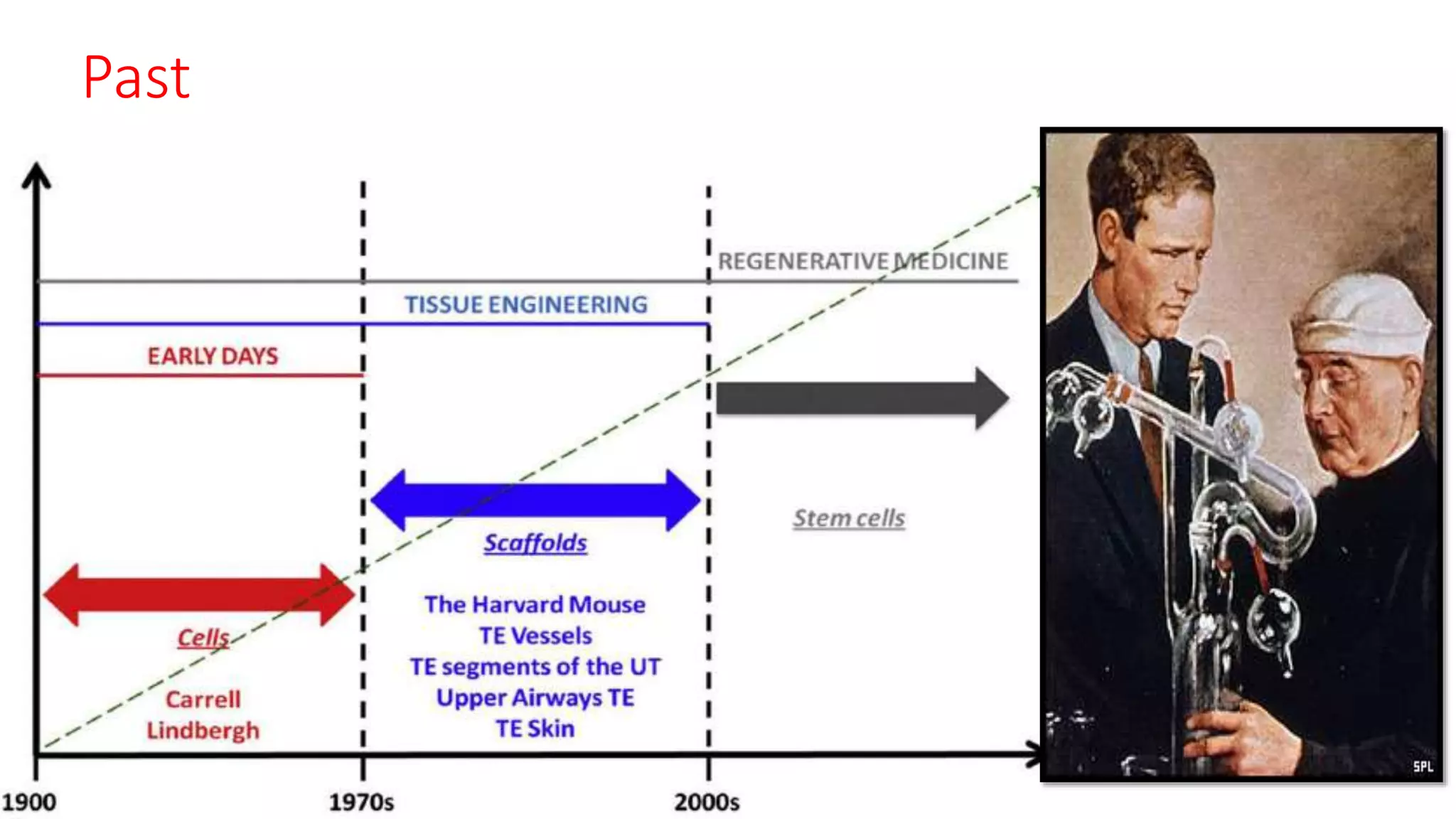
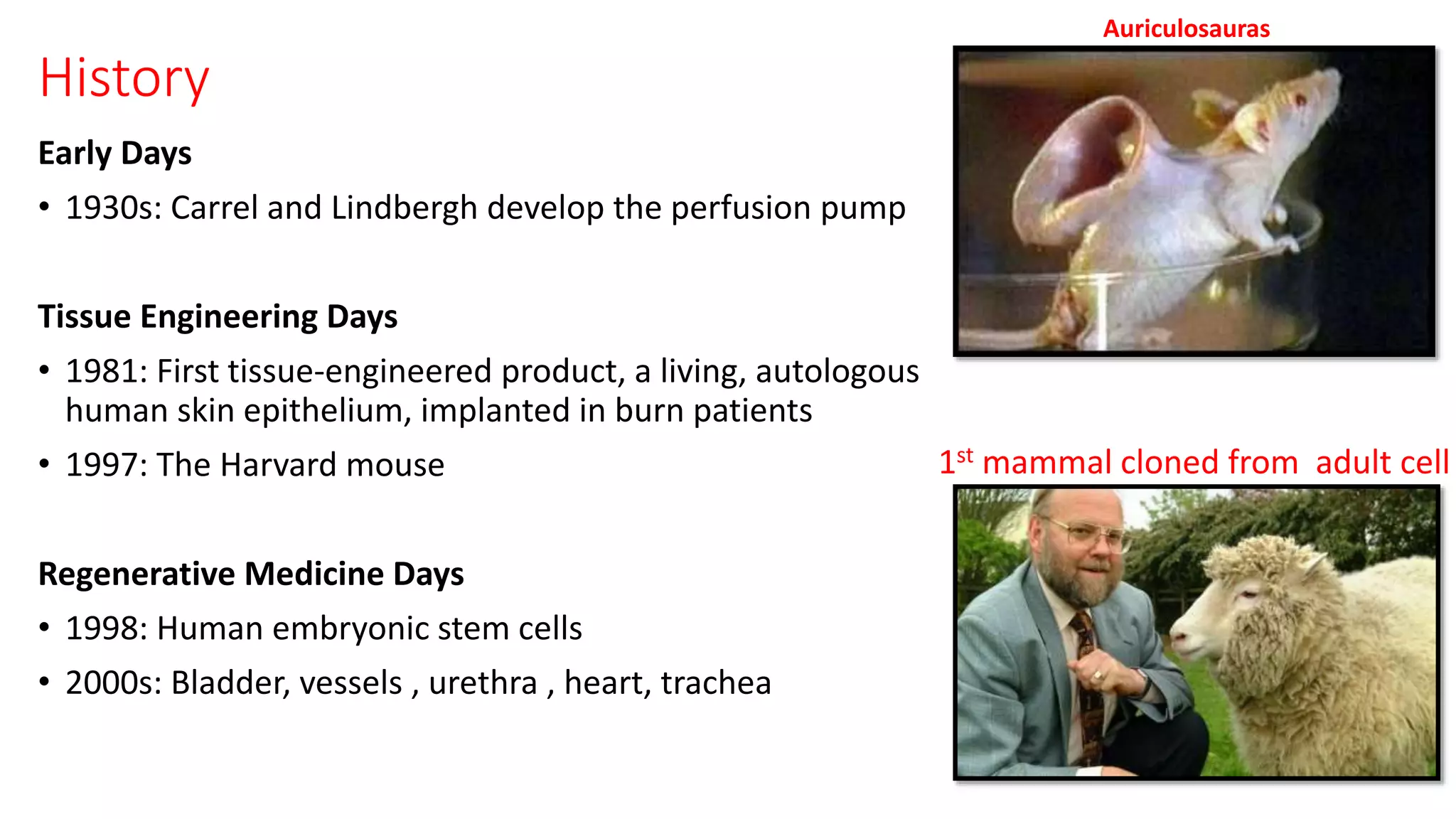
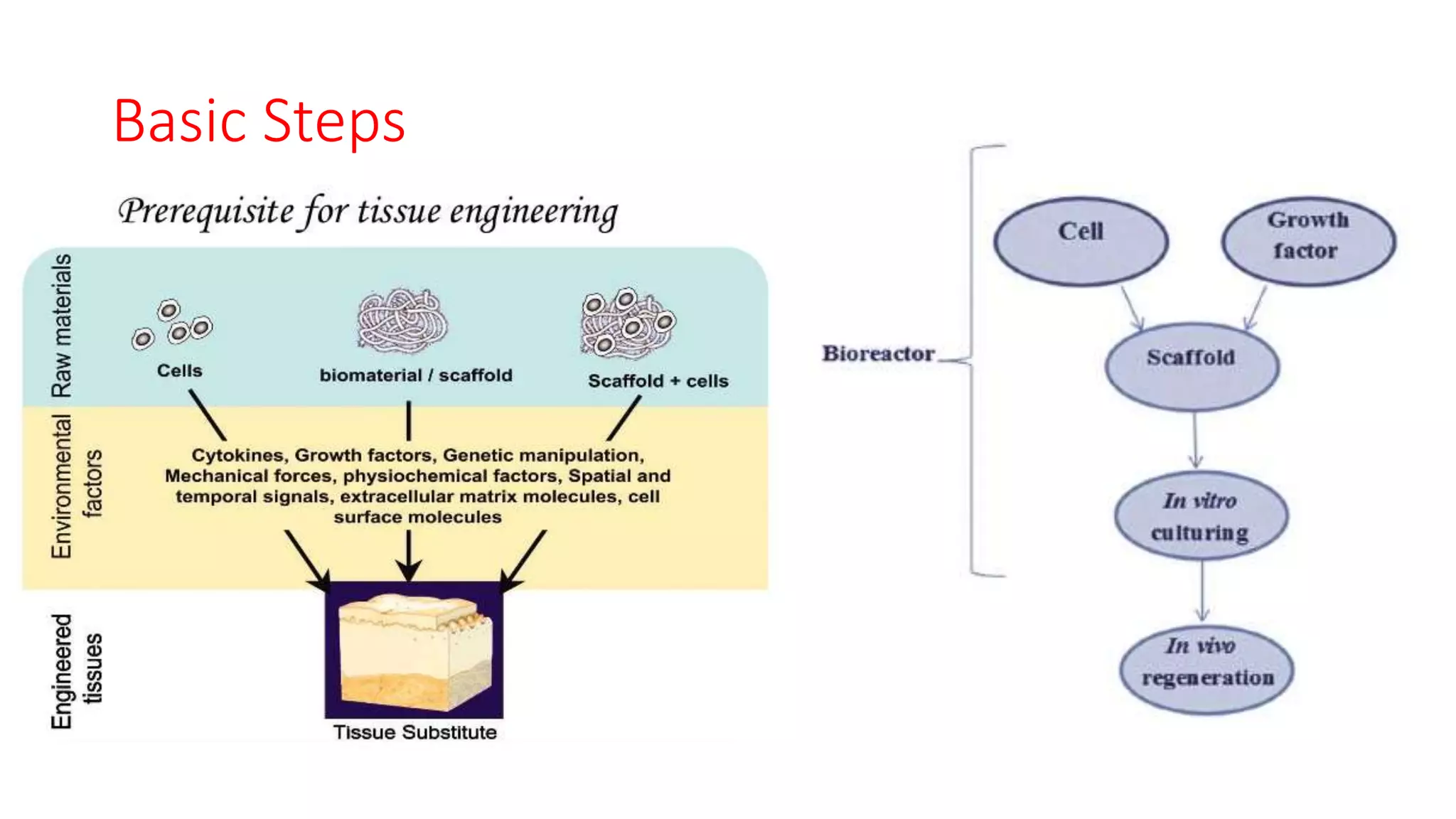
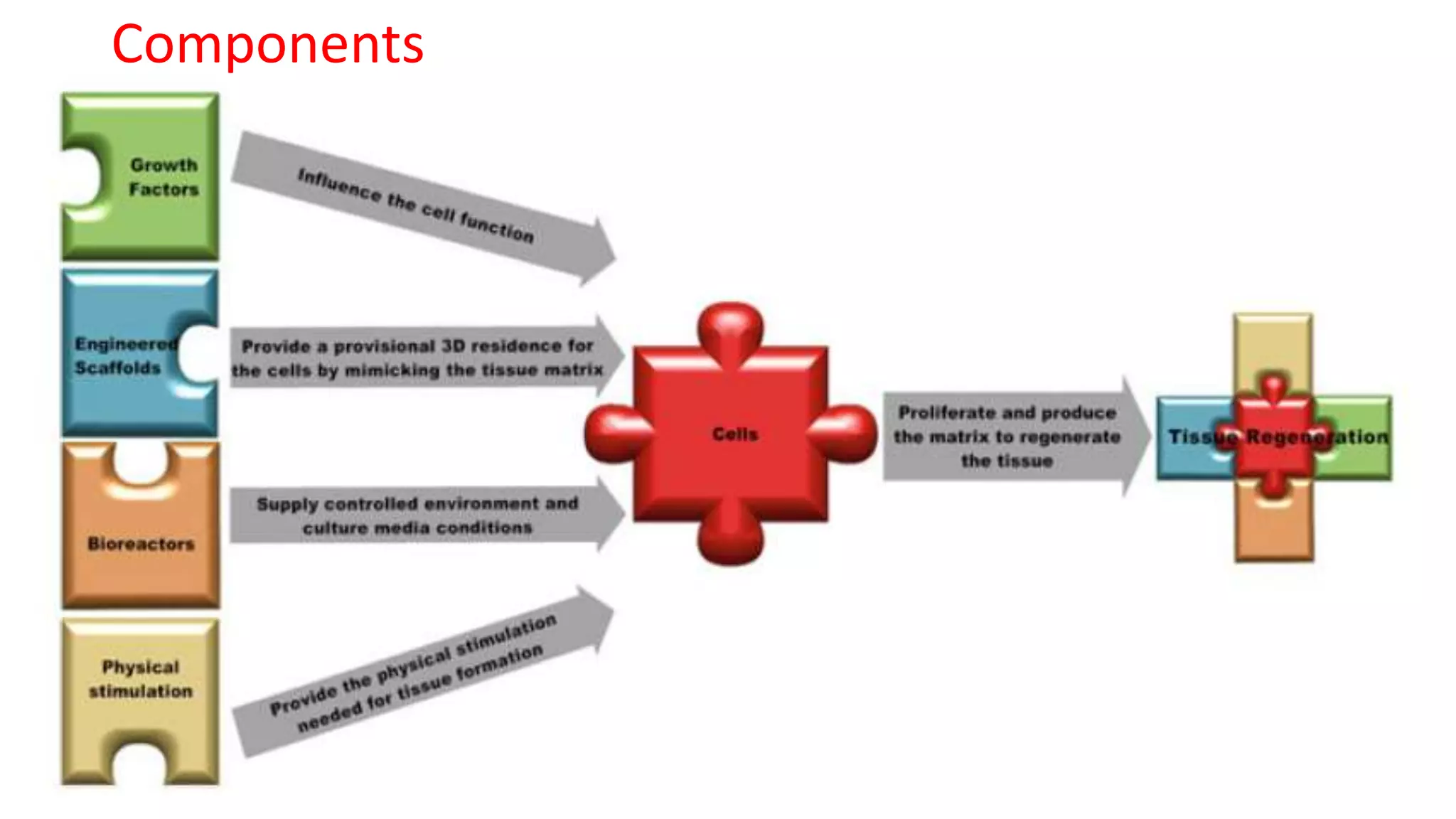
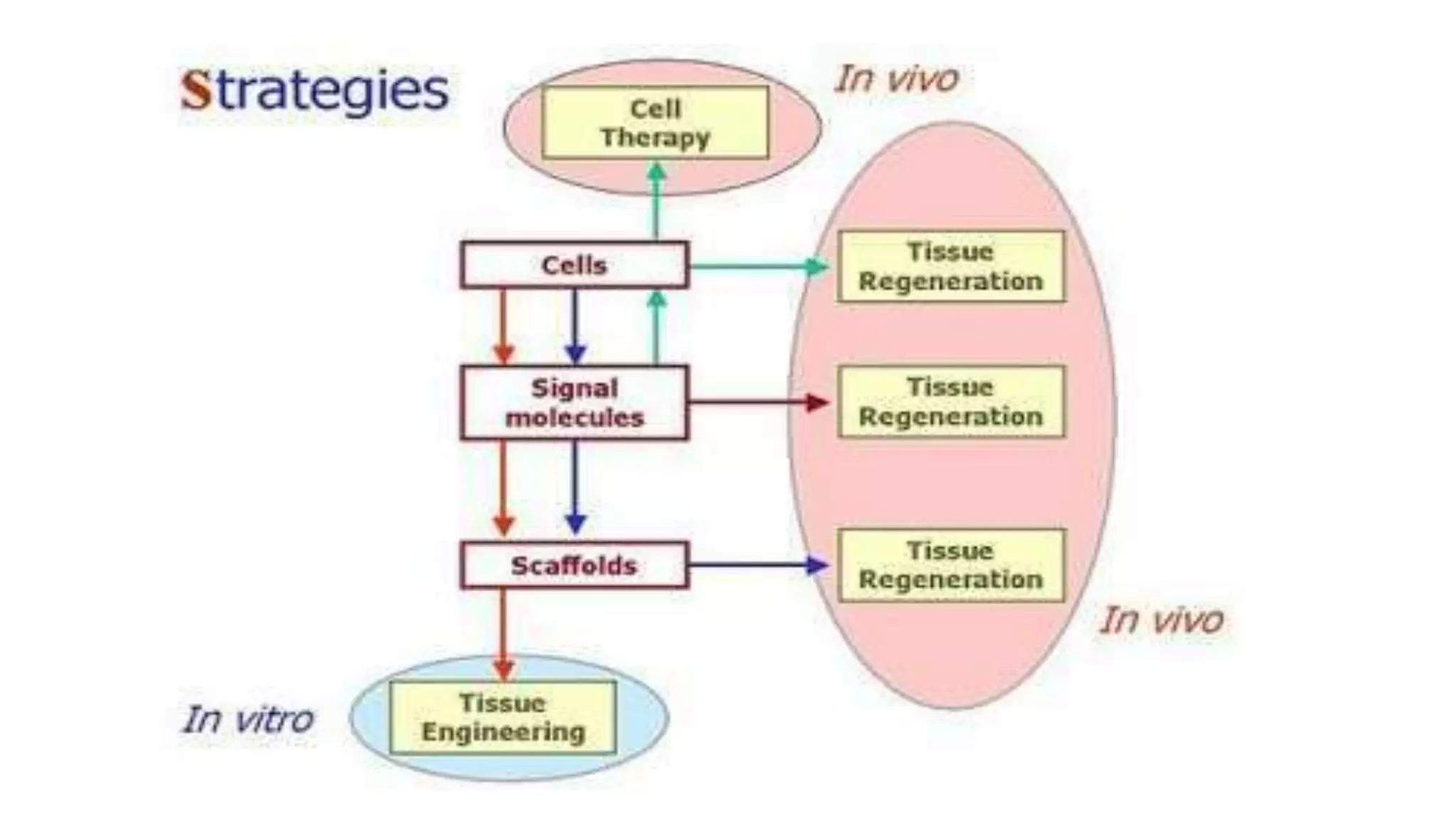
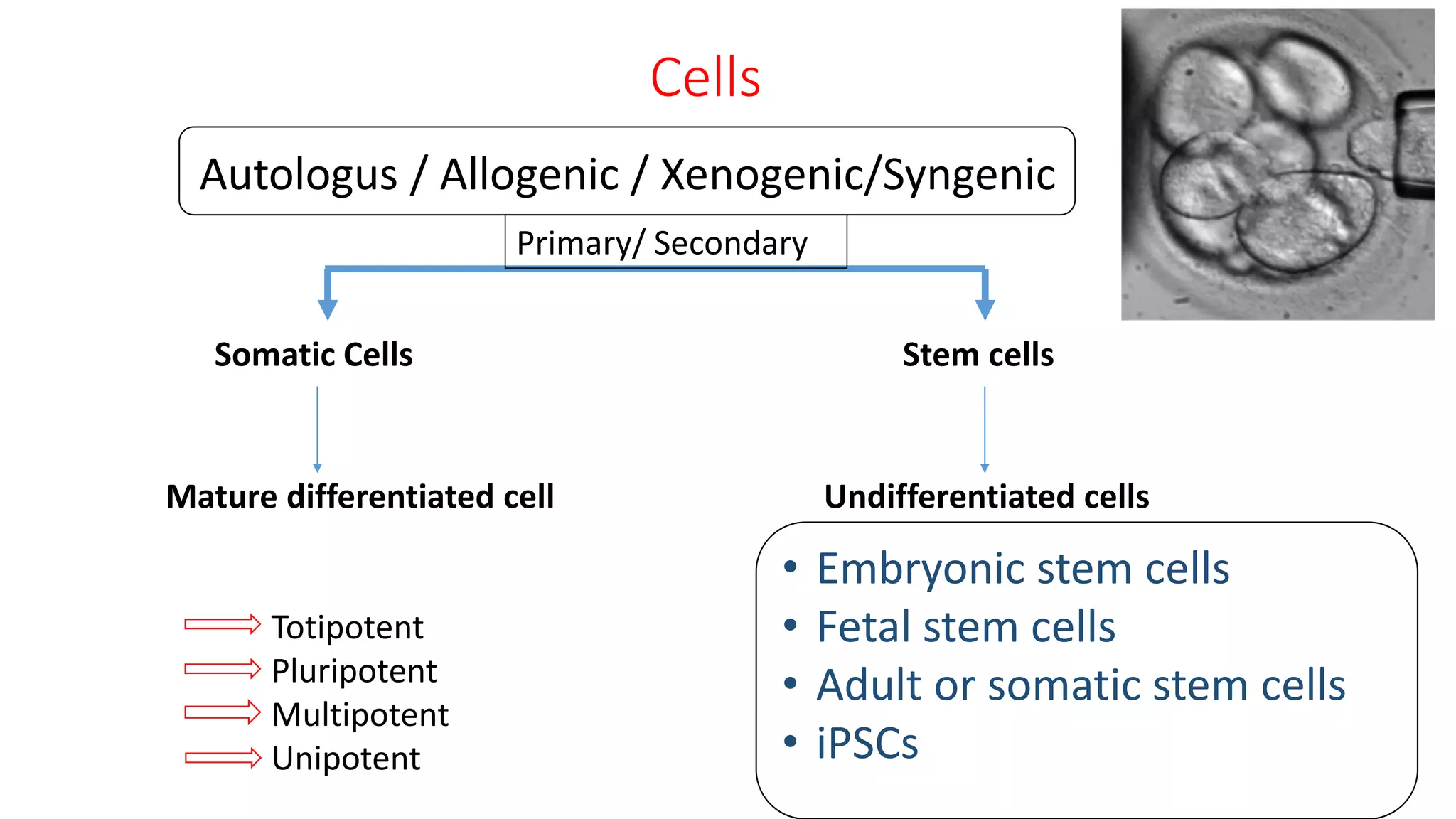
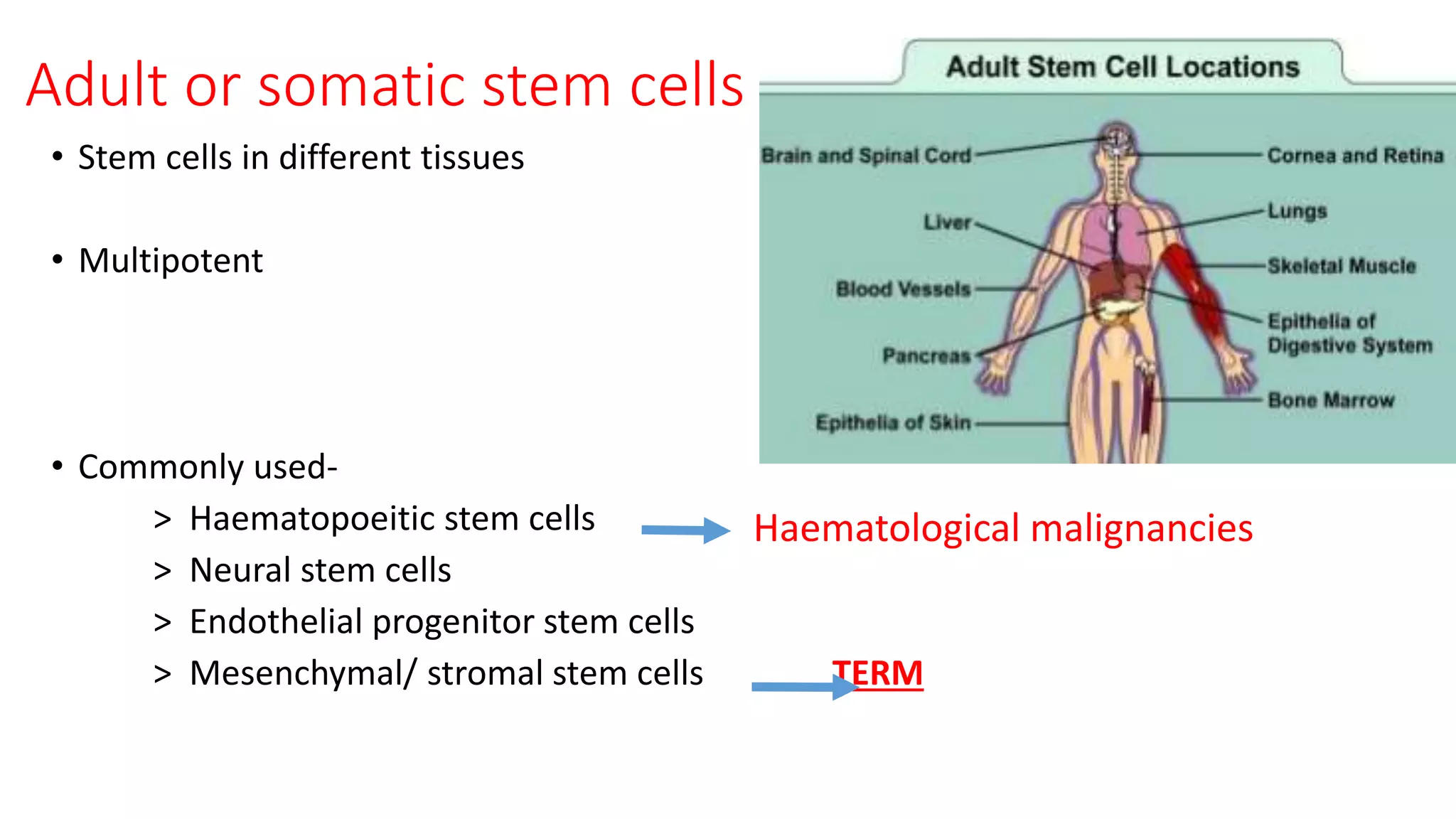
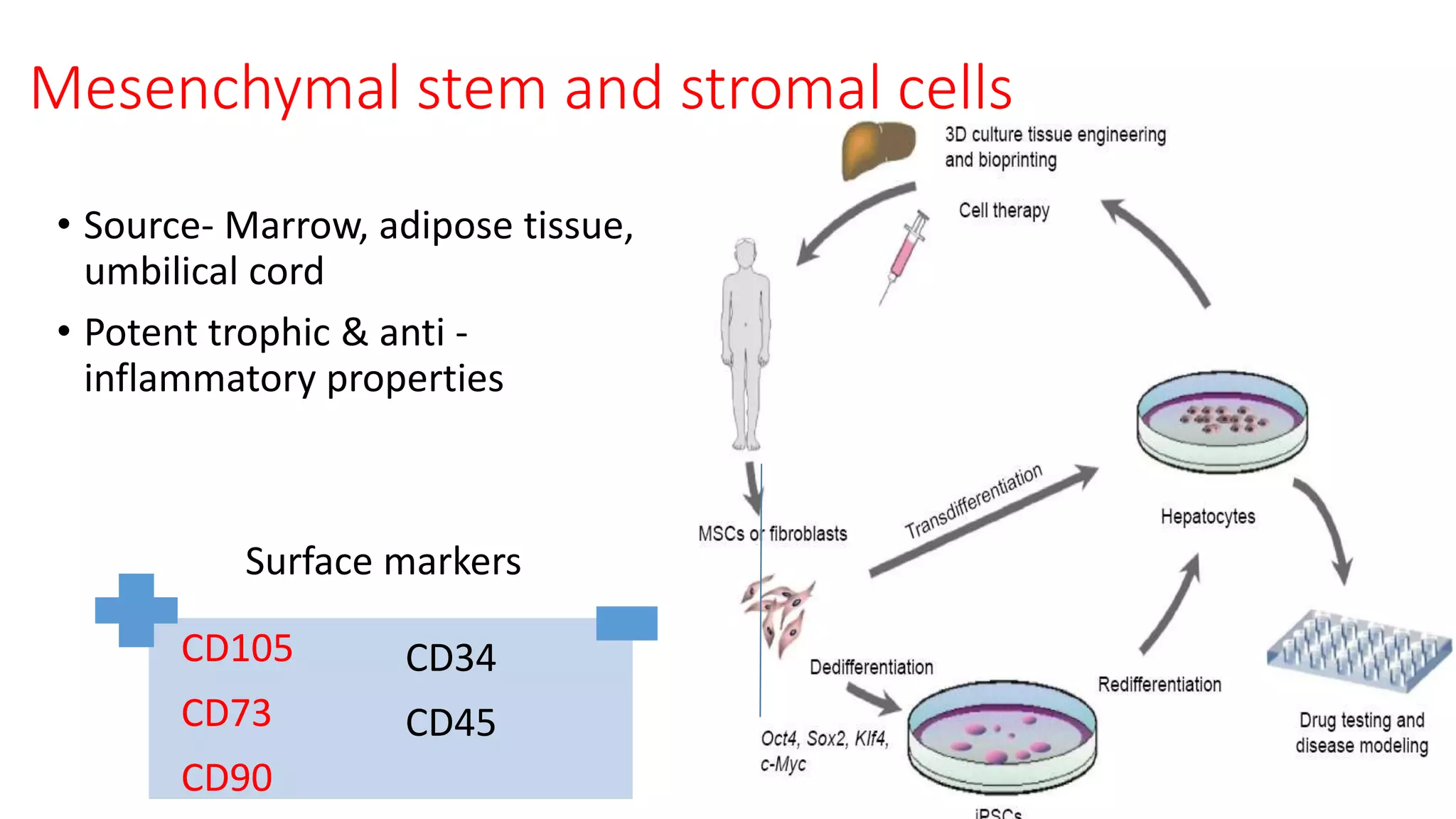
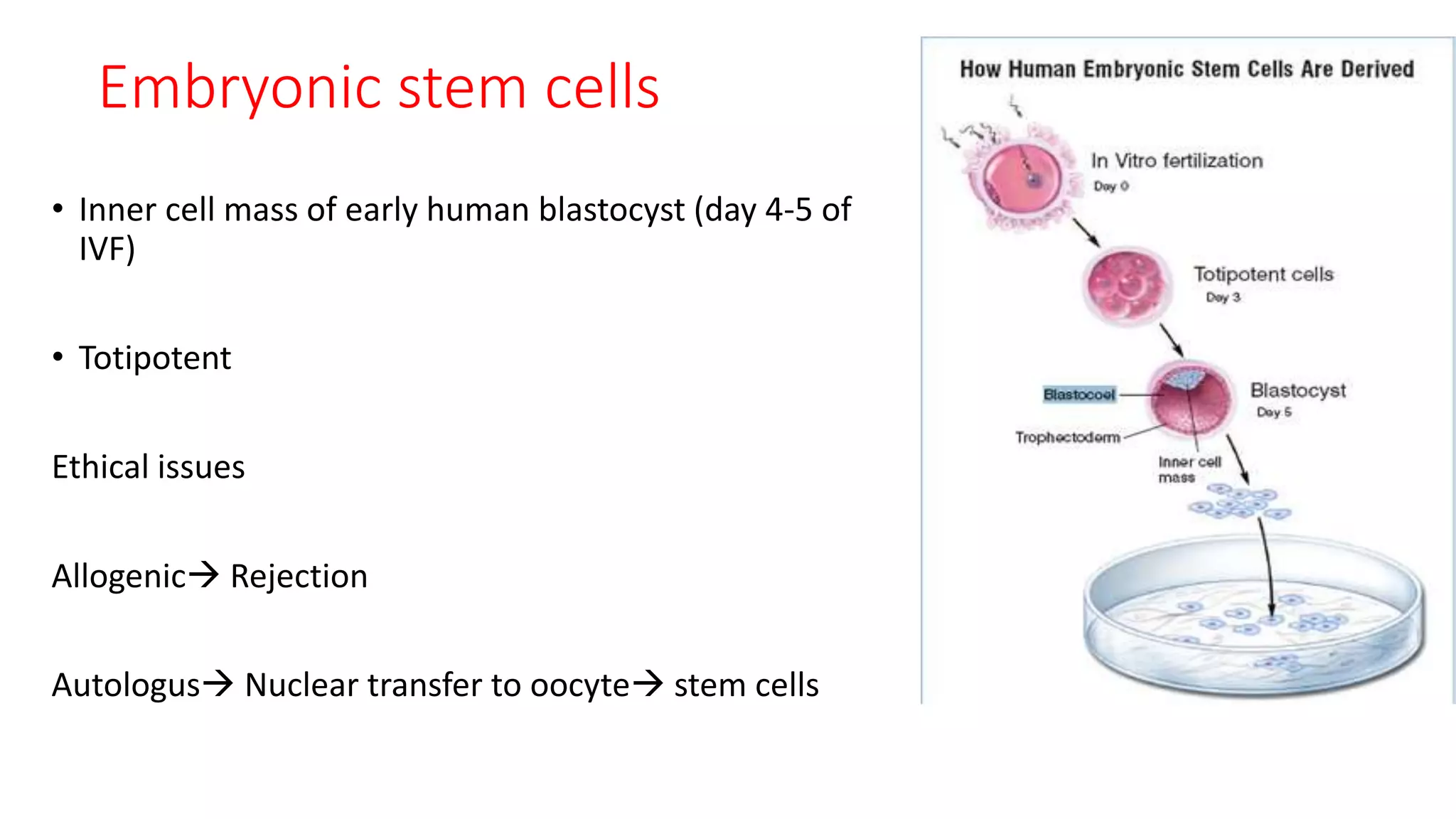
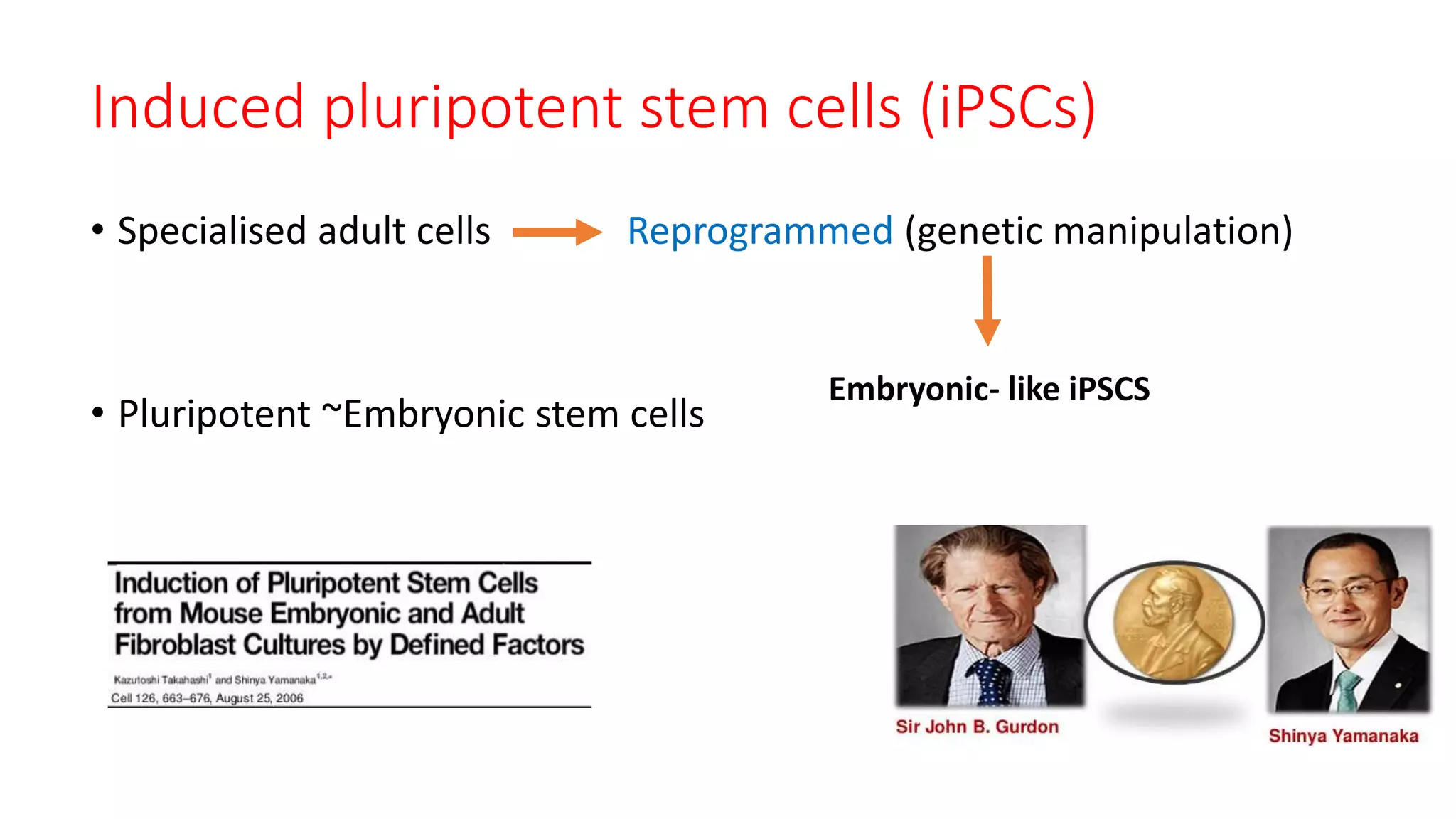
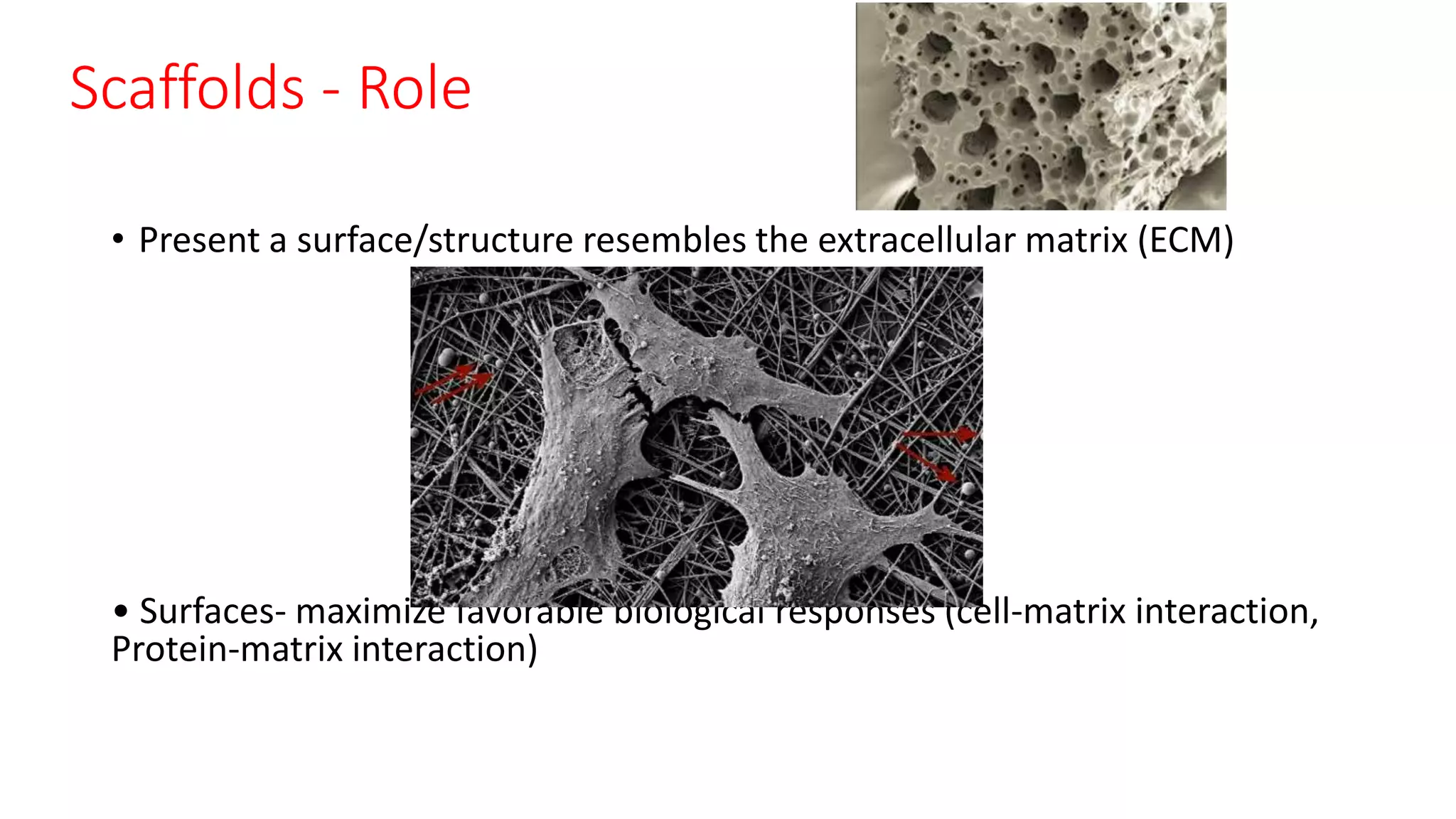
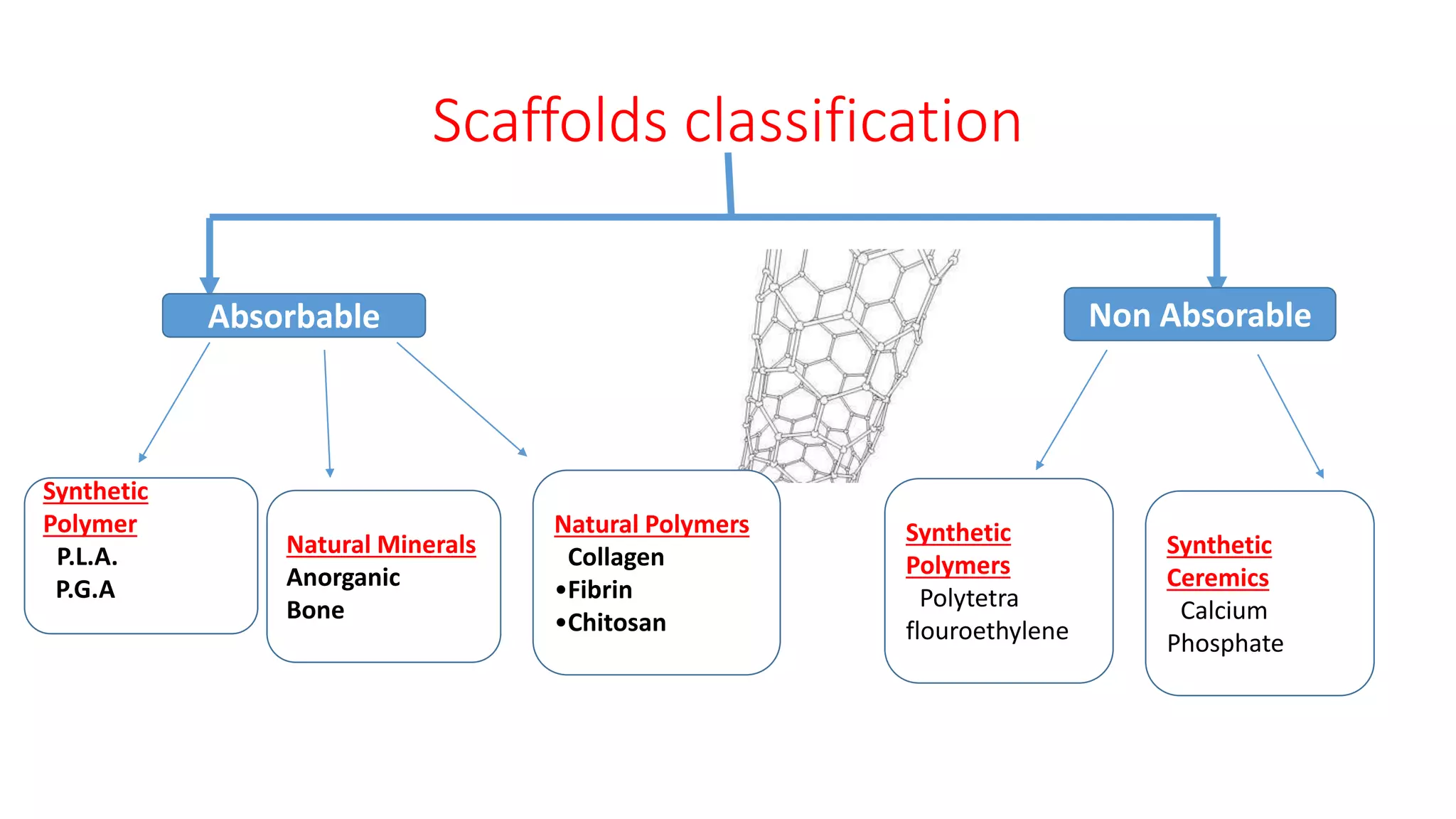
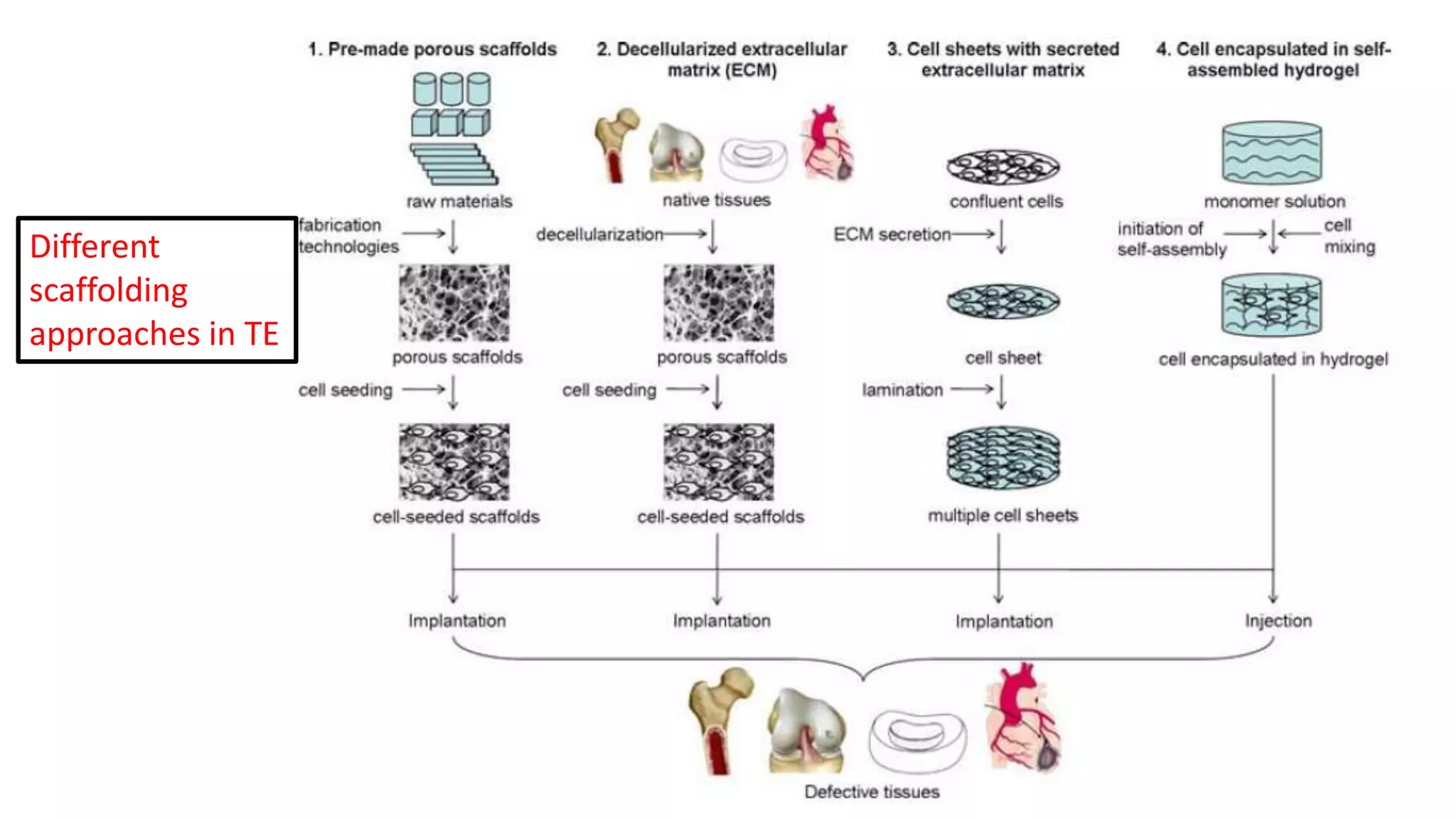
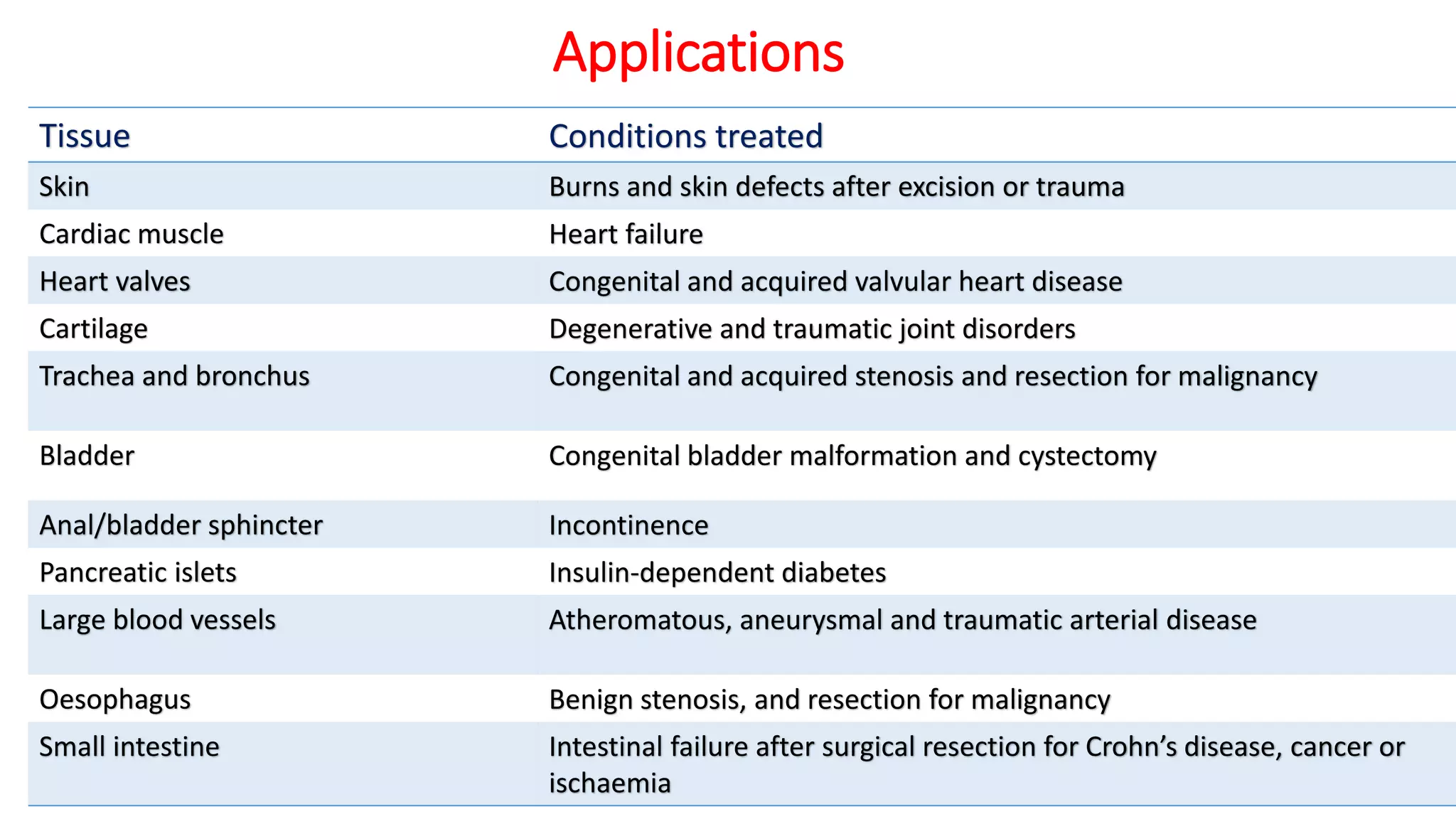
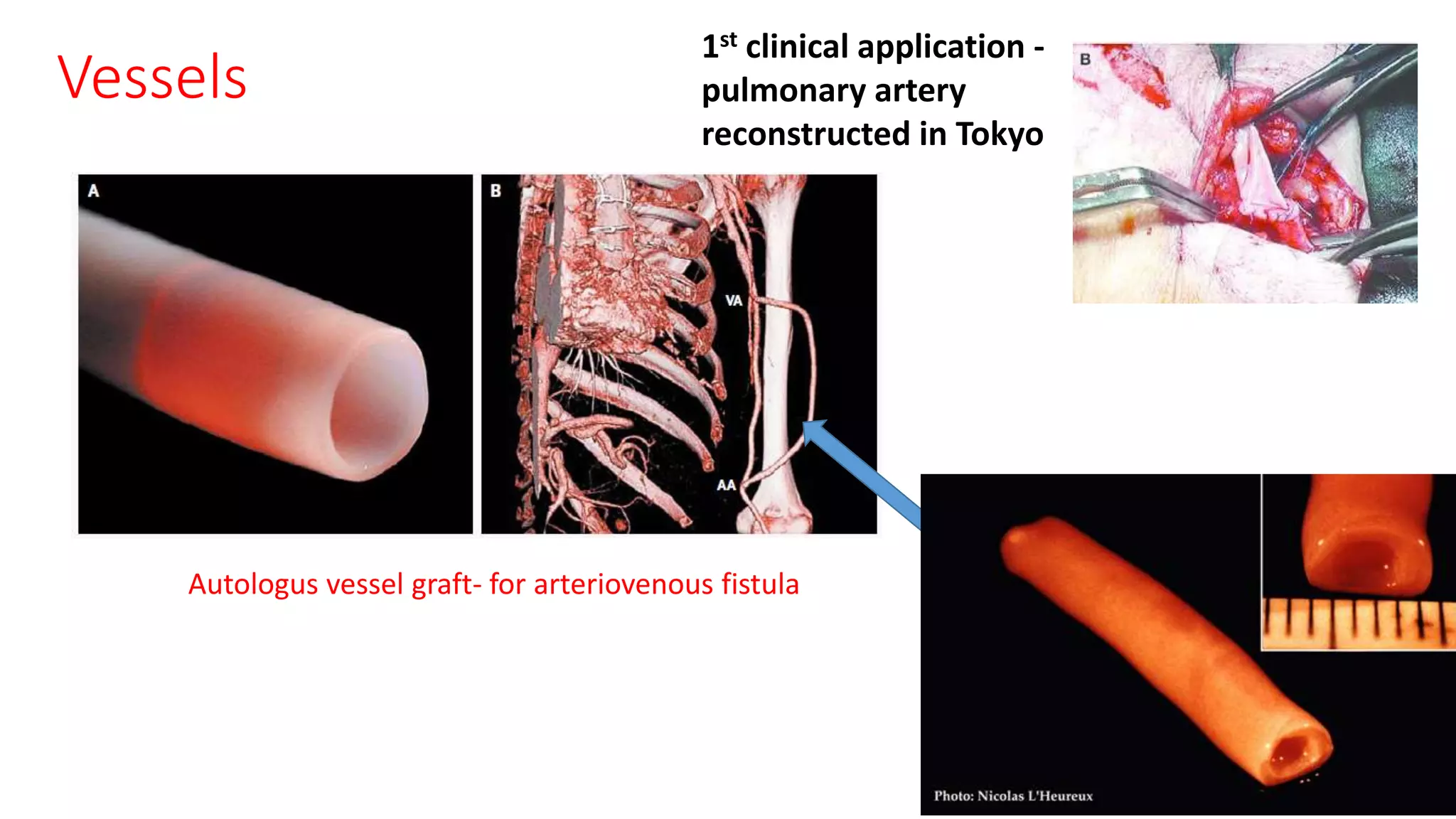
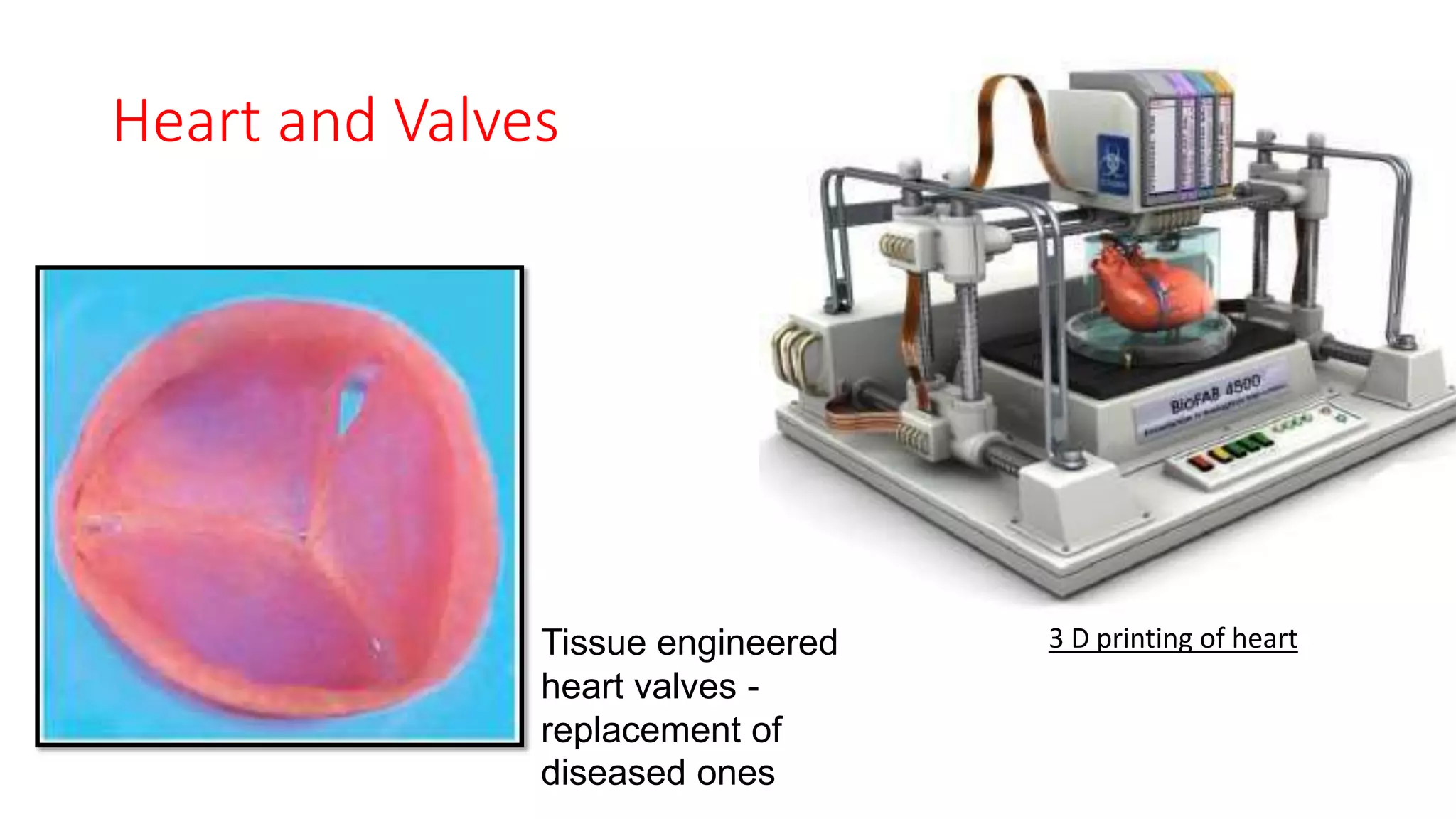
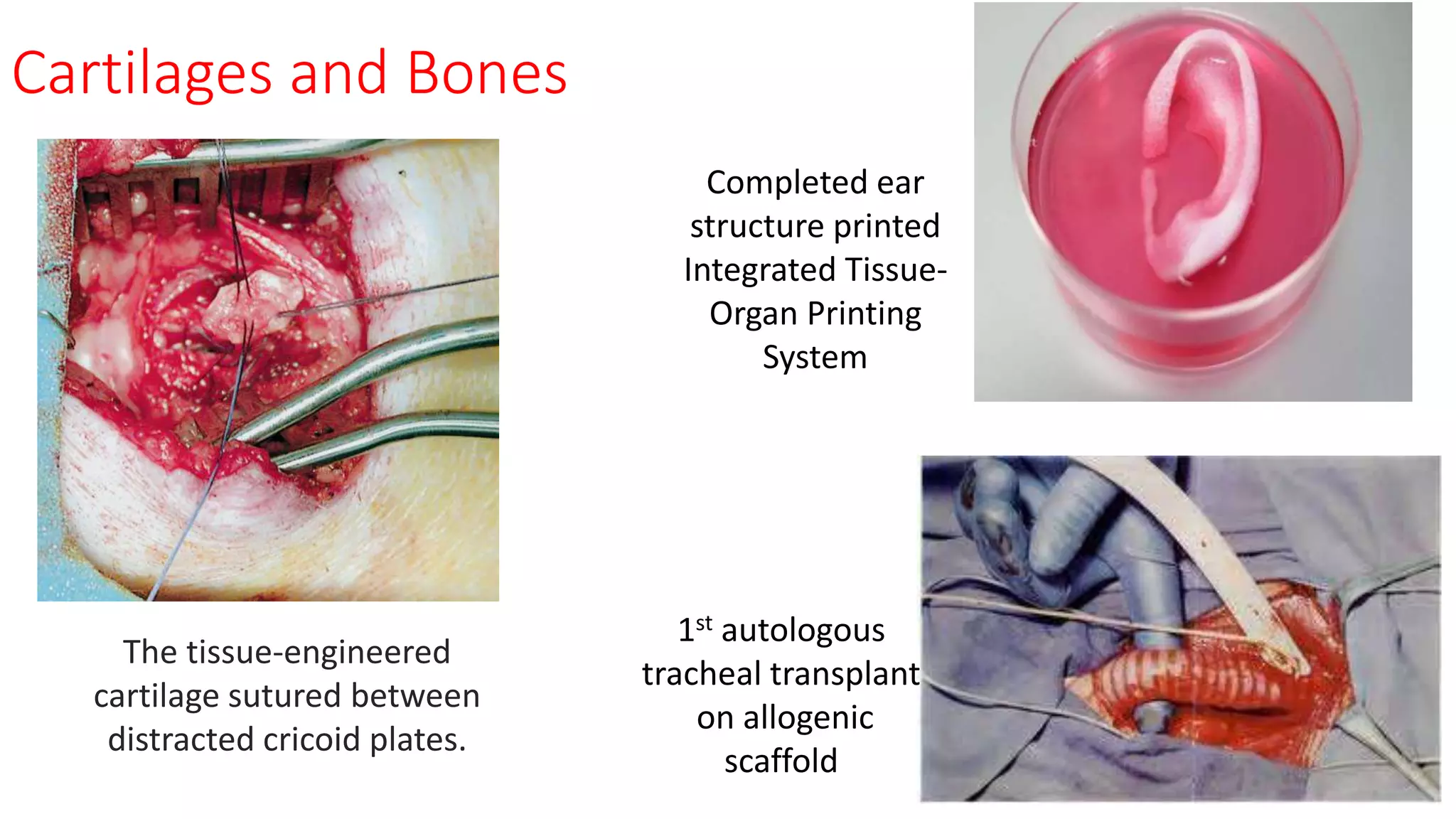
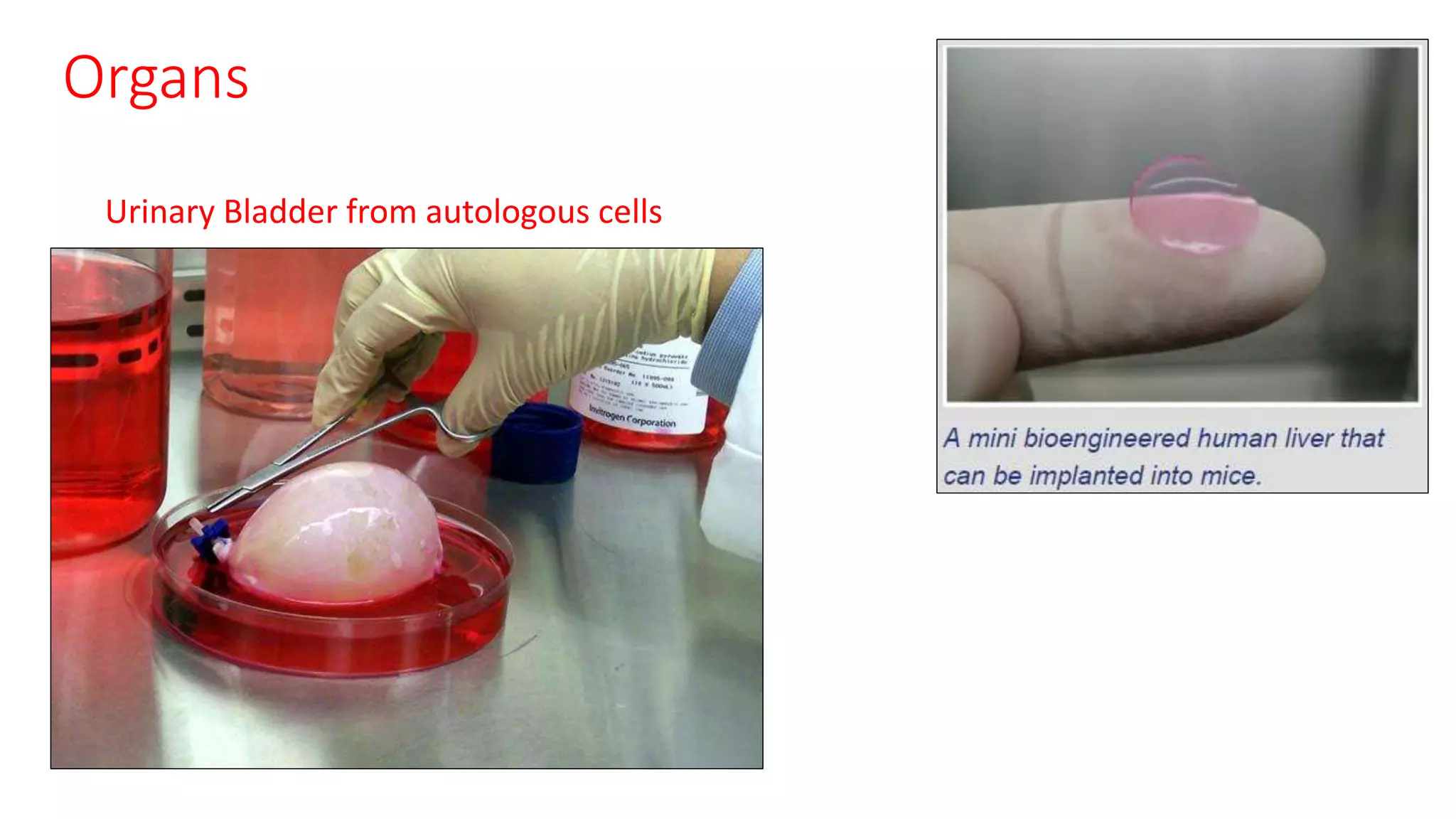
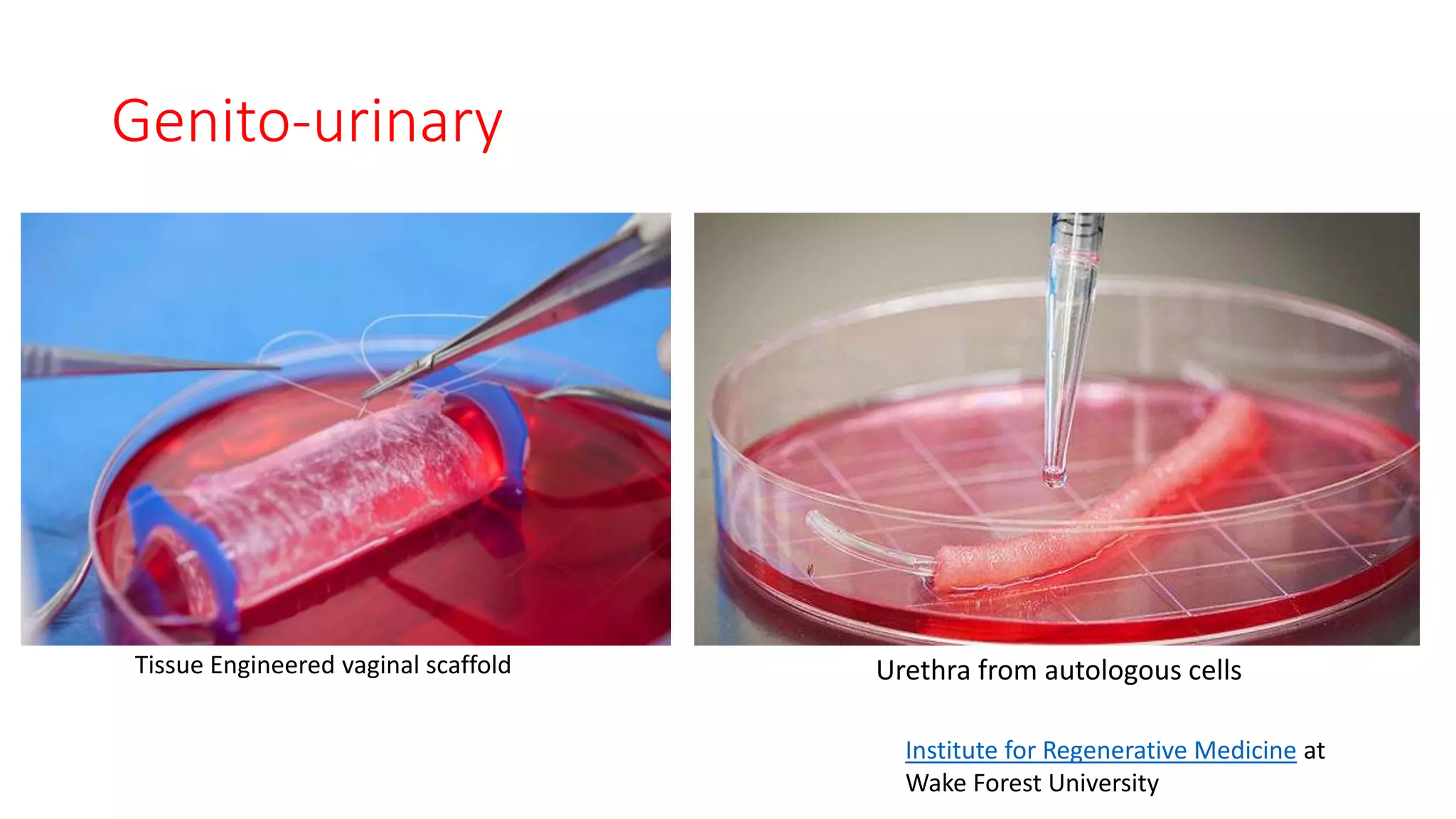
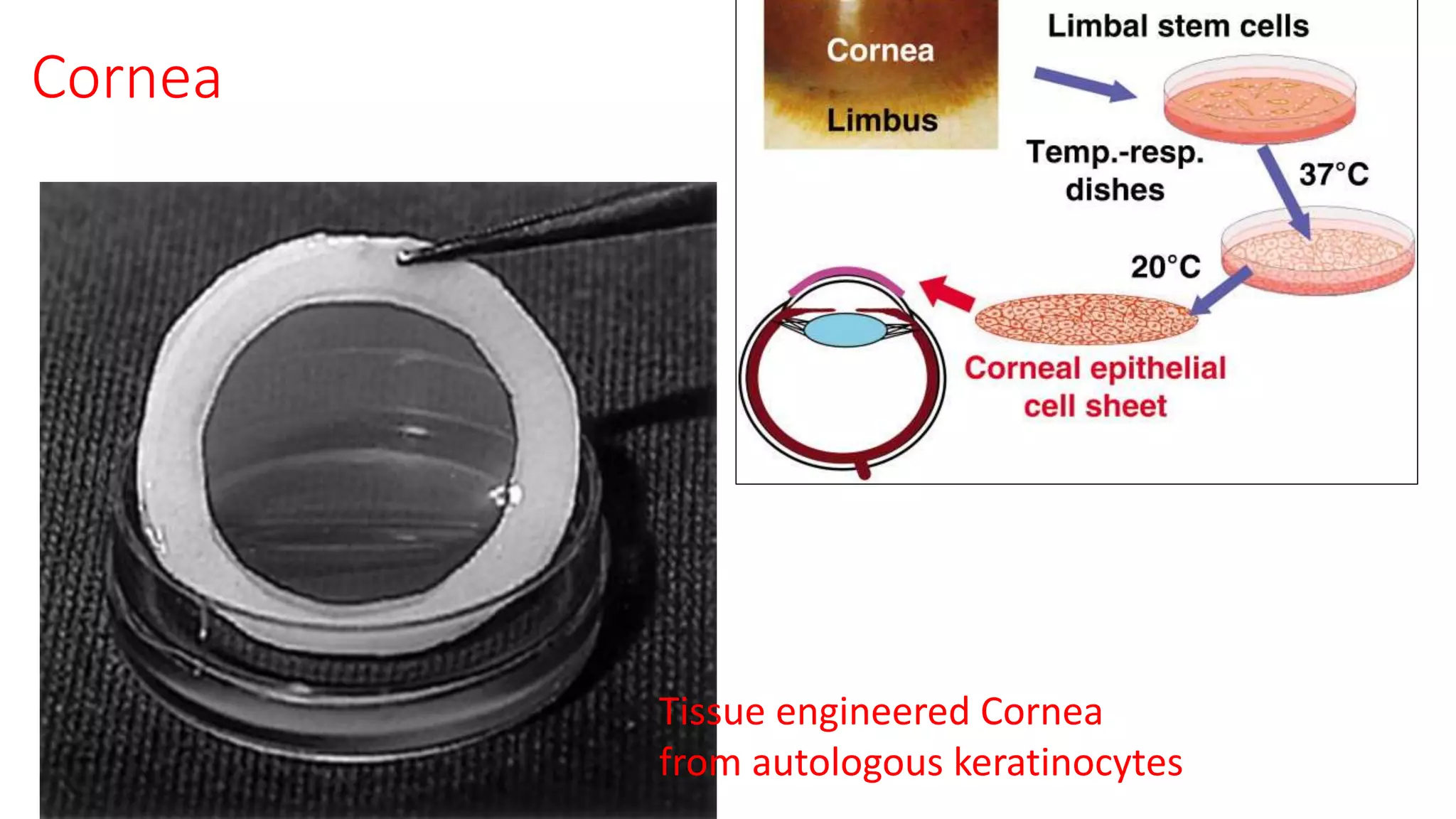
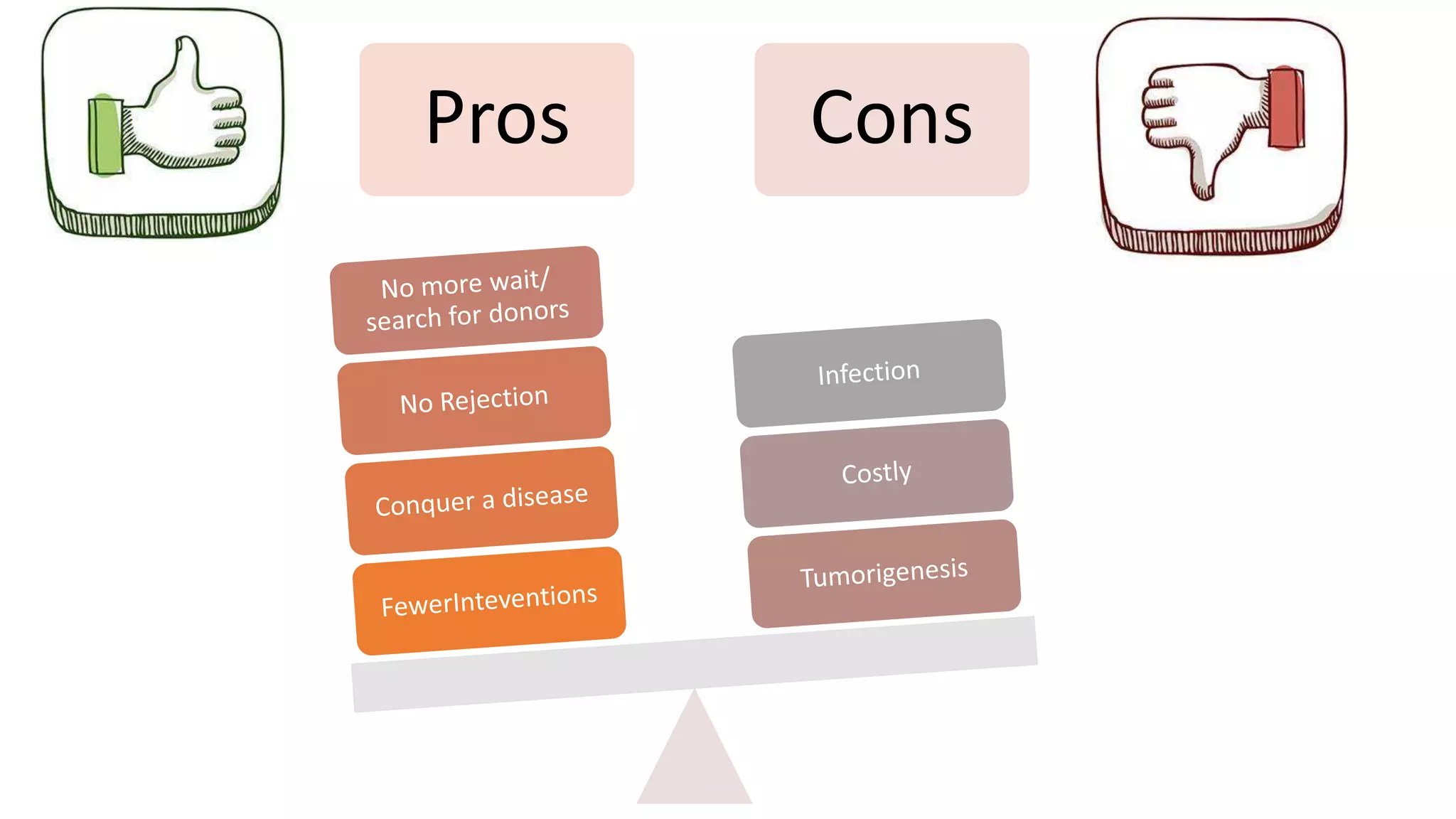
Tissue engineering and regenerative medicine aim to regenerate human tissues and organs. Tissue engineering involves seeding cells onto scaffolds to create tissues, while regenerative medicine focuses on cell therapies. The field is multidisciplinary and requires collaboration across various areas. Applications have included skin, blood vessels, heart valves, cartilage, bones and whole organs. Challenges remain around ethics, quality control, understanding tissue differentiation, and meeting clinical demand. While still early, the field is making progress in translating technologies to treat conditions like burns, heart disease, arthritis and diabetes.