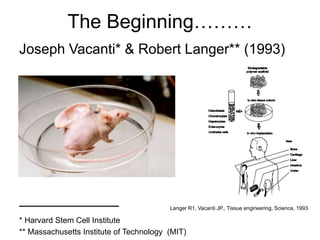
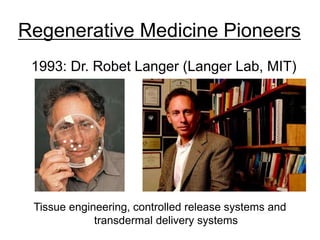
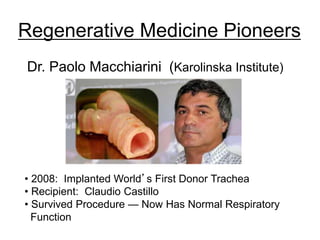
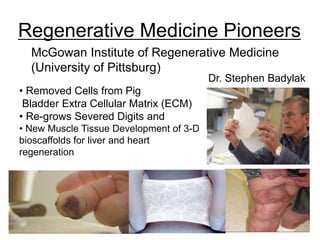
The document discusses regenerative medicine and tissue engineering, highlighting the importance of scaffolds in developing biological substitutes for damaged tissues. It outlines the challenges faced in this field, including biomaterial design, cell sourcing, and vascularization, while emphasizing the role of nanotechnology and microfluidics in enhancing scaffold fabrication. Additionally, it references pioneering efforts and innovative developments in organ and tissue engineering by various research institutions and companies.

![Synthetic Scaffolds
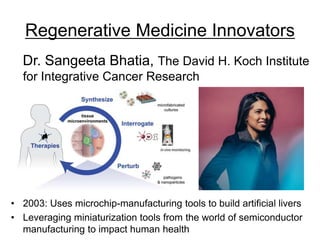
[Lecture: Sangeeta Bhatia – ‘Tiny Technologies’ and Regenerative Medicine:
stemcellassays.com/2011/04/lecture-sangeeta-bhatia-tiny-technologies-and-regenerative-medicine/]](https://image.slidesharecdn.com/tissueengineeringregenerativemedicine-150701011449-lva1-app6891/85/Tissue-Engineering-Regenerative-Medicine-16-320.jpg)
![Potential of Regenerative Medicine
Chip Technology
[Geraldine Hamilton, Body parts on a chip, TEDx Boston, June 2013:
https://youtu.be/CpkXmtJOH84]
• Reduces Need for Animal Testing
• 3-D Printed Organs on Chips Used to Test Vaccines](https://image.slidesharecdn.com/tissueengineeringregenerativemedicine-150701011449-lva1-app6891/85/Tissue-Engineering-Regenerative-Medicine-23-320.jpg)
![3-D Elastic Membrane Fits Heart’s
Epicardium
3-D Printer Creates Heart Membrane
[Prof. Igor Efimov, Washington University in St. Louish: ttps://news.wustl.edu/news/Pages/26554.aspx]
Lizhi Xu and al., Nature Communications, 2014, 3329, doi:10.1038/ncomms4329
Promise of Regenerative Medicine](https://image.slidesharecdn.com/tissueengineeringregenerativemedicine-150701011449-lva1-app6891/85/Tissue-Engineering-Regenerative-Medicine-24-320.jpg)
![R&D Trends, Innovation and
Pioneering
[Laboratory for Multiscale Regenerative Technologies: https://lmrt.mit.edu/research]](https://image.slidesharecdn.com/tissueengineeringregenerativemedicine-150701011449-lva1-app6891/85/Tissue-Engineering-Regenerative-Medicine-25-320.jpg)
![Dr. Ali Khademhosseini (Wyss Institute at Harvard)
[MIT Technology Review: www2.technologyreview.com/tr35/profile.aspx?TRID=610]
• 2007: Creating living tissues
• Organs in the lab
Regenerative Medicine Pioneers](https://image.slidesharecdn.com/tissueengineeringregenerativemedicine-150701011449-lva1-app6891/85/Tissue-Engineering-Regenerative-Medicine-29-320.jpg)


![Regenerative Medicine Innovators
Dr. Ramille N. Shah (Northwestern Univ.)
• 2011: Leader in Field of 3D-Printable Materials
• Engineers new 3D-Inks
• Creates Porous Scaffolds
• Technique: Additive Manufacturing
(Nanofiber Scaffold For
Cartilage Regeneration)
[Center for Regenerative Nanomedicine, Northwestern University:
rn.northwestern.edu/projects/peptide-amphiphile-polymer-hybrids-articular-cartilage-
regeneration]
Peptide amphiphile
nanofiber hybrid scaffolds
will be created using 3D
bioprinting technology](https://image.slidesharecdn.com/tissueengineeringregenerativemedicine-150701011449-lva1-app6891/85/Tissue-Engineering-Regenerative-Medicine-34-320.jpg)