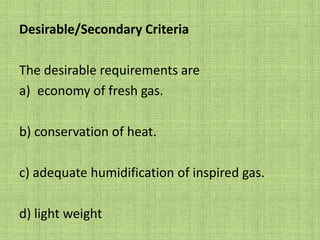
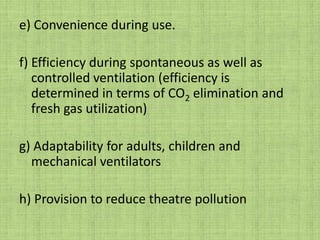
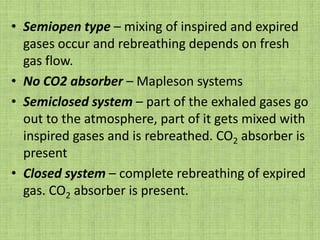
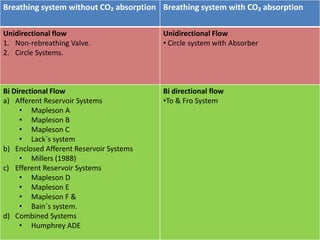
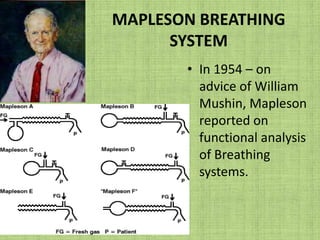
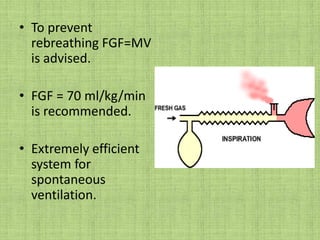
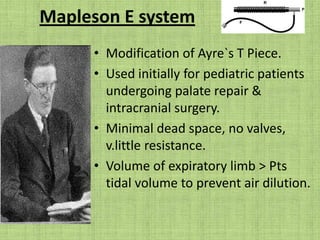
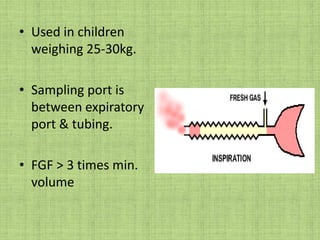
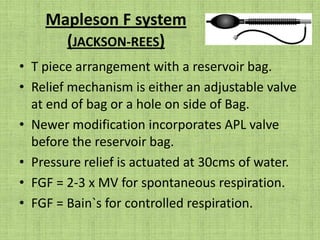
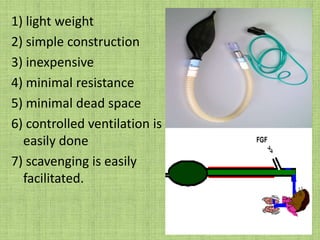
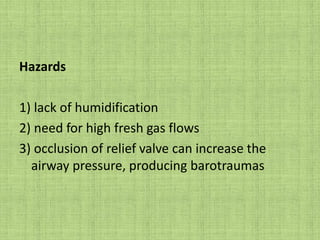
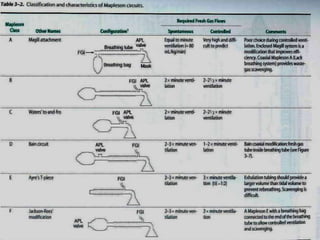
This document summarizes the history and components of breathing systems used in anesthesiology. It discusses the evolution of breathing circuits from early simple open systems to more advanced closed and semi-closed systems incorporating reservoirs, valves, filters and CO2 absorbers. Key systems are described, including Mapleson classifications and the Magill circuit. The essential criteria of an ideal breathing system and desirable secondary criteria are also outlined.