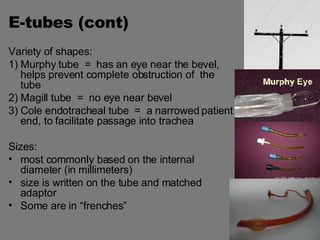
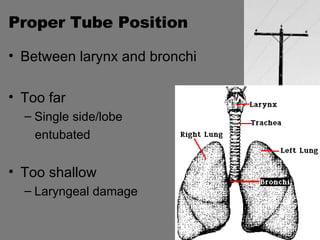
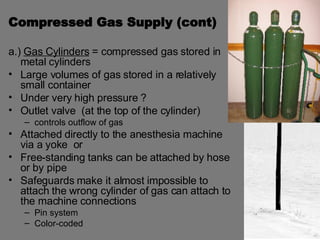
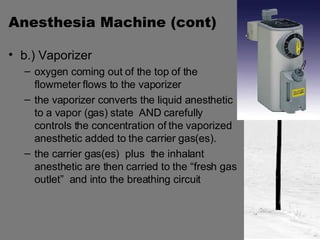
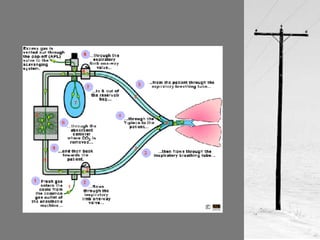
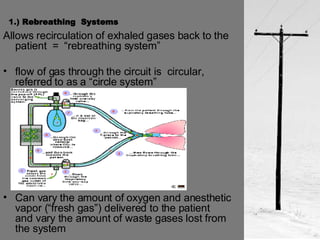
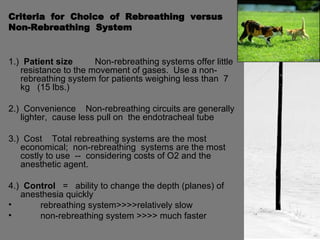
This document summarizes different types of anesthetic equipment used in veterinary medicine, including endotracheal tubes, anesthetic machines, breathing circuits, and their components and functions. It discusses the purpose and properties of endotracheal tubes, vaporizers and their role in delivering anesthetic agents, and how breathing circuits carry gases to and from the patient using rebreathing or non-rebreathing systems. Key factors that influence the function of vaporizers and the choice of breathing circuit are also outlined.