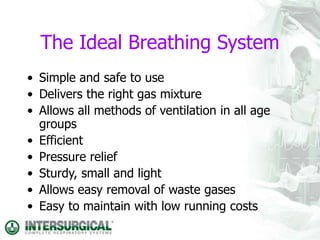
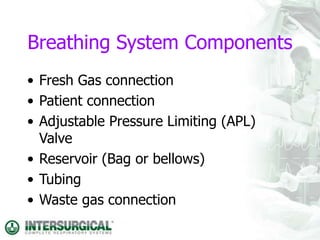
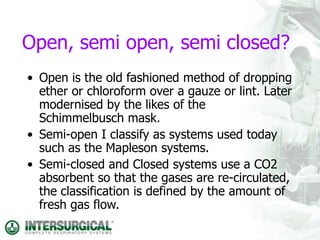
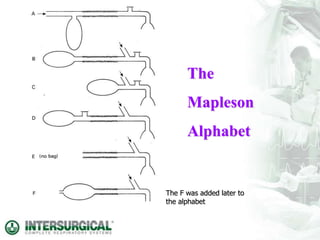
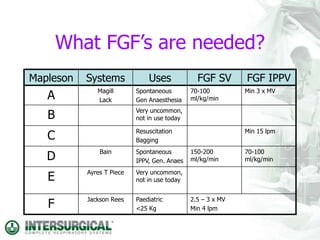
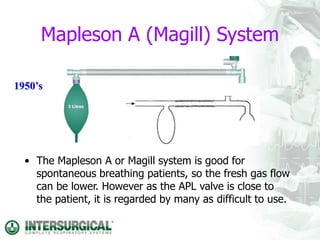
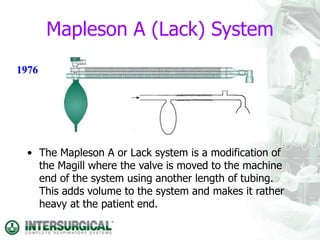
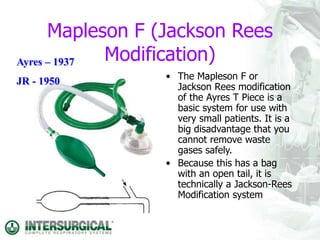
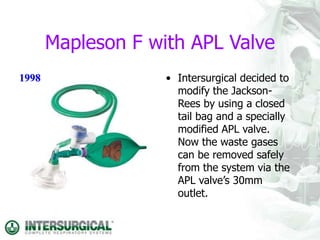
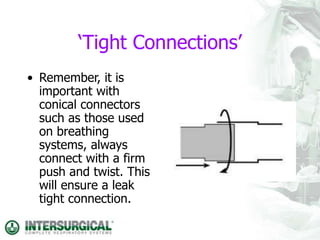
This document discusses different types of breathing systems used in anaesthesia. It describes the components and ideal properties of breathing systems. Open, semi-open, and semi-closed systems are defined. Several specific semi-open systems are outlined, including the Mapleson A, D, F systems. Semi-closed systems require CO2 absorbents and lower fresh gas flows than open systems. Types of semi-closed systems are also defined. The document emphasizes the importance of ensuring tight connections between breathing system components.