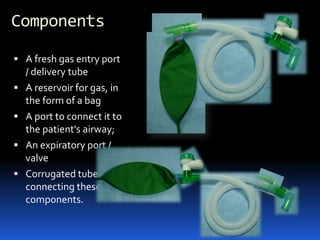
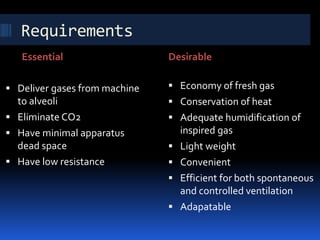
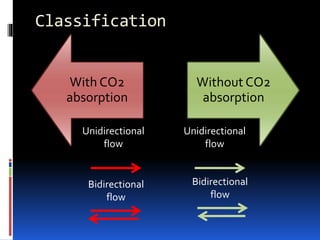
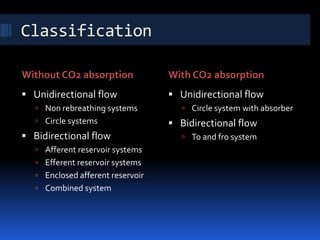
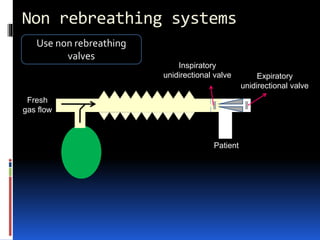
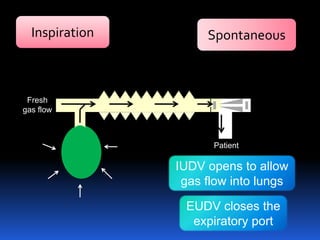
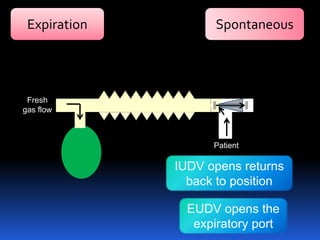
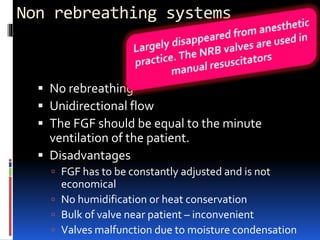
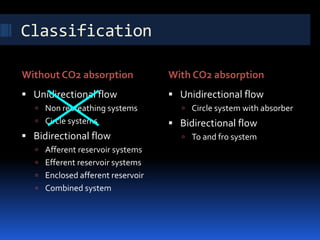
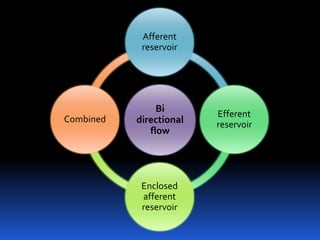
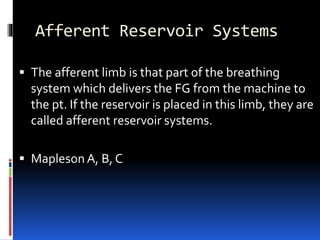
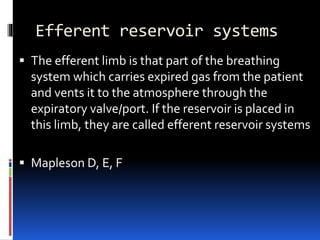
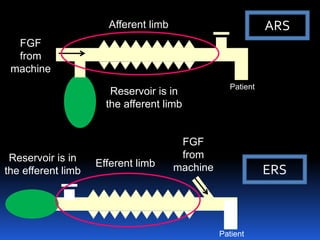
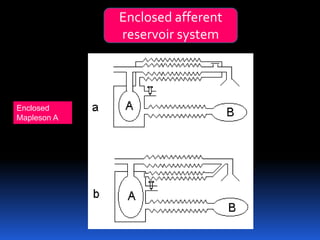
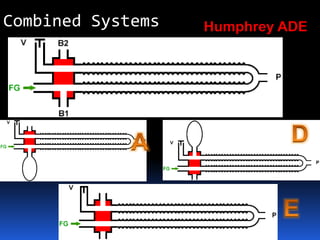
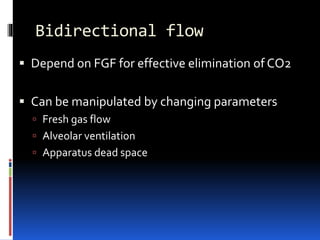
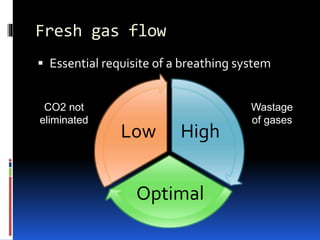
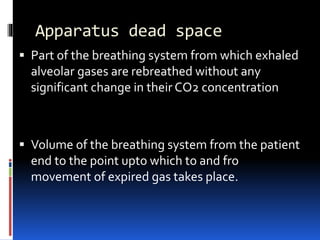
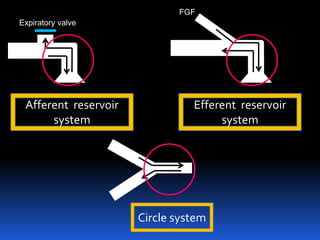
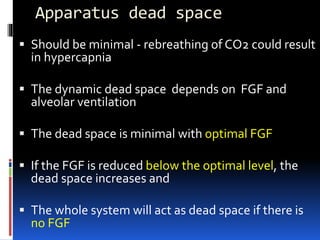
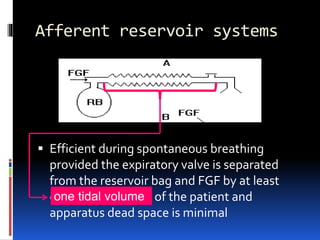
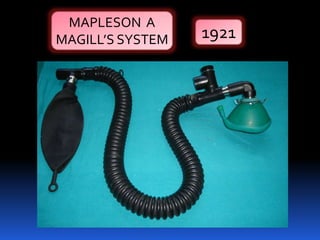
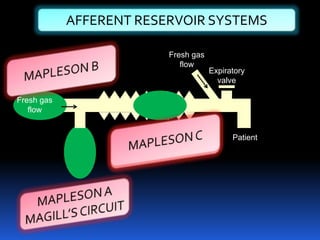
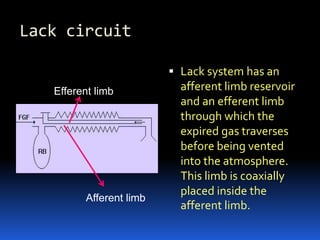
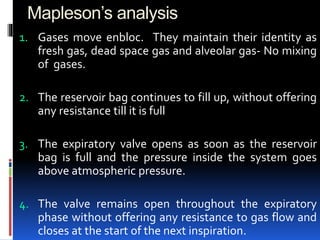
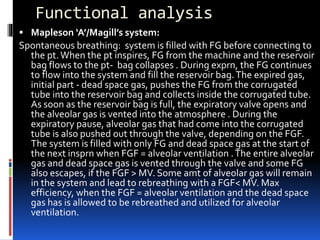
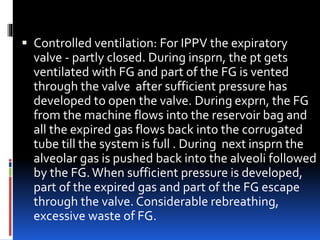
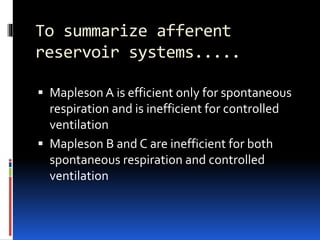
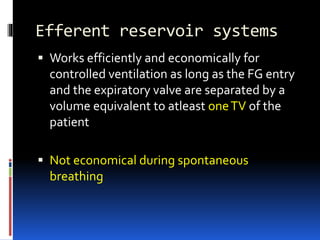
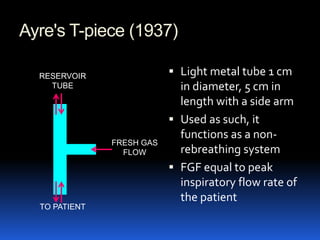
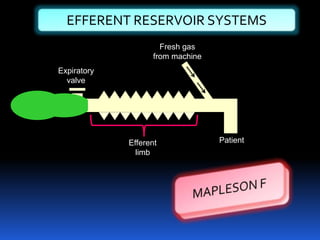
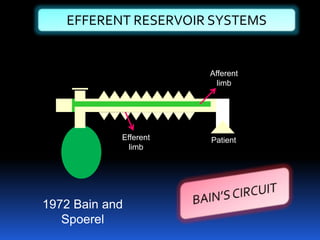
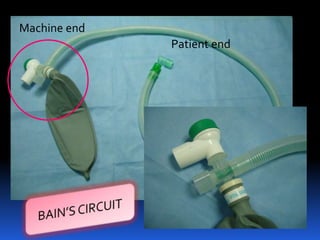
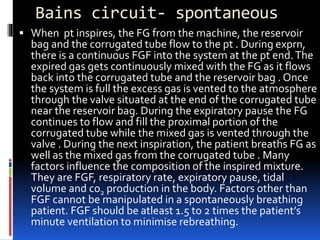
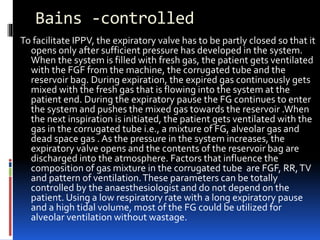
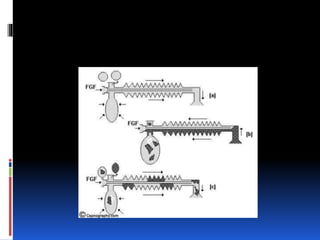
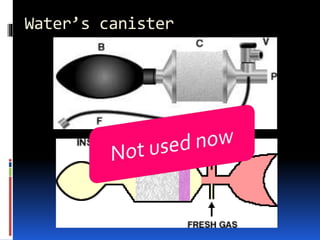
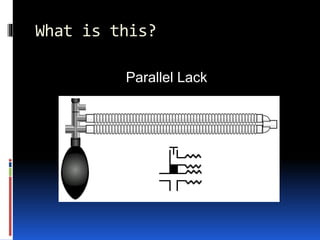
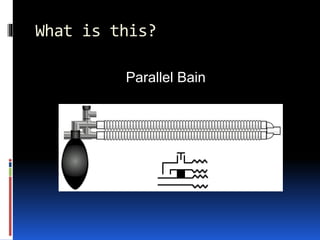
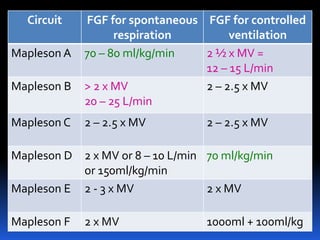
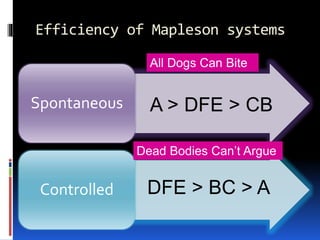
A breathing system connects the patient's airway to the anesthesia machine, creating an artificial atmosphere for breathing. It has components like a fresh gas entry port, reservoir bag, patient connection port, and expiratory port. Breathing systems are classified based on gas flow direction and whether they absorb carbon dioxide. Common systems include the non-rebreathing system, circle system, and Bain circuit. The optimal fresh gas flow depends on the system and whether ventilation is spontaneous or controlled. Proper functioning relies on minimizing apparatus dead space and balancing the fresh gas flow with alveolar ventilation.