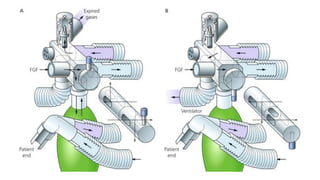
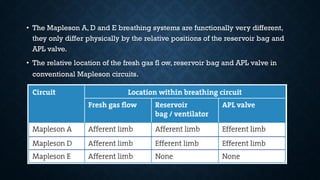
This document discusses various types of breathing systems used in anesthesia including open, semi-open, semi-closed and closed systems. It provides details on common breathing systems such as the circle system, Mapleson classifications A-F, Bain system and Jackson-Rees modification. The ideal properties of a breathing system are also listed.