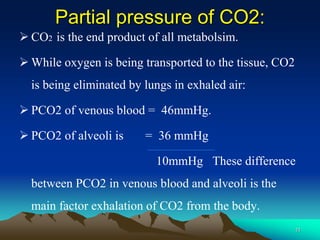
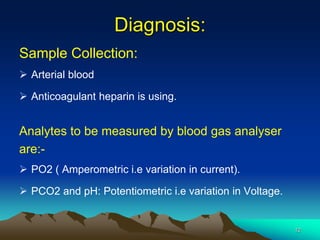
This document discusses blood gas analysis, which measures oxygen (PO2) and carbon dioxide (PCO2) levels in blood. Respiration involves pulmonary ventilation, diffusion of gases in the alveoli and blood, transport of O2 and CO2 to and from cells, and regulation of the process. O2 is crucial for ATP production through cellular respiration, while CO2 is the end product. Factors like alveolar surface area and diffusion rate impact PO2 levels. Arterial blood samples are collected and analyzed using electrodes to measure current (for PO2) or voltage (for PCO2 and pH). The results provide information about respiratory function and disorders.