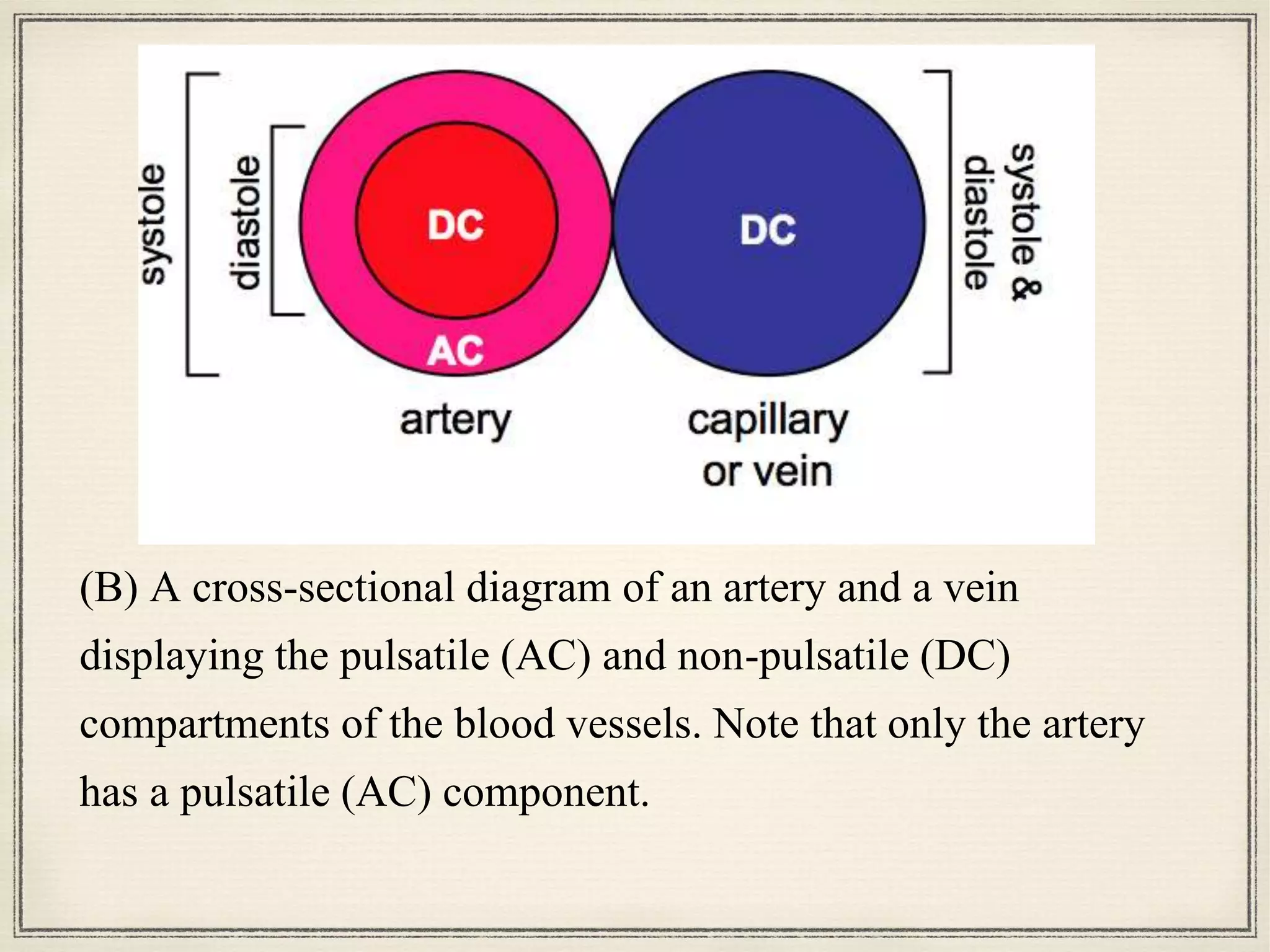
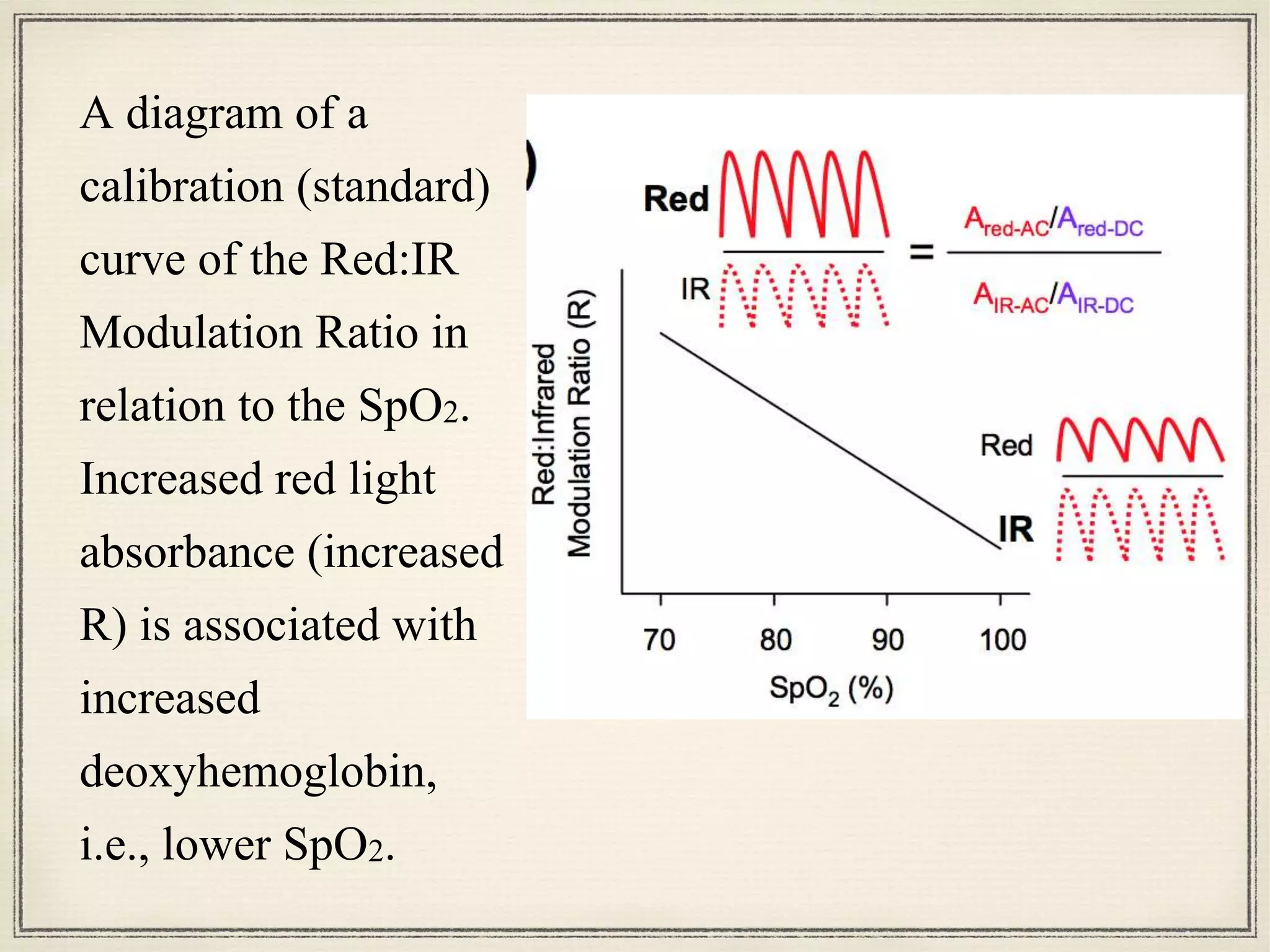
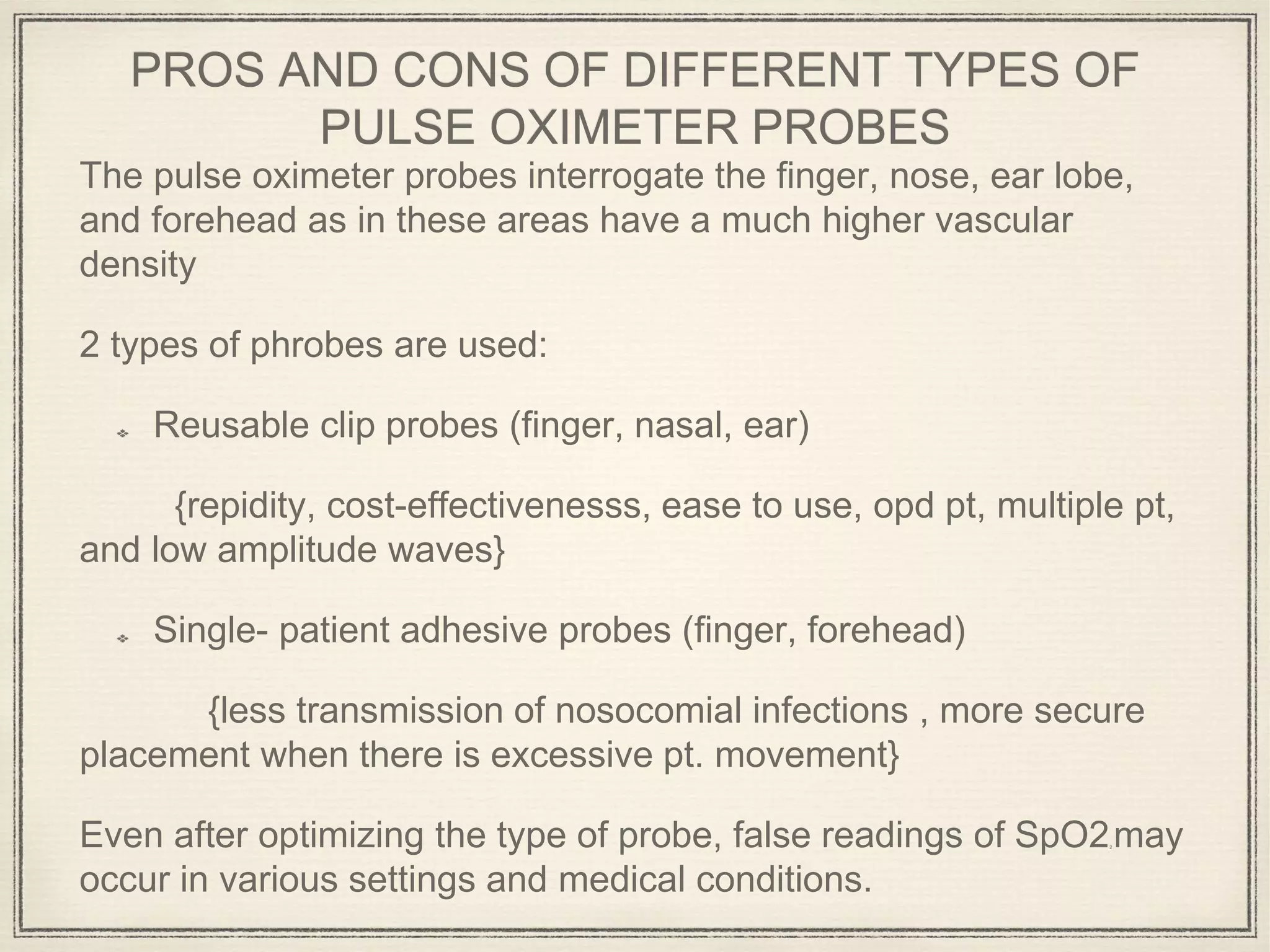
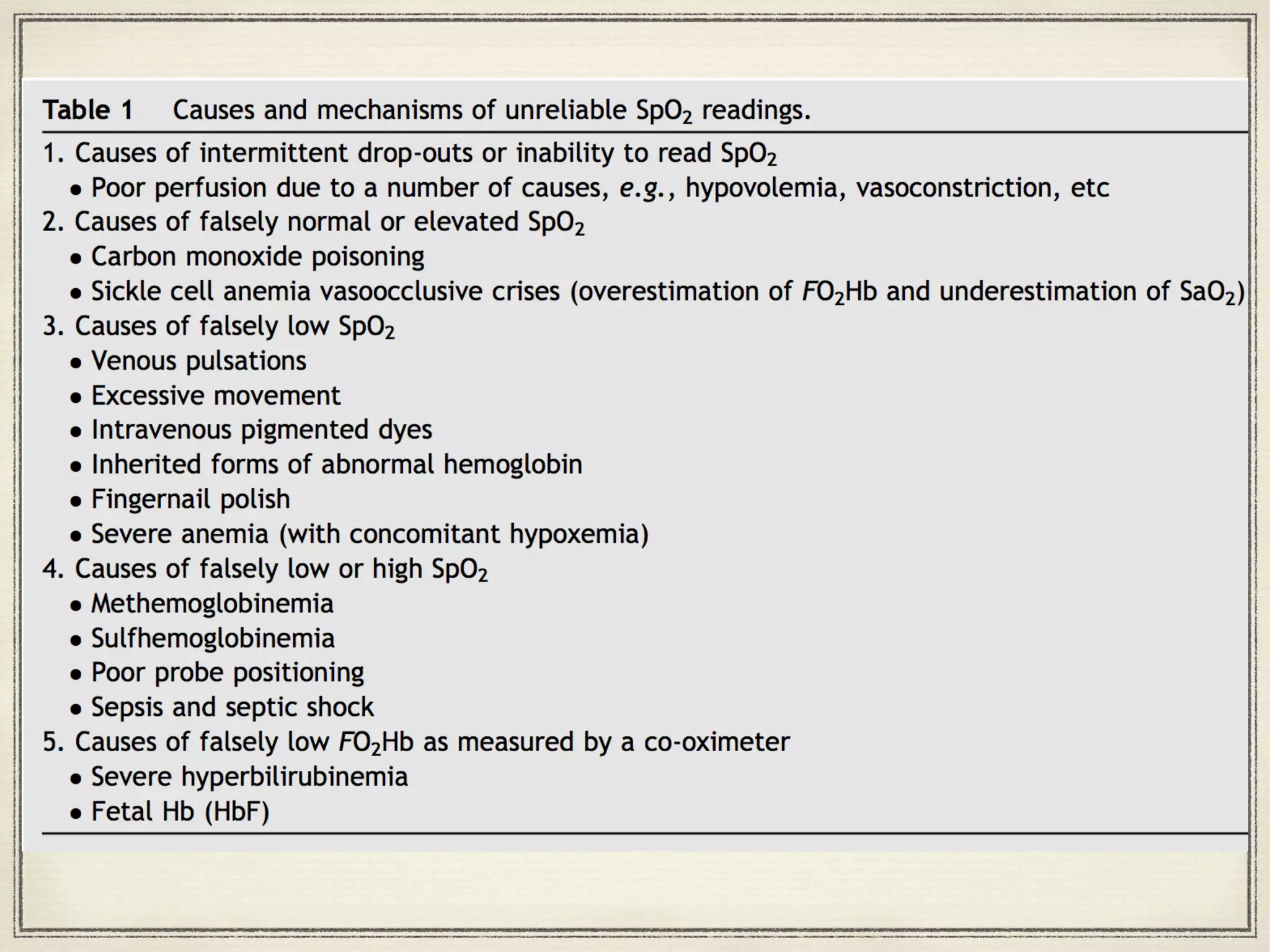
Pulse oximetry uses light absorption properties of oxyhemoglobin and deoxyhemoglobin to measure arterial oxygen saturation (SpO2). It works by emitting red and infrared light through tissue and detecting pulsatile changes caused by arterial blood flow. However, several medical conditions can cause inaccurate readings by interfering with this optical detection process. Understanding the limitations is important to avoid clinical errors.