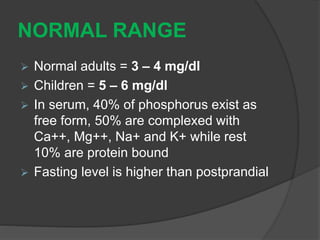
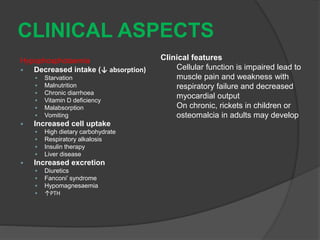
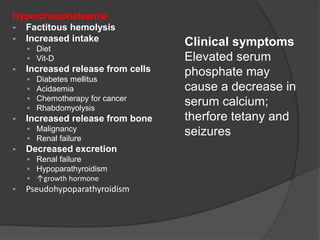
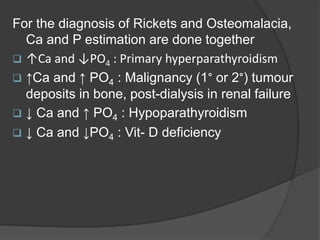
Calcium and phosphorus are essential minerals found primarily in bones and teeth. Calcium makes up 1-2% of total body weight and is found mostly in bones, while phosphorus makes up 1% of body weight and is primarily intracellular. Dietary sources of calcium include dairy products, while phosphorus is obtained from foods like cereals, meat, and nuts. Absorption of both minerals can be affected by factors like vitamin D, pH, and other dietary constituents. Calcium and phosphorus are important for bone health, cell signaling, and other metabolic processes. Abnormal levels can cause issues like muscle problems or bone diseases. Their levels are tightly regulated and measured together to diagnose certain conditions.