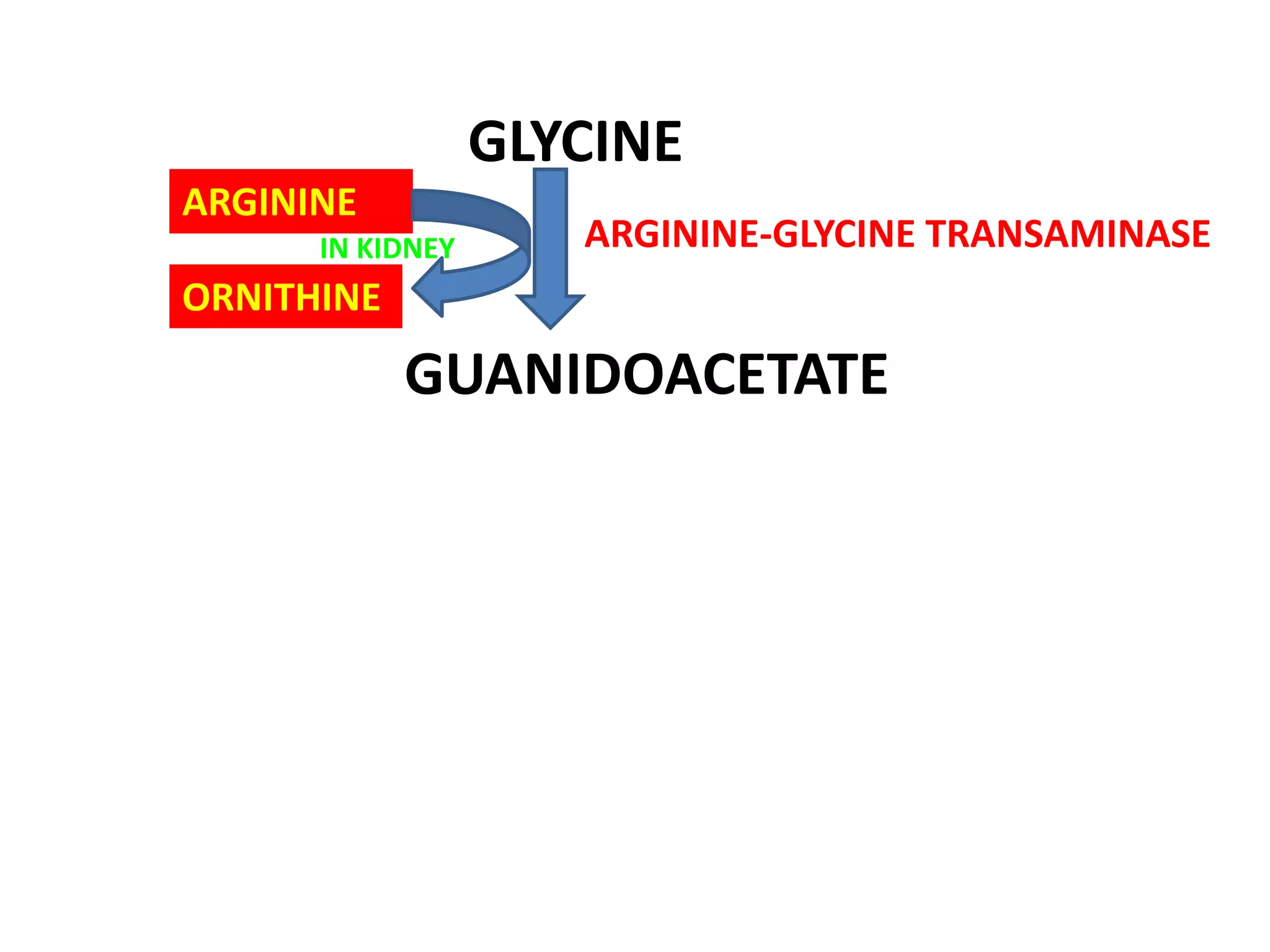
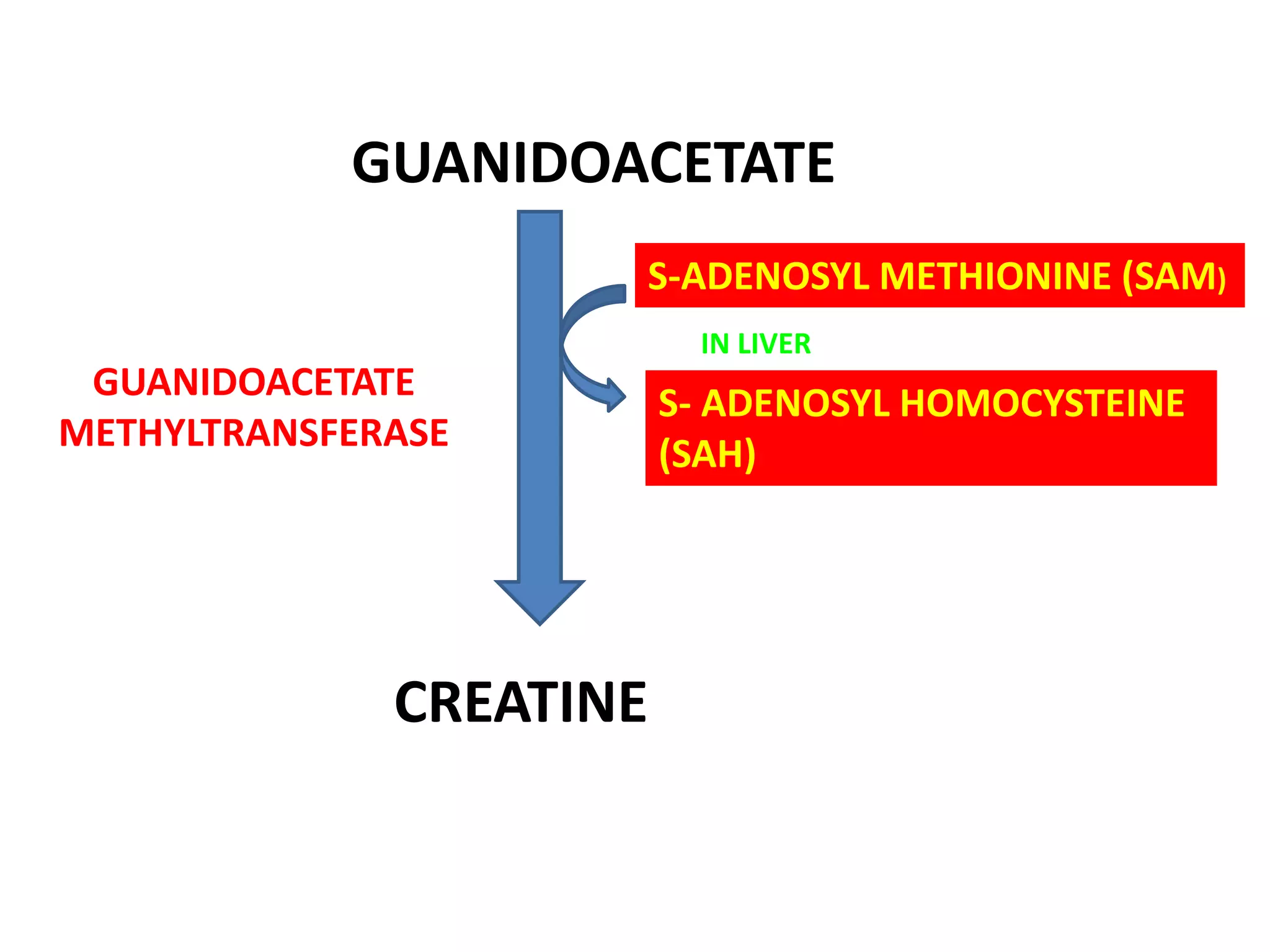
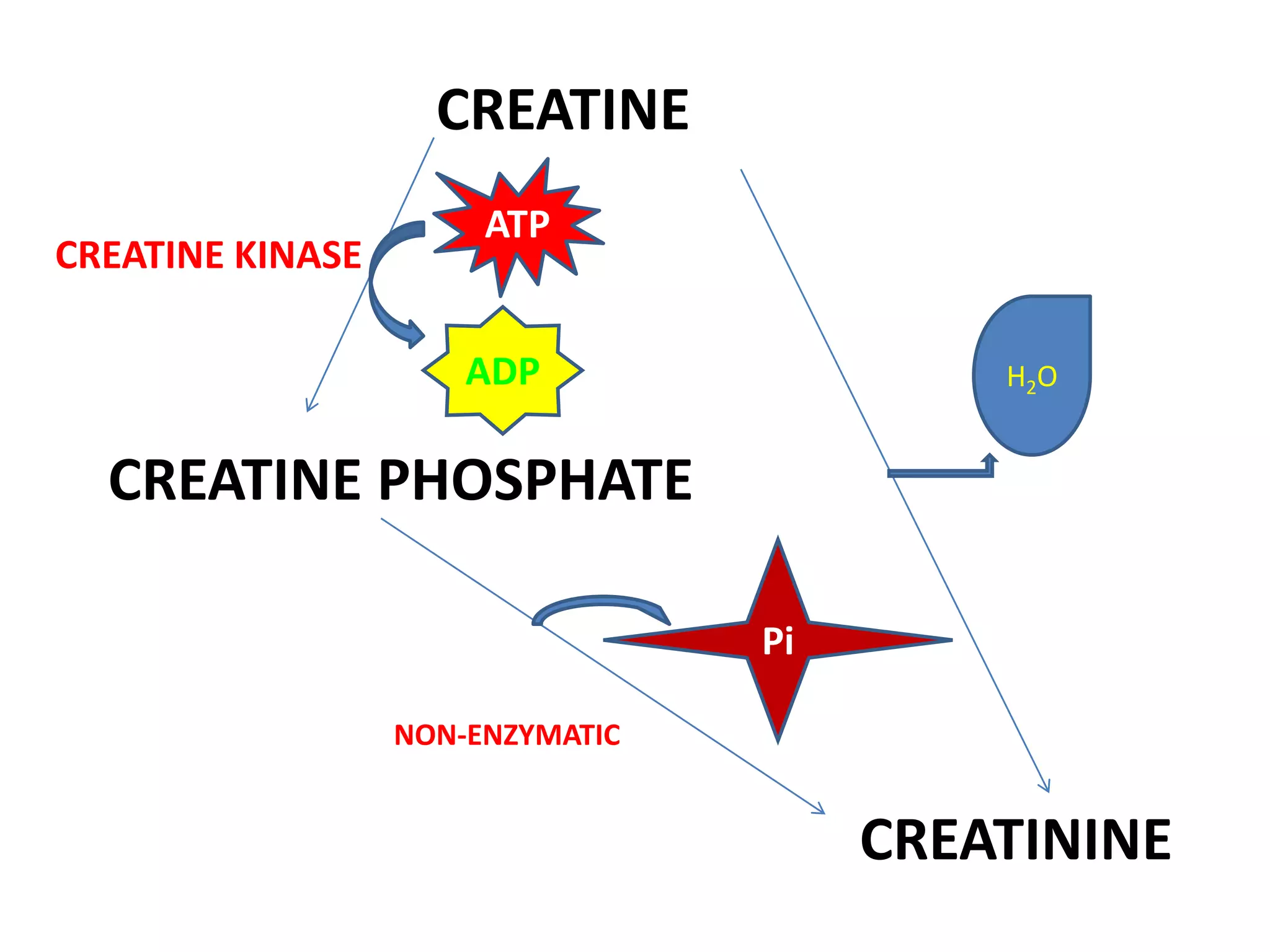
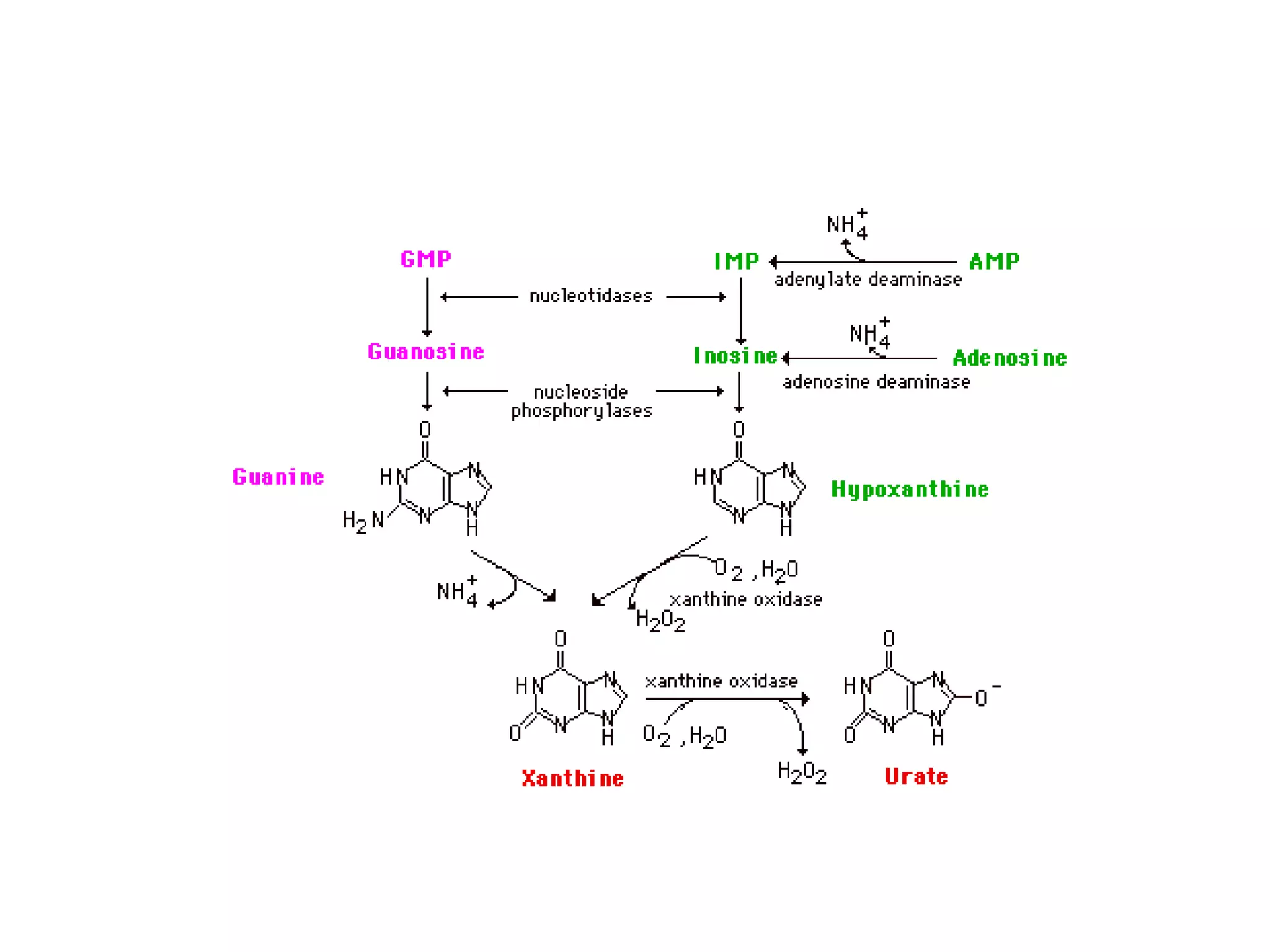
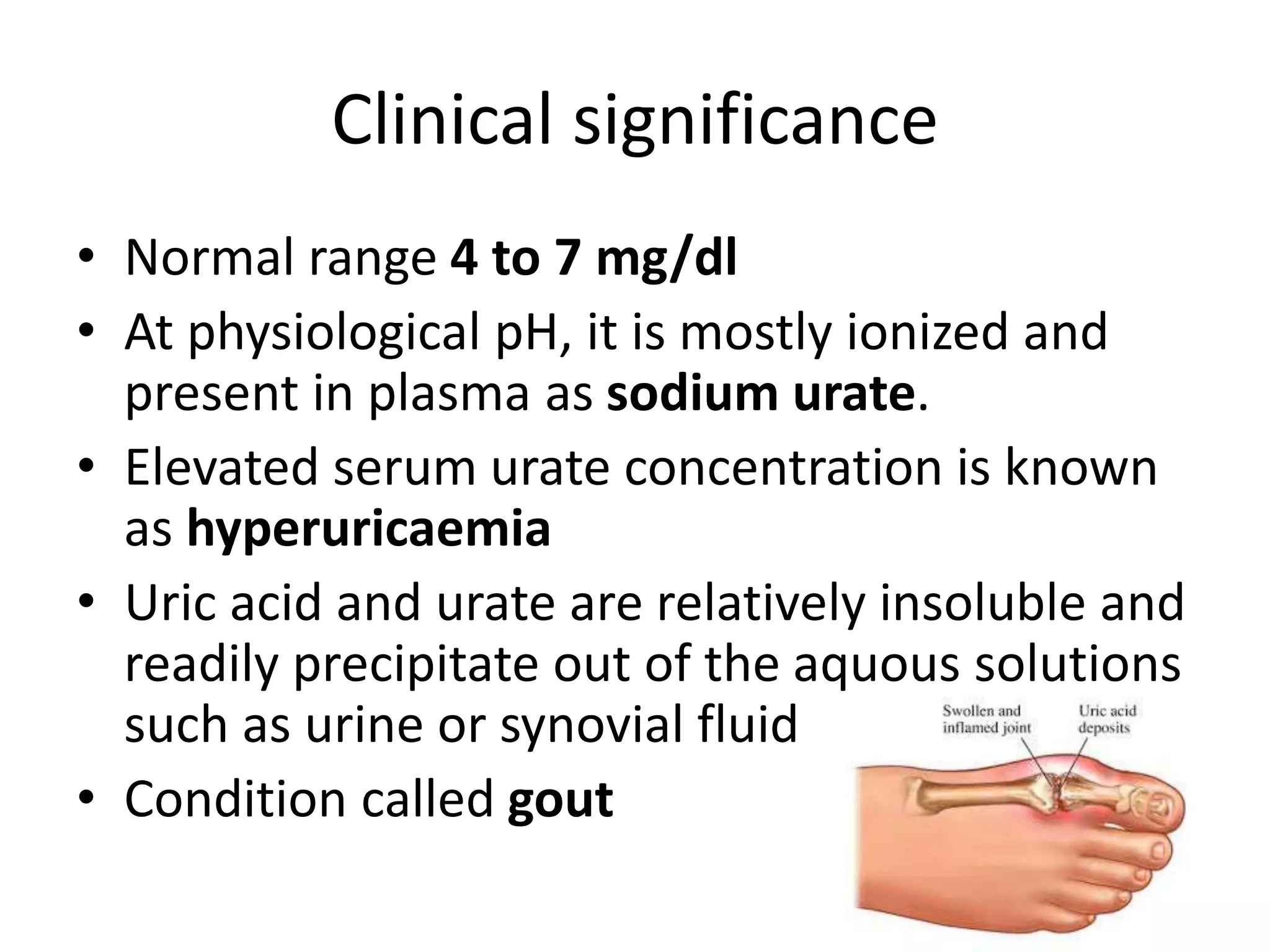
Creatinine metabolism occurs in the kidney and liver from amino acids and is stored as creatine phosphate in muscle and brain. It is normally excreted in urine. Uric acid is produced from purine metabolism and breakdown and is excreted primarily by the kidney. Elevated uric acid levels can cause gout due to precipitation of urate crystals in joints. Gout can be primary from inborn enzyme defects or secondary from other causes that increase uric acid production or decrease excretion like renal disease. Treatment involves diet modification and drugs like allopurinol.