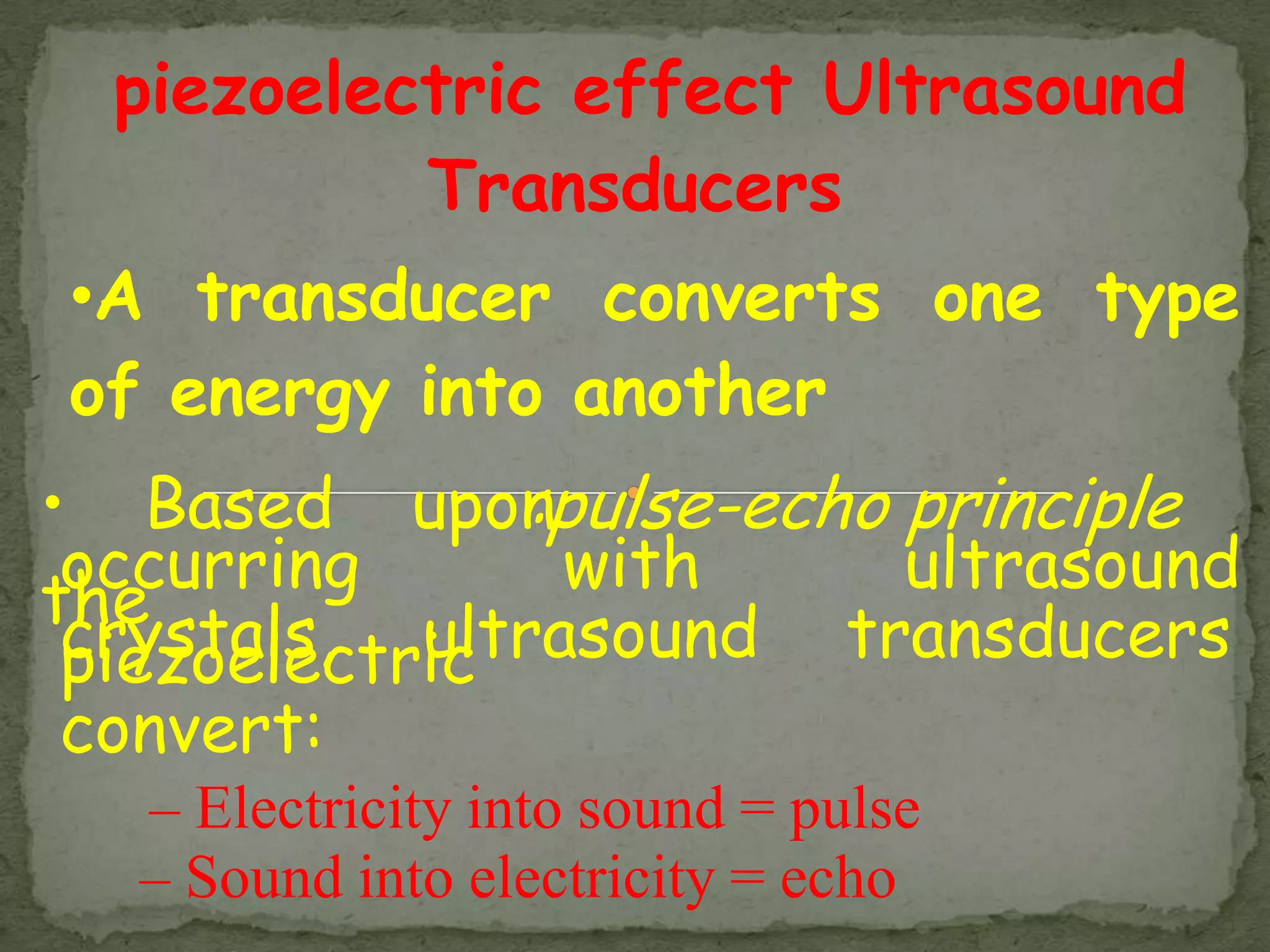
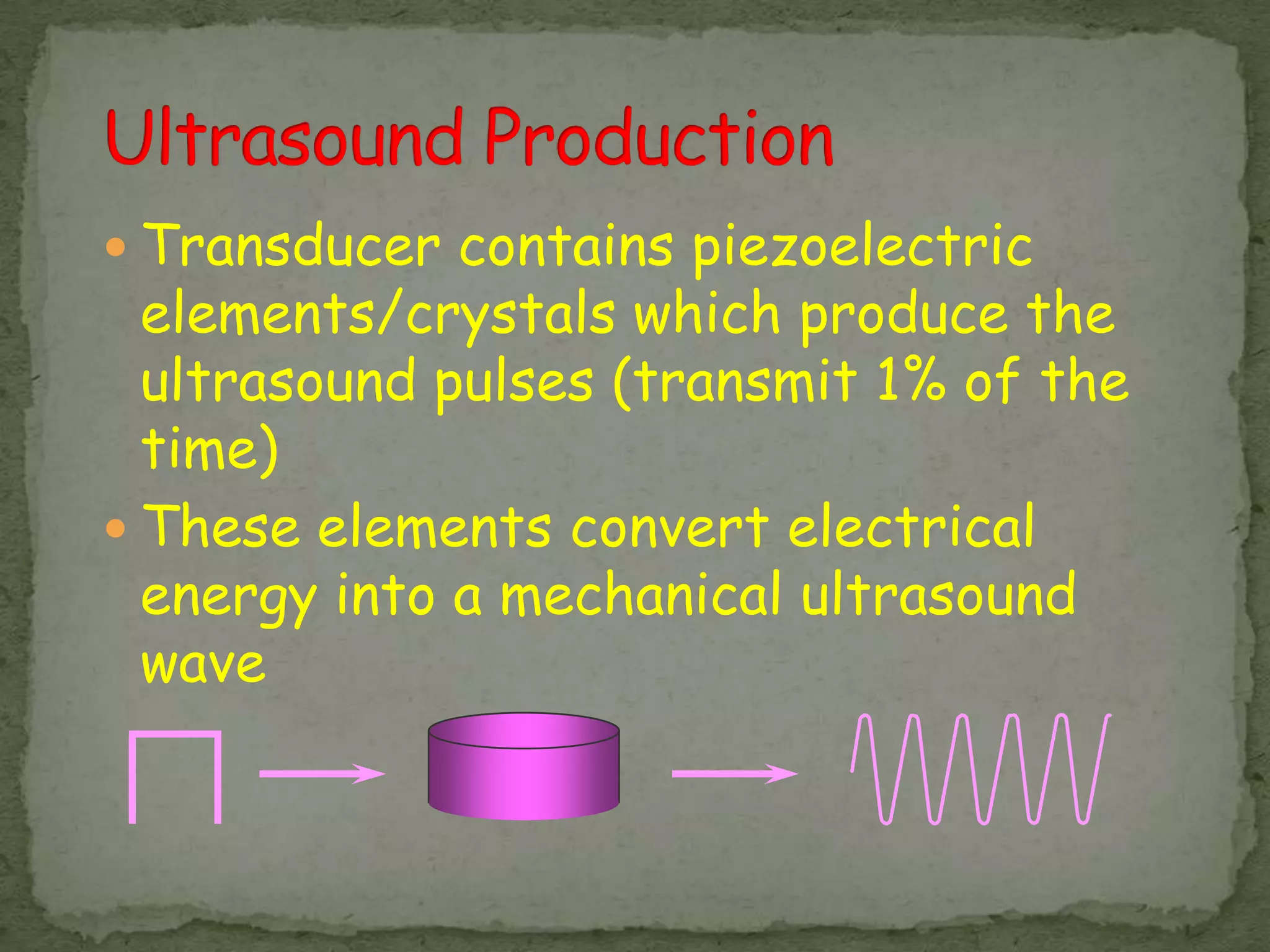
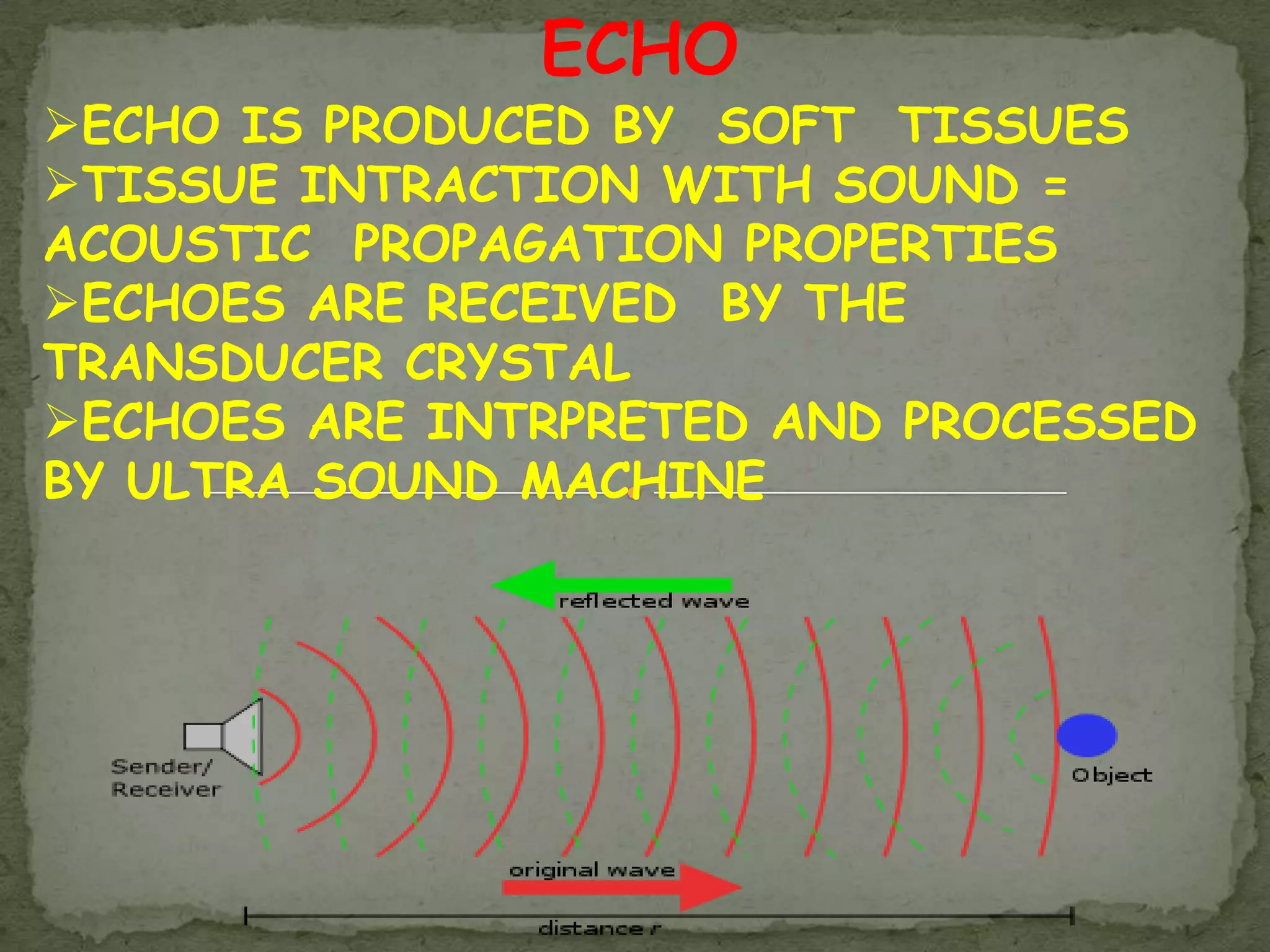
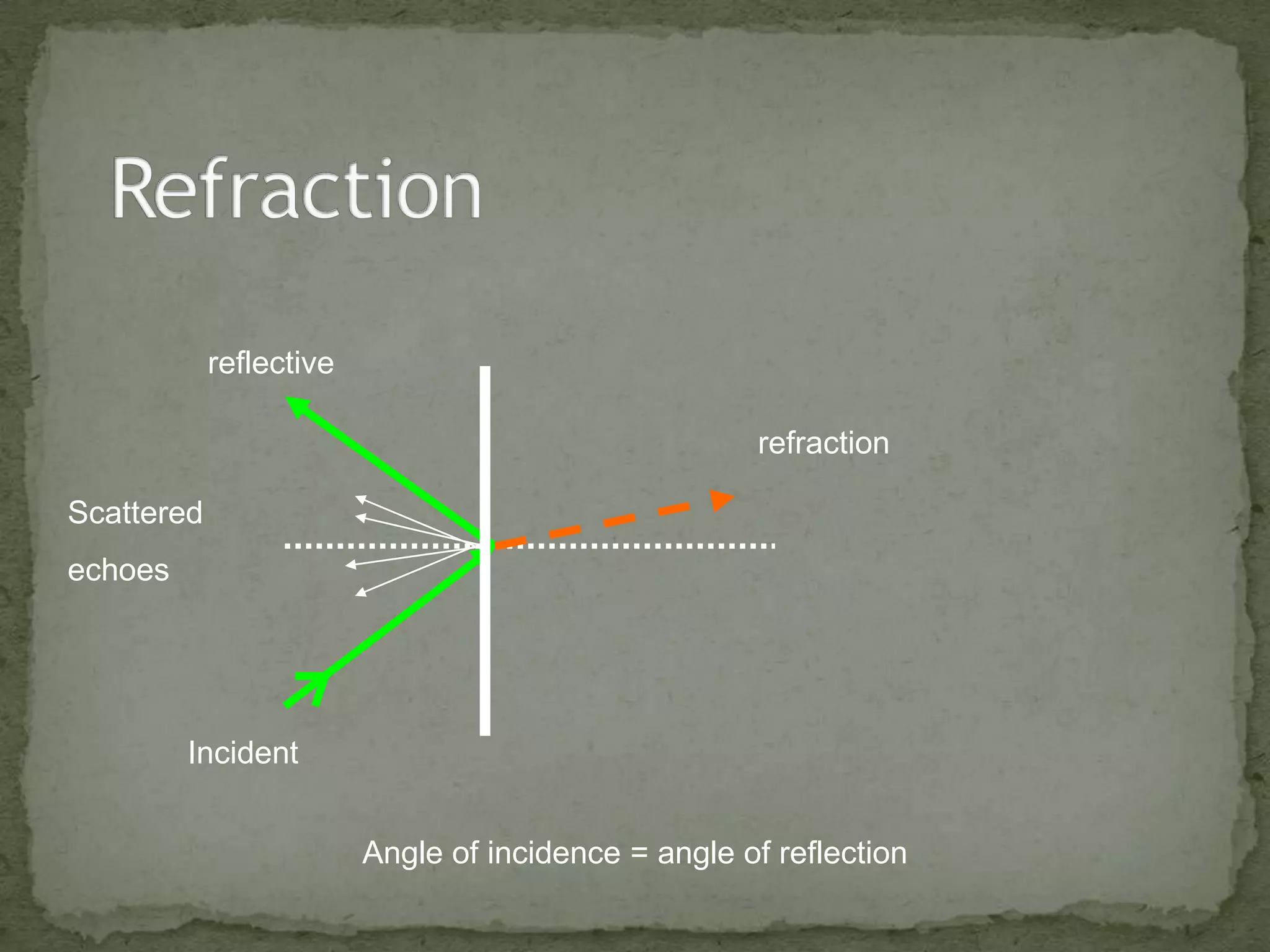
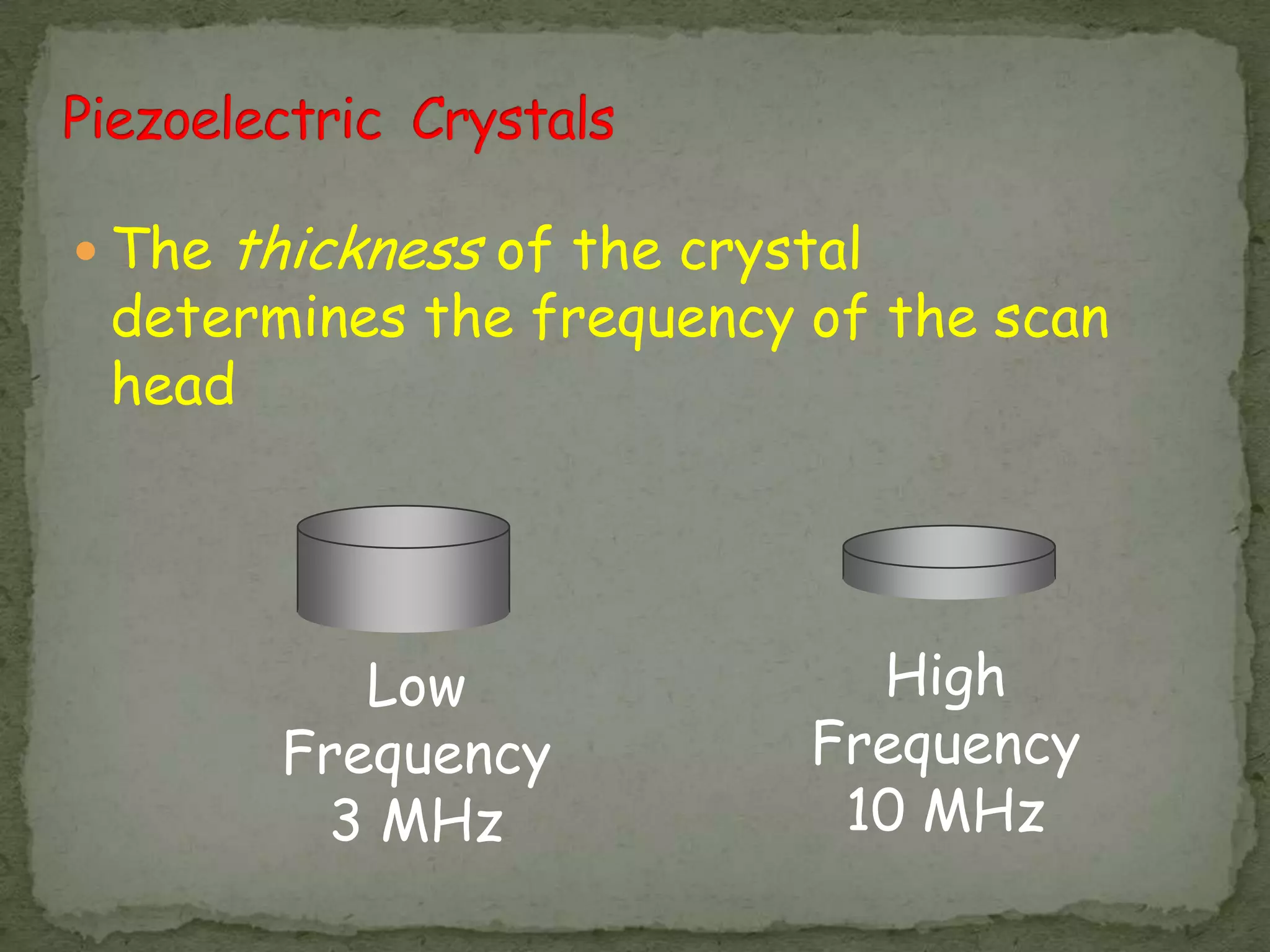
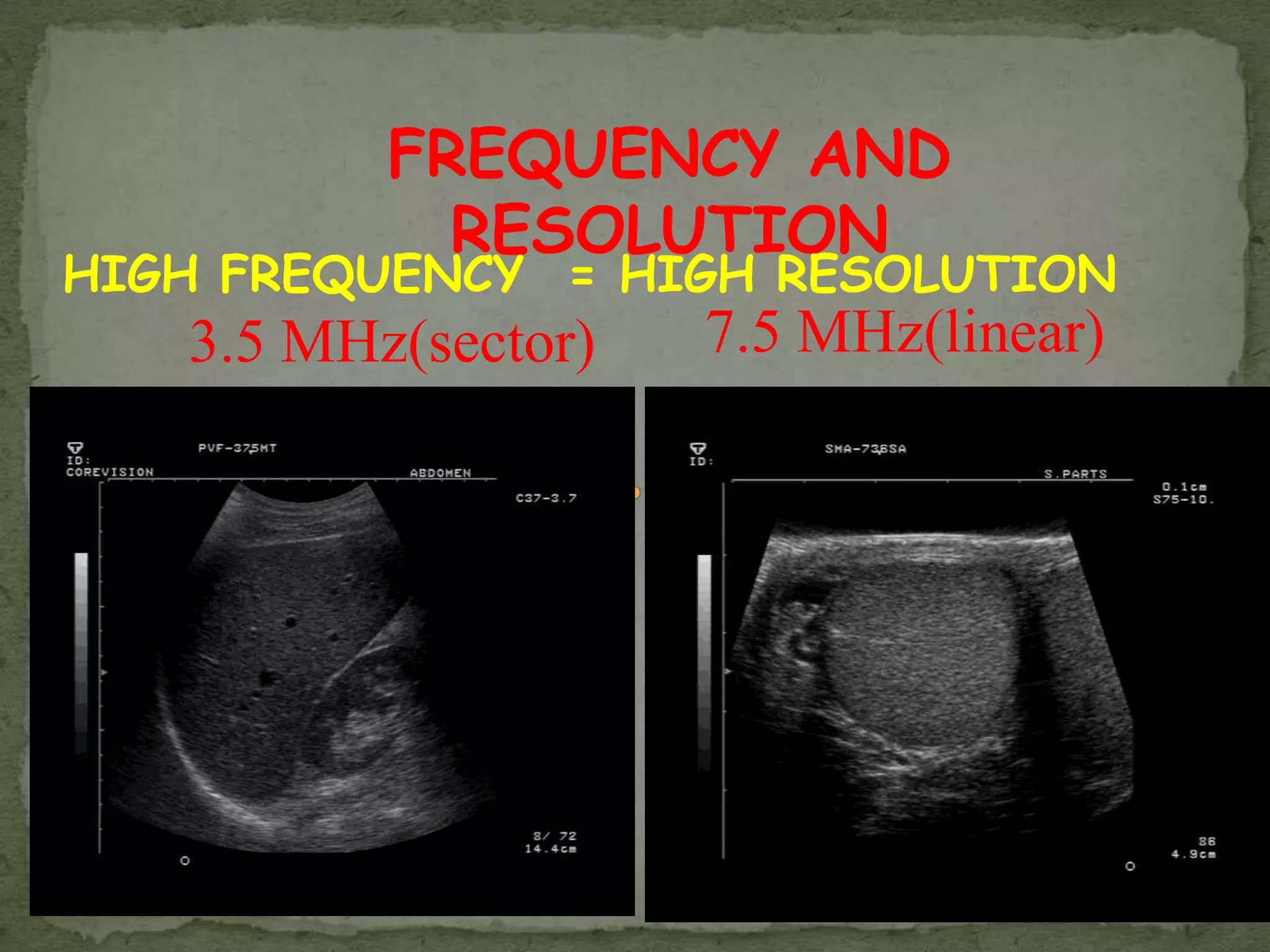
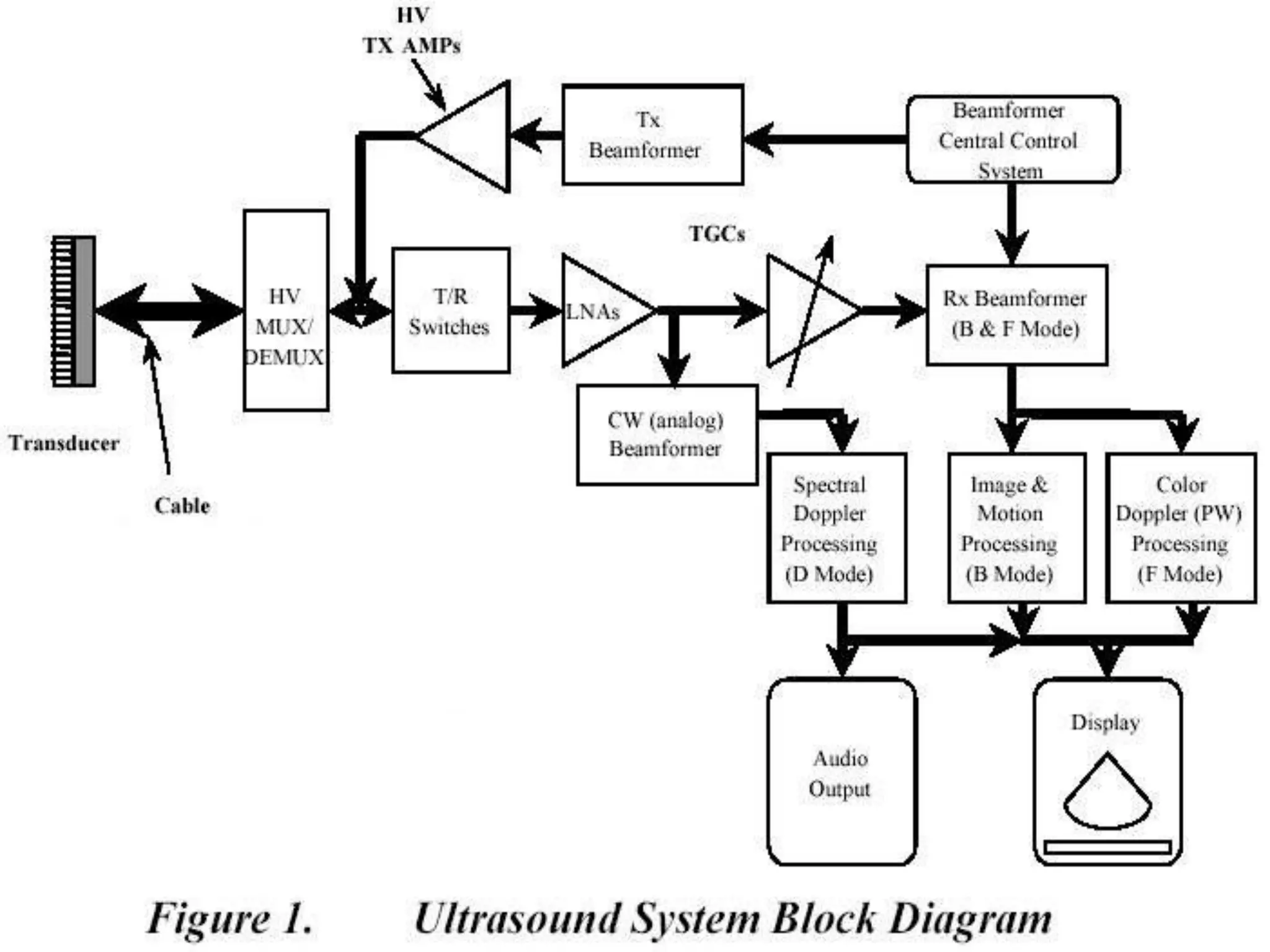
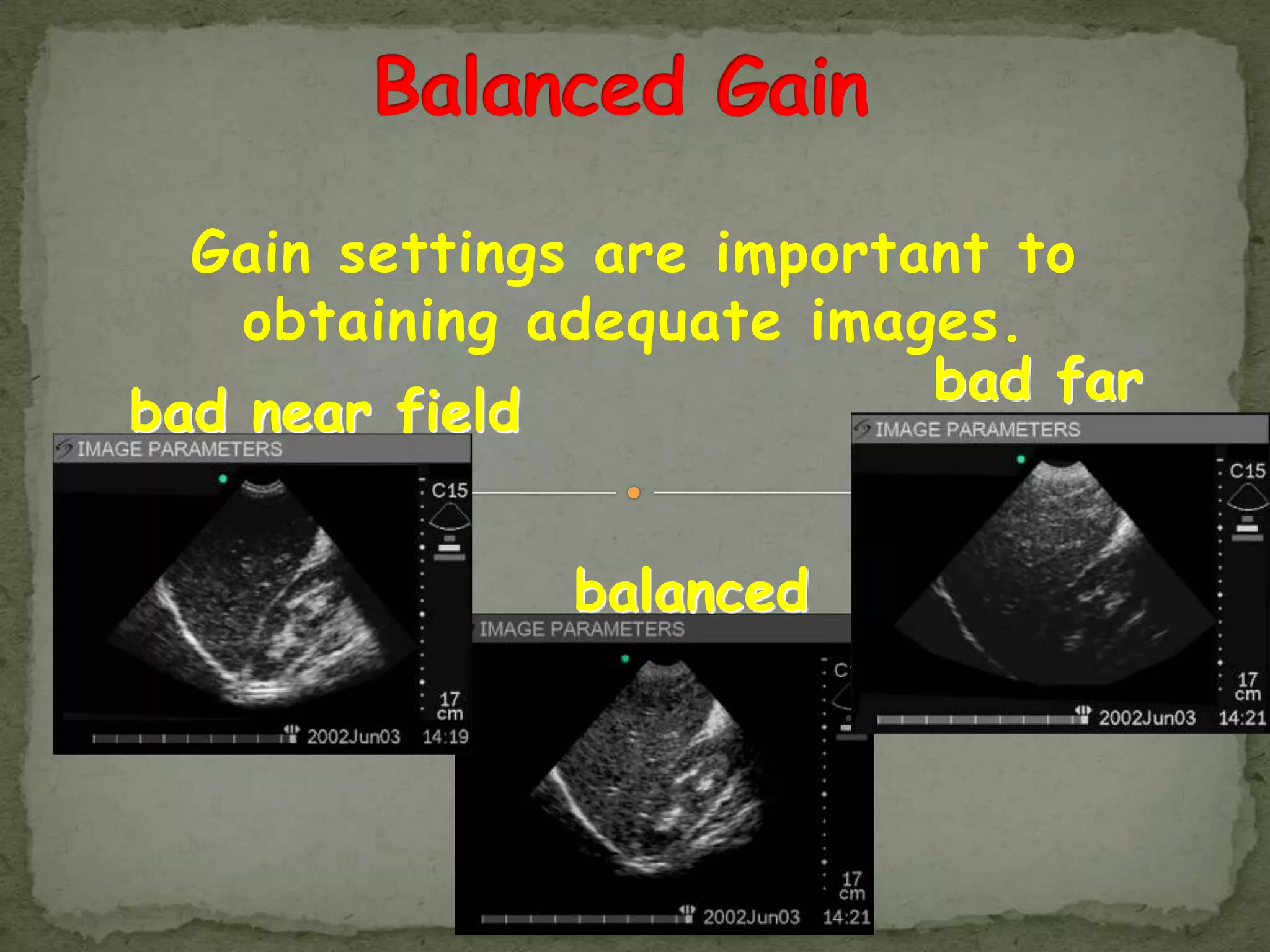
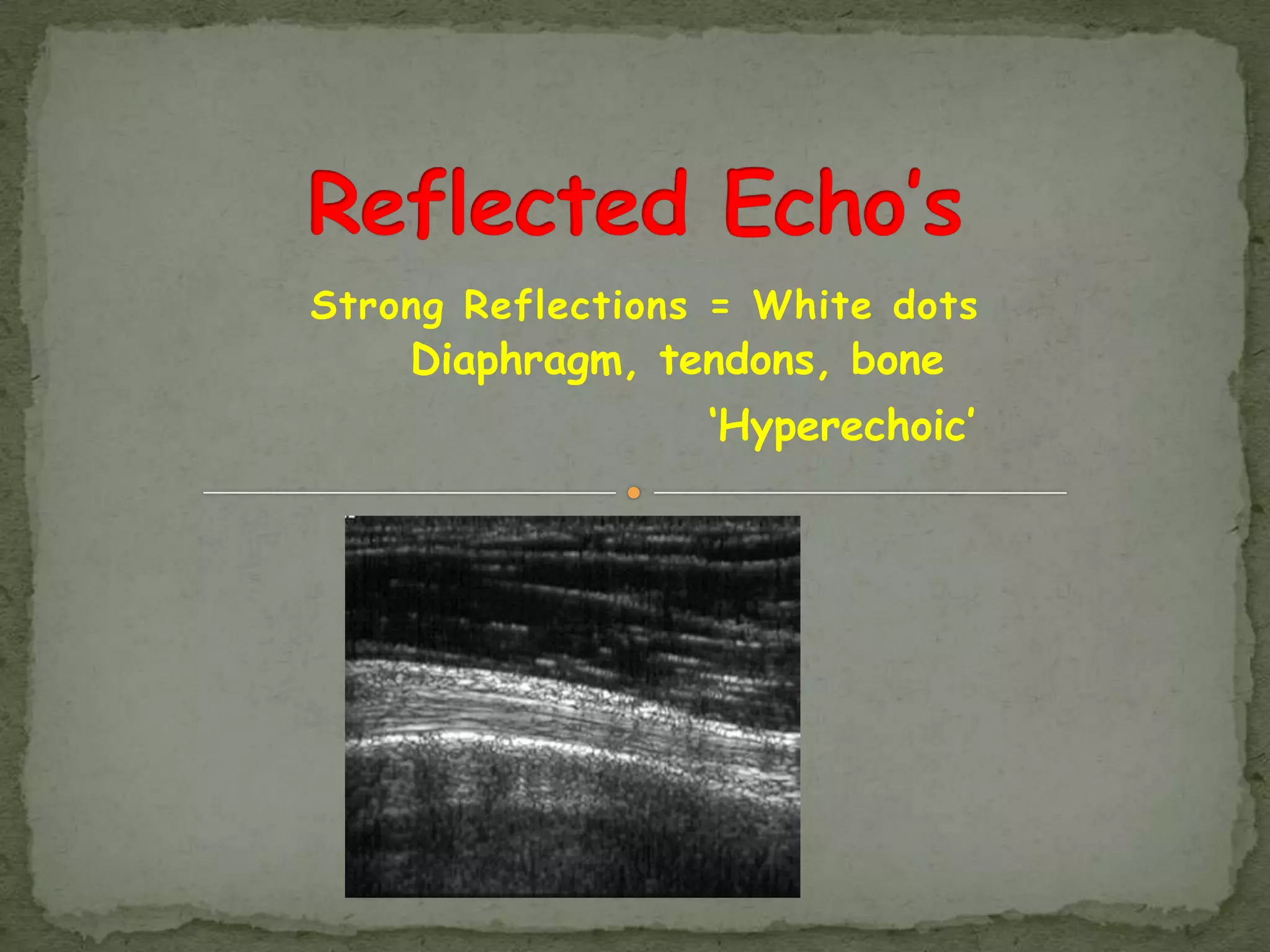
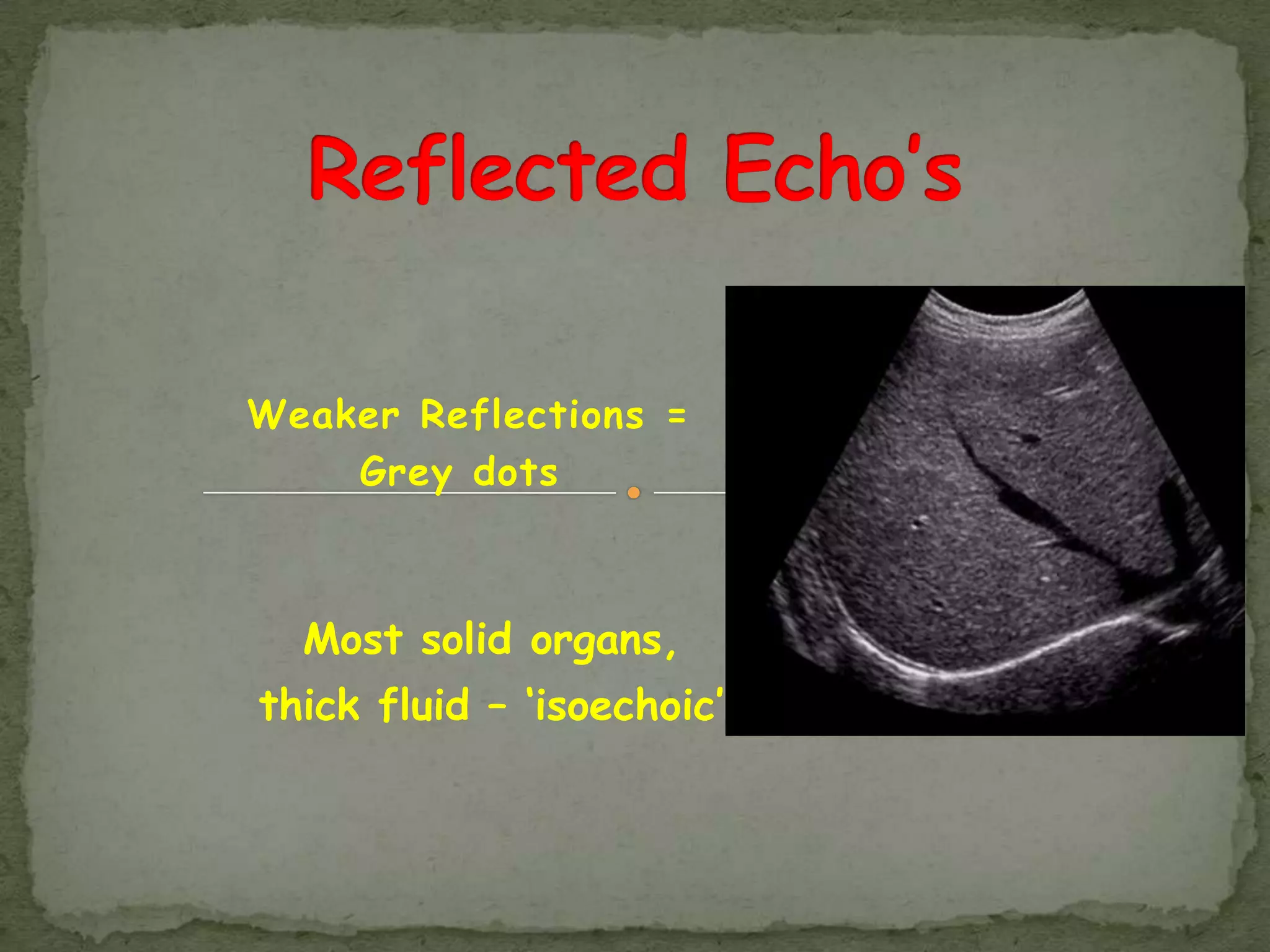
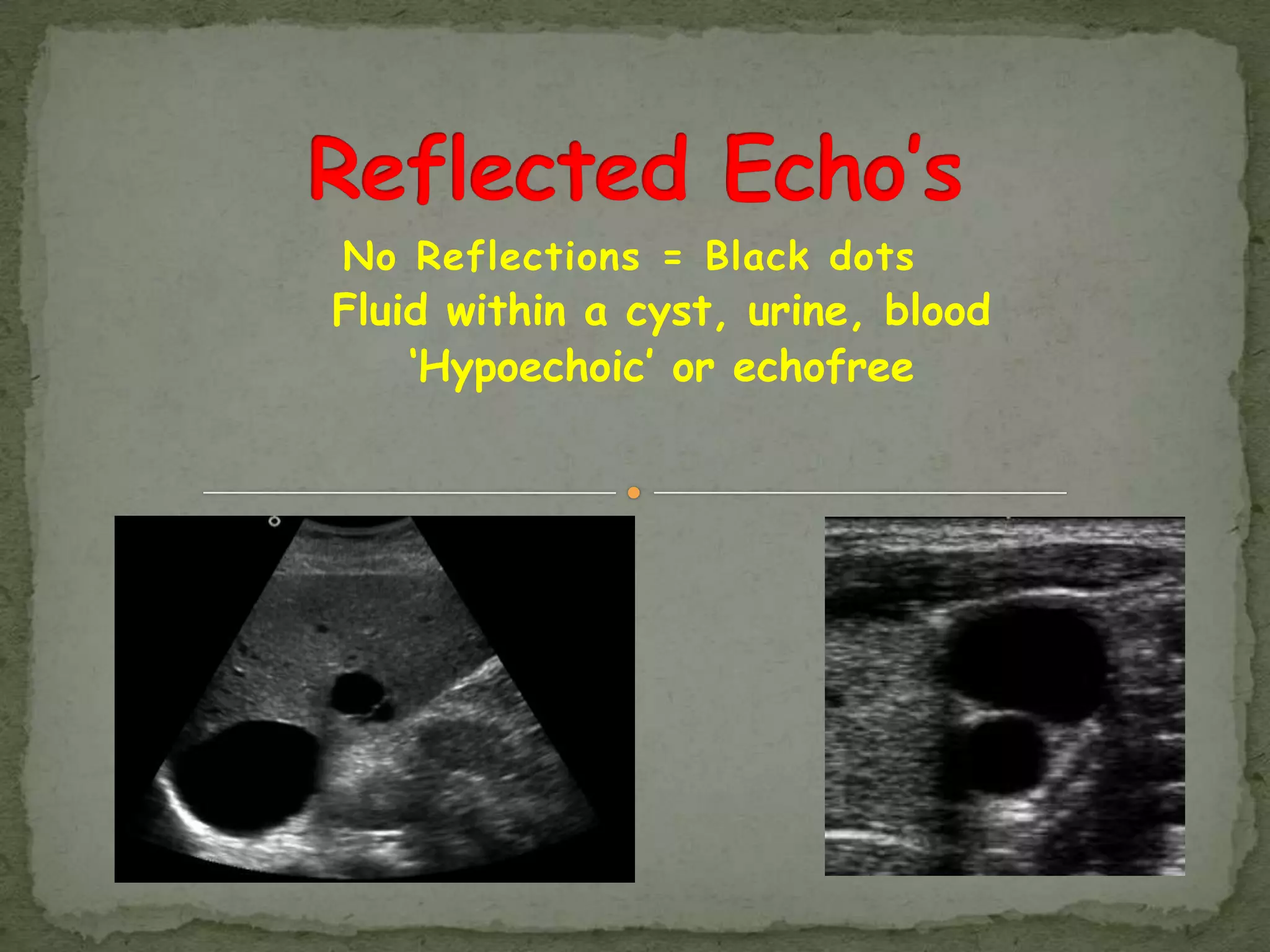
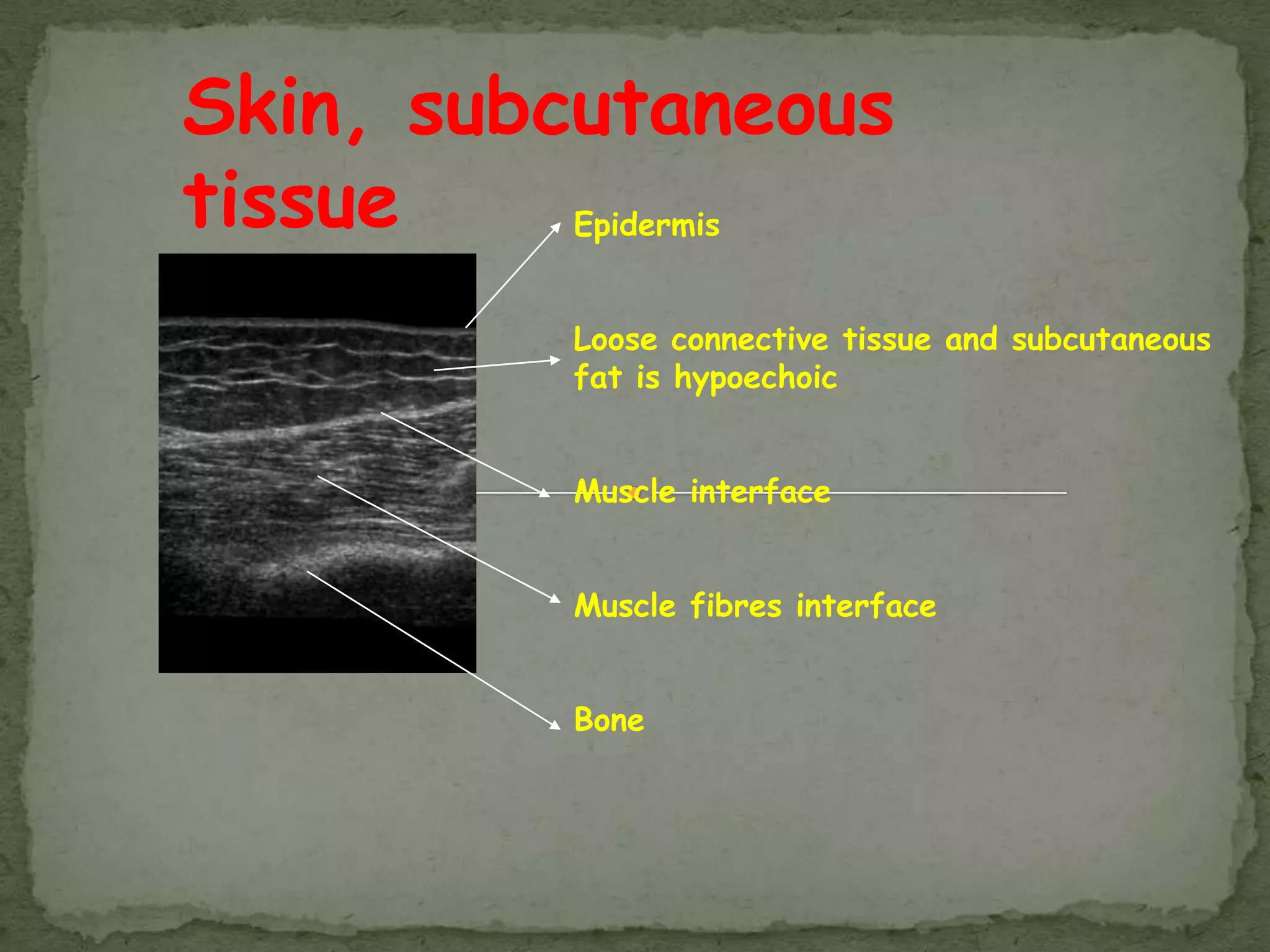
Ultrasound imaging uses high frequency sound waves to create images of internal organs and structures. It provides a non-invasive way to visualize anatomy and diagnose conditions. The document discusses how ultrasound works, including how transducers convert electrical signals to sound waves and receive echo signals. It also covers the factors that affect image quality and resolution. Overall, ultrasound is a valuable medical imaging tool when properly operated by a skilled clinician.