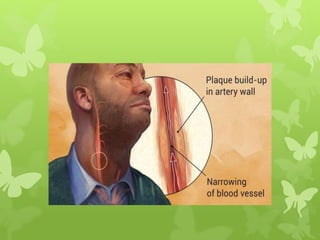
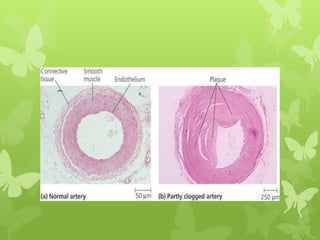
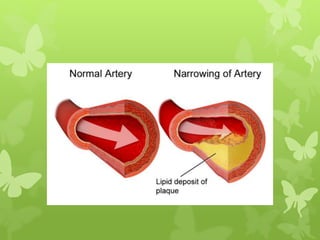
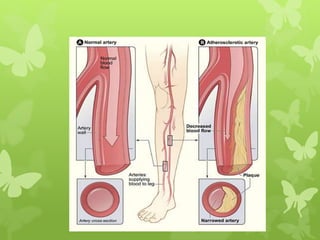
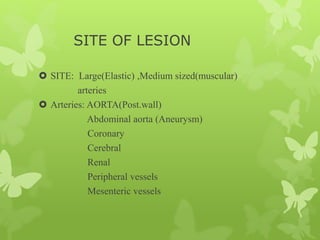
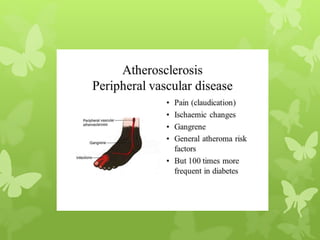
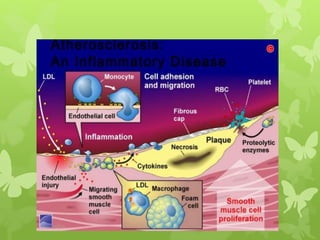
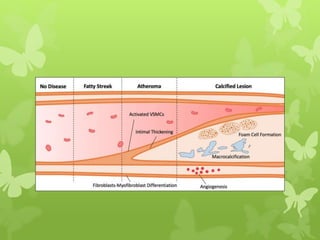
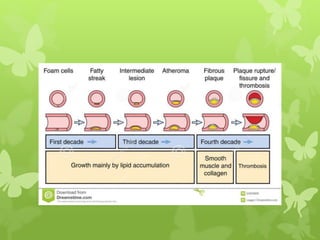
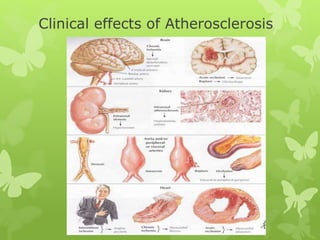
1. Atherosclerosis is a condition where arteries become narrowed and hardened due to plaque buildup in the artery wall.
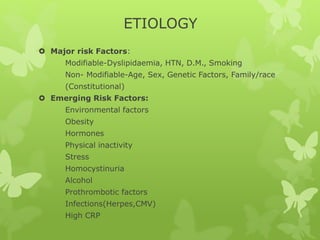
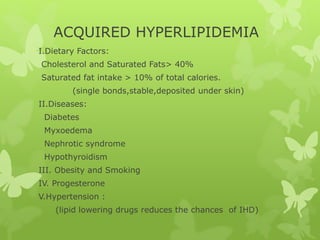
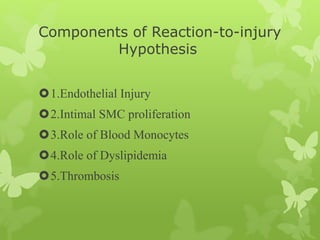
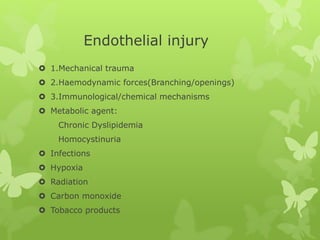
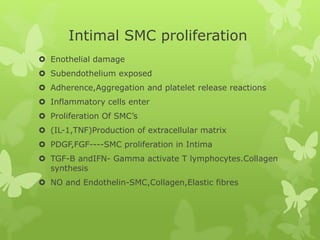
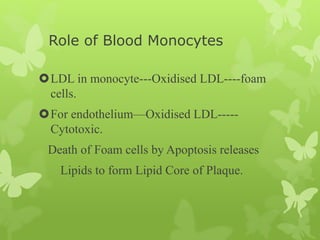
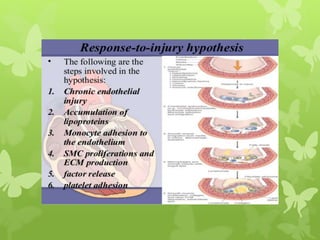
2. Major risk factors include dyslipidemia, hypertension, diabetes, and smoking, which can cause endothelial injury and initiate a response involving smooth muscle cell proliferation and monocyte infiltration.
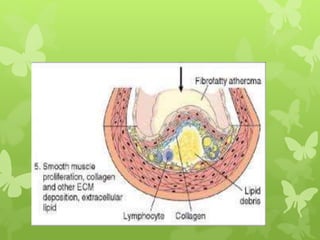
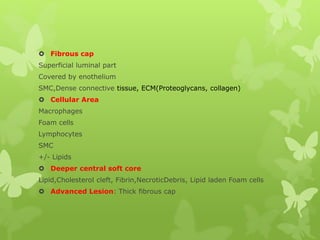
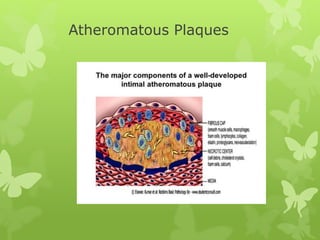
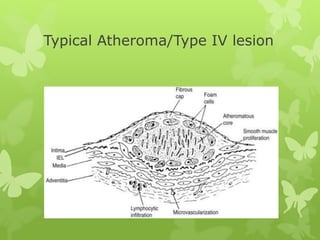
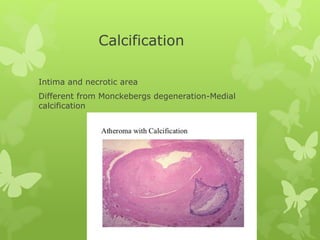
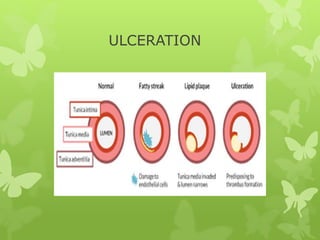
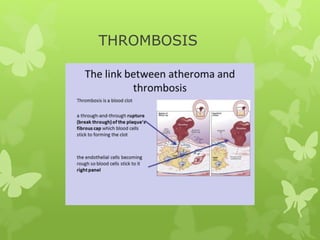
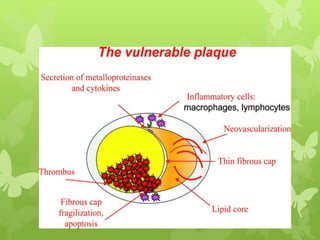
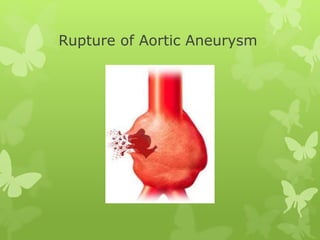
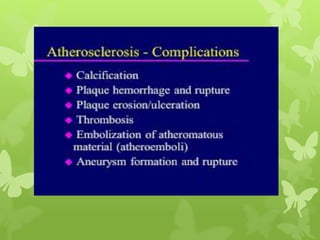
3. Plaque is made up of fat, cholesterol, calcium, and other substances and can progressively worsen over time, potentially leading to complications like heart attacks or strokes if plaques rupture or thrombosis occurs.








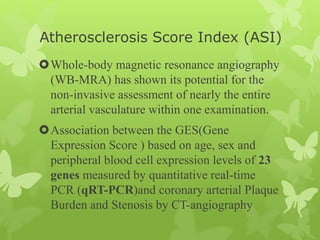
![Atherosclerosis Scoring
The traditional Framingham Risk Score
[QRISK score (http://www.qrisk.org)
Reynolds Risk Score
(http://www.reynoldsriskscore.org)]
The Society for Heart Attack and Eradication (SHAPE)
guidelines ; they advocate assessment of biomarkers in
all intermediate risk patients, a position not yet
endorsed by NLA. ACC/AHA
Guideline for Assessment of Cardiovascular Risk in
Asymptomatic Adults (2010) lists a few diagnostic tests
as Class IIa recommendations.](https://image.slidesharecdn.com/atherosclerosis-180504175041/85/Atherosclerosis-74-320.jpg)
