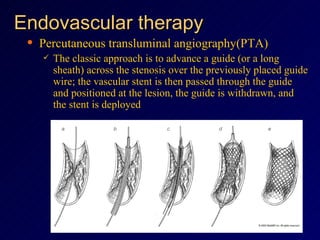
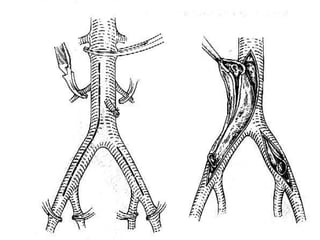
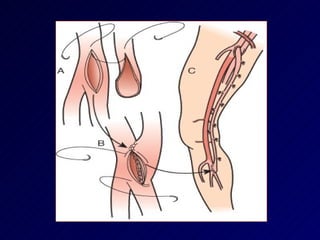
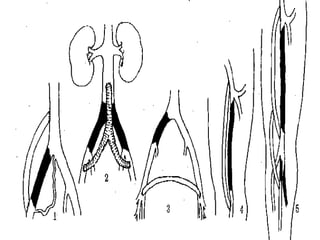
Atherosclerosis is a disease affecting large arteries characterized by plaque buildup in the vessel wall containing lipids, inflammatory cells, and smooth muscle cells. It is caused by multiple risk factors like hyperlipidemia, smoking, hypertension, and diabetes. Symptoms vary depending on location and severity of blockages, and may include leg pain with walking, non-healing wounds, or gangrene. Treatment involves lifestyle changes, medications, and procedures like angioplasty or bypass surgery to improve blood flow.