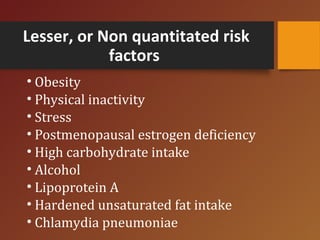
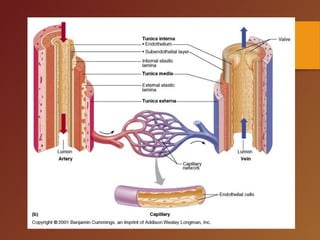
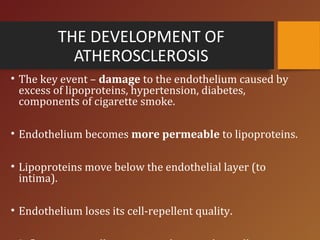
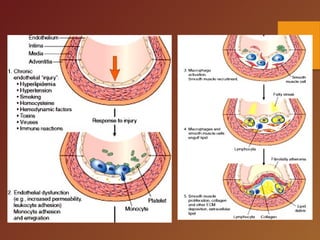
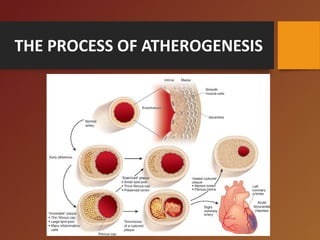
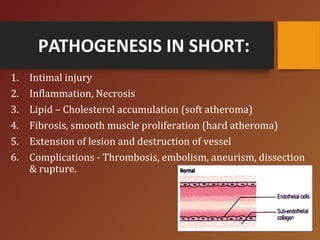
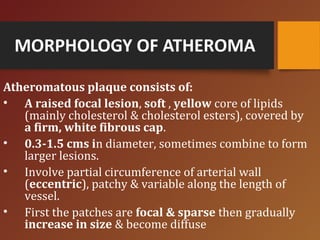
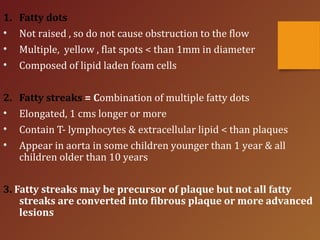
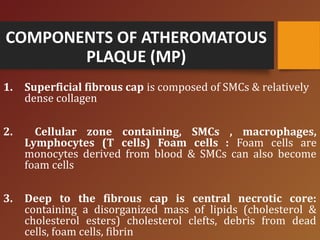
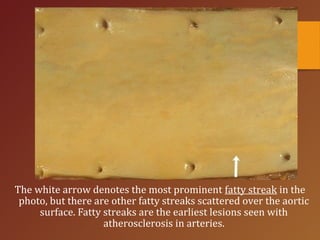
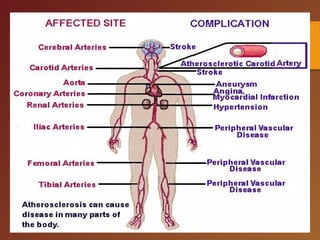
Atherosclerosis is a cardiovascular disease characterized by the narrowing or blockage of arteries due to endothelial dysfunction, lipid deposition, and inflammation. Risk factors include both non-modifiable elements like age and genetics, as well as modifiable factors such as hypertension and smoking. The disease progresses through stages involving intimal injury, inflammation, and lipid accumulation, ultimately leading to serious complications like heart attacks and strokes.