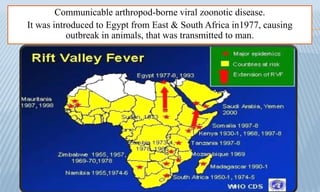
Arthropods transmit many viral, bacterial, and parasitic diseases including yellow fever, dengue fever, rift valley fever, and viral encephalitis. Mosquitoes are the main disease vectors, transmitting pathogens during blood feeding. Common symptoms include fever, bleeding, liver damage, and neurological involvement. Diagnosis involves travel history, serology, and PCR or culture. Prevention focuses on controlling mosquito vectors through environmental management and insecticides, as well as vaccination for diseases like yellow fever.