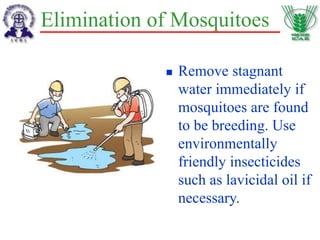
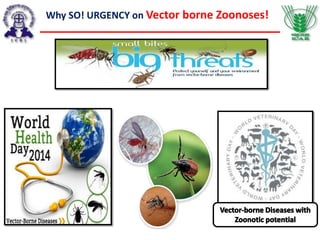
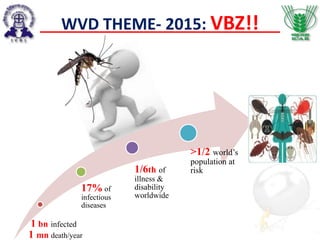
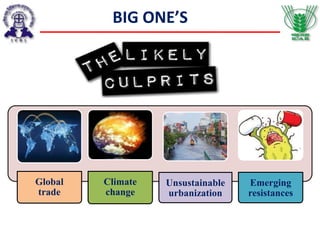
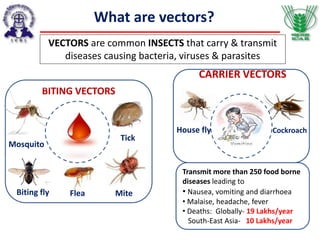
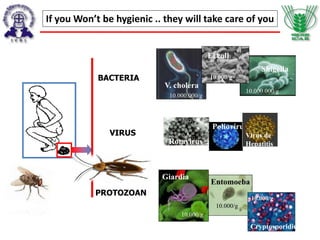
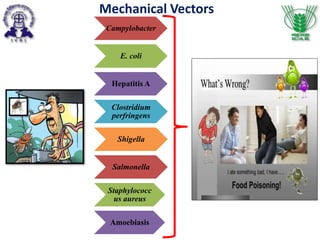
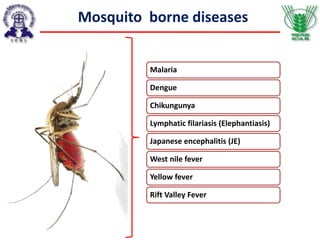
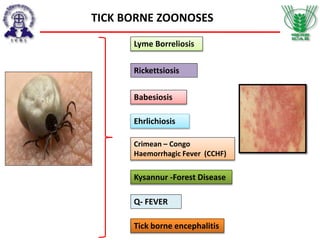
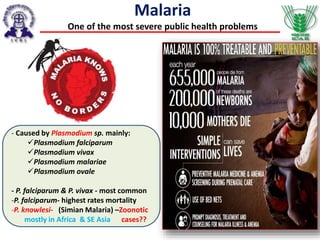
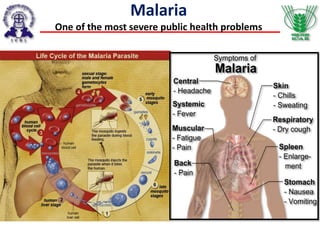
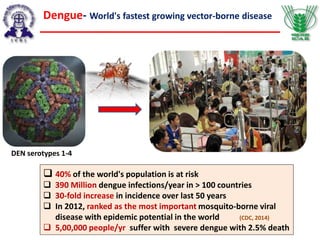
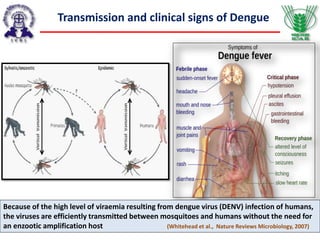
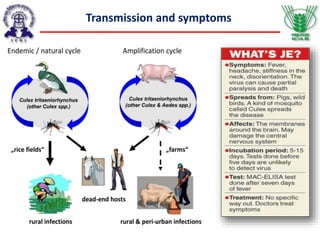
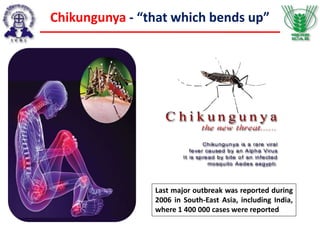
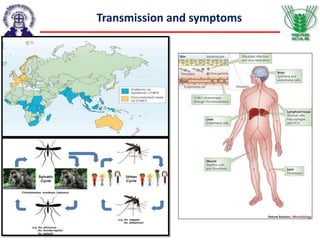
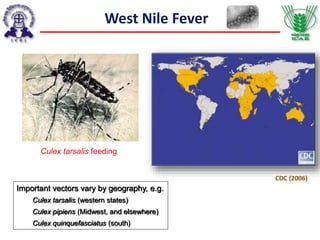
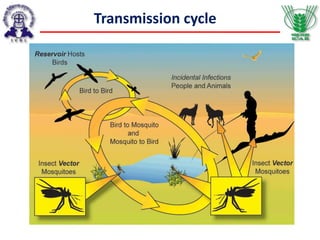
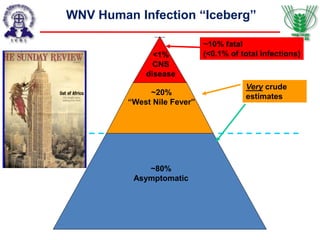
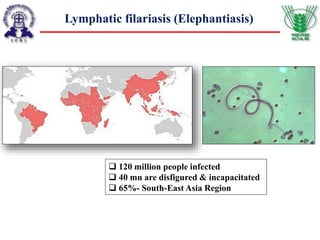
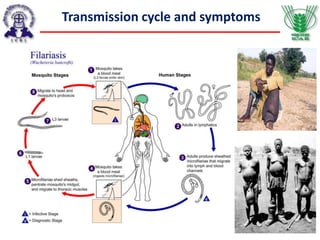
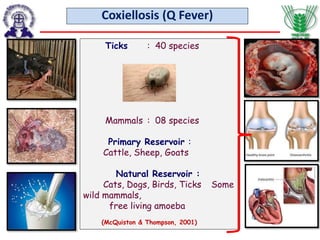
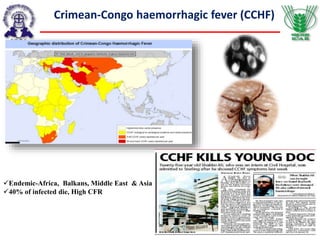
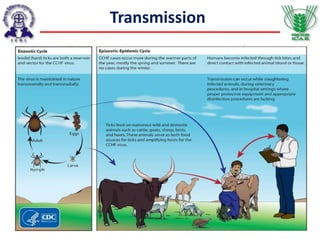
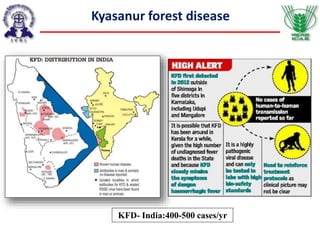
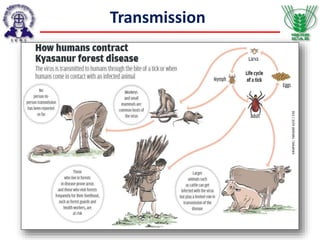
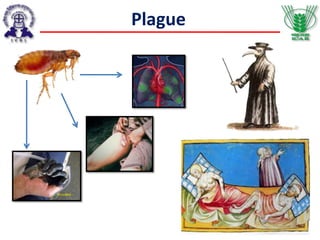
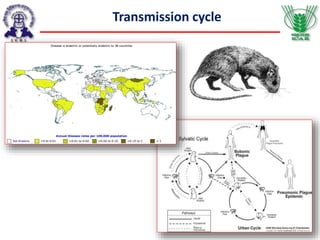
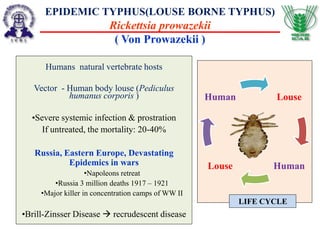
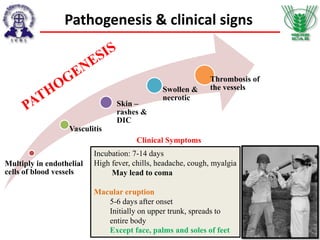
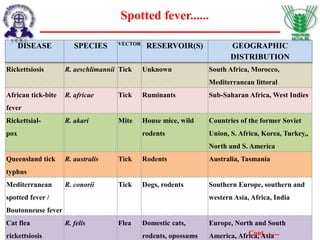
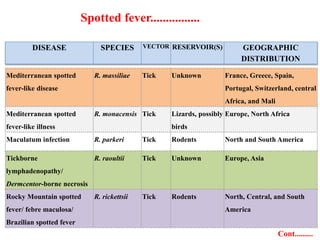
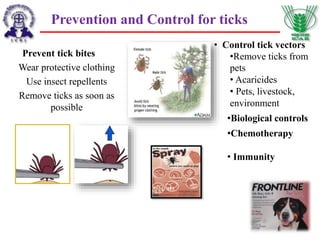
The document discusses World Veterinary Day 2015 and highlights the urgency of addressing vector-borne zoonotic diseases, which pose significant health risks globally. It emphasizes the role of vectors, such as mosquitoes and ticks, in the transmission of various pathogenic organisms that lead to substantial morbidity and mortality. The document also outlines prevention strategies and the importance of maintaining hygiene and environmental cleanliness to mitigate the spread of these diseases.



![DEET containing products, such as
repellents, anti-mosquito patches and
spray are generally most effective to
avoid mosquito bites.
Citronella, Soybean oil and 3-[N-Butyl-
N-acetyl]-aminopropionic acid
containing products also have mosquito
repellent effects.
Portable ultrasonic devices are less
reliable when compared with DEET.
Personal Protection
Choosing the insect repellents](https://image.slidesharecdn.com/vbzs2015-04-24wvdeditedbysvs71final-150429094905-conversion-gate01/85/Vector-Borne-Zoonoses-46-320.jpg)