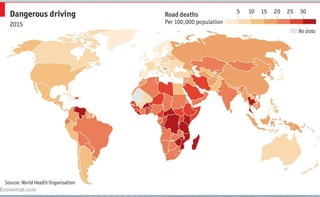
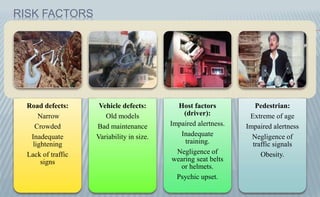
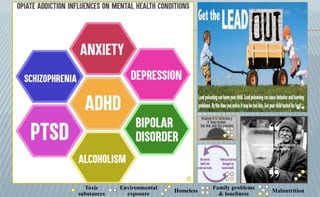
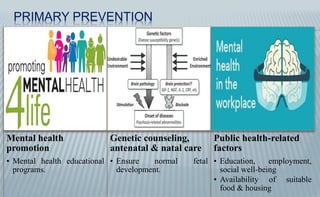
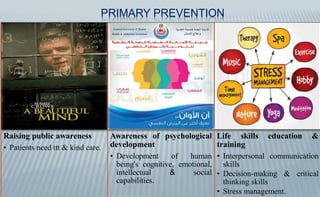
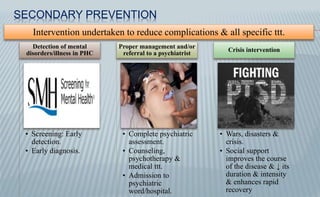
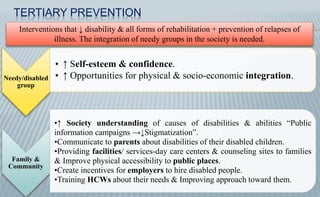
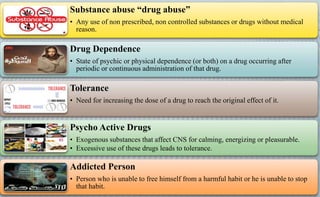
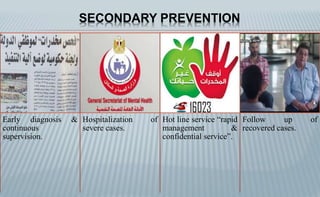
This document discusses epidemiology of non-communicable diseases, specifically accidents, road traffic accidents, home accidents, occupational accidents, and substance abuse. It notes that accidents are unexpected events that cause injury, death or property damage. Road traffic accidents are a leading cause of death in developing countries. Home accidents commonly involve burns, falls, electric shocks, wounds and poisoning. Occupational accidents are work-related injuries and the document outlines various risk factors. Substance abuse is also discussed, including types of drugs, risk factors, impacts, and prevention strategies. Prevention is addressed at primary, secondary and tertiary levels.