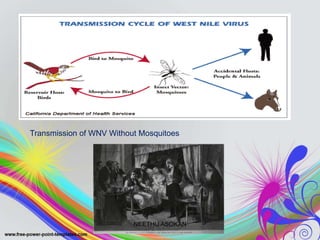
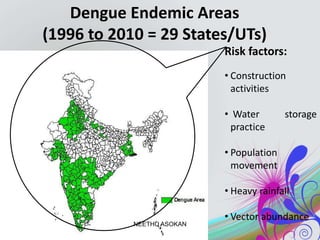
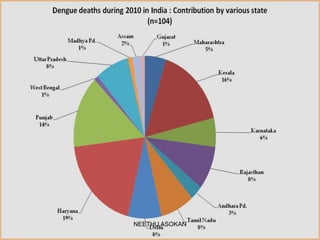
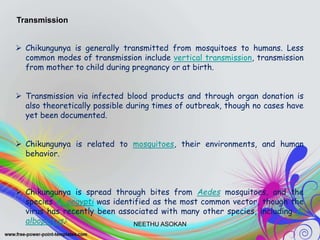
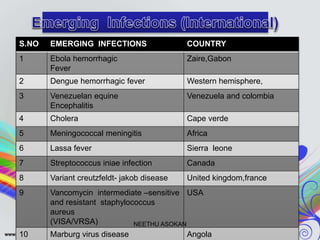
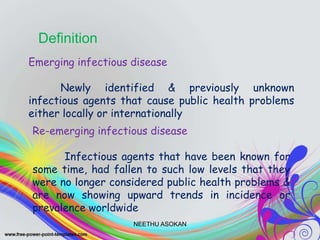
The document discusses various emerging and re-emerging infectious diseases, their causes, and examples. It defines emerging infectious diseases as newly identified infectious agents and re-emerging diseases as known agents that were previously under control but are increasing. The document then examines biological, environmental physical and social factors that influence disease emergence. It provides examples of transmission routes and recently emerging diseases such as Ebola virus, influenza, SARS, West Nile virus, monkeypox, and dengue. Tables list Ebola outbreak case counts by country and emerging infections and locations in India from 1990-2006.














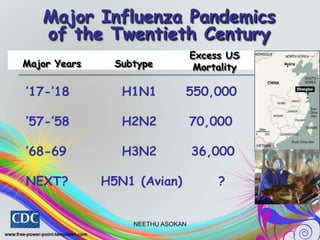
![ H1N1, which caused Spanish Flu in 1918, and Swine Flu in
2009
H2N2, which caused Asian Flu in 1957
H3N2, which caused Hong Kong Flu in 1968
H5N1, which caused Bird Flu in 2004
H7N7, which has unusual zoonotic potential[35]
H1N2, endemic in humans, pigs and birds
H9N2
H7N2
H7N3
H10N7
H7N9
Influenzavirus A
Influenzavirus B
Influenzavirus A
Influenzavirus C
NEETHU ASOKAN](https://image.slidesharecdn.com/presentation2emergingdiseases-191204123556/85/Emerging-diseases-16-320.jpg)