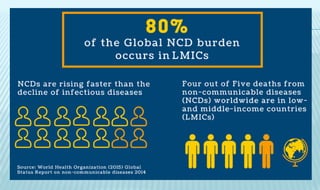
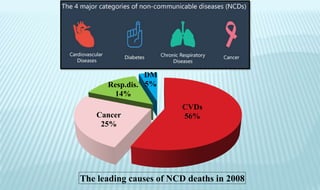
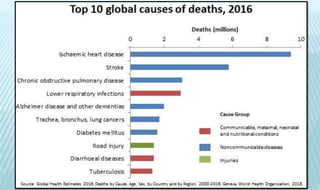
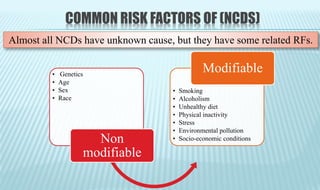
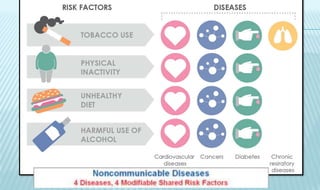
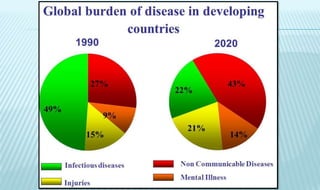
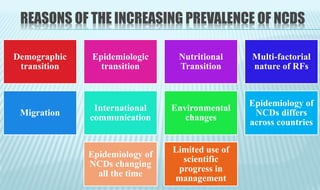
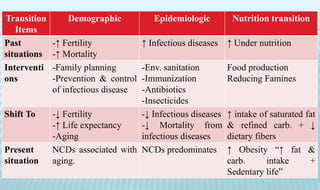
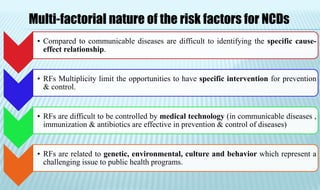
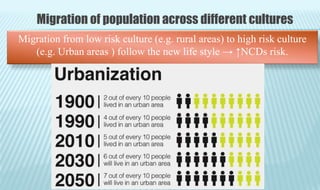
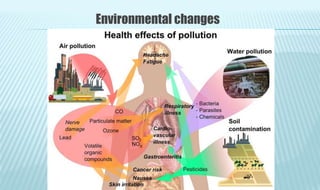
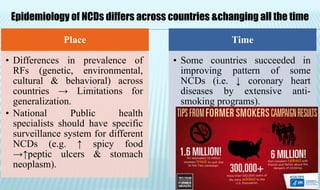
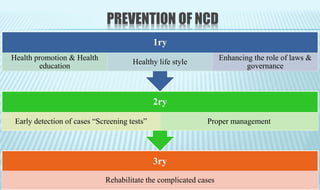
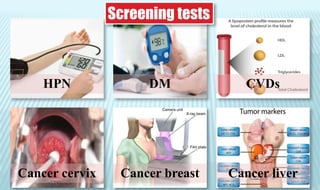
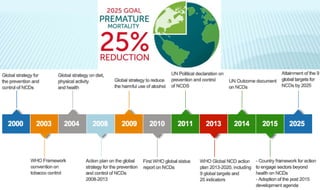
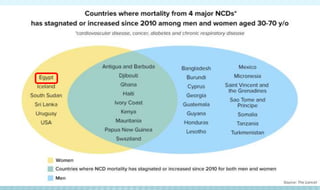
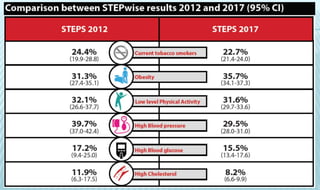
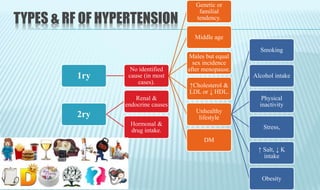
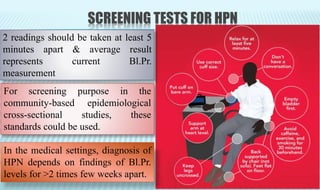
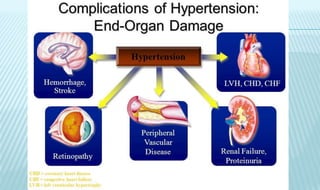
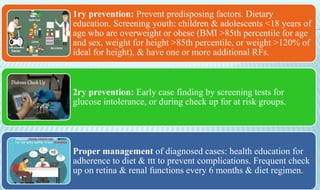
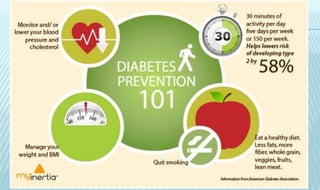
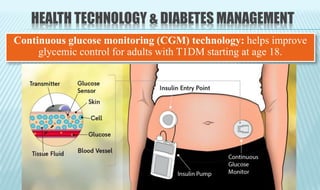
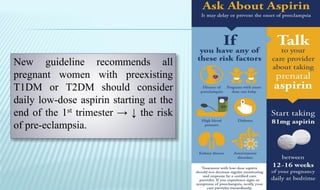
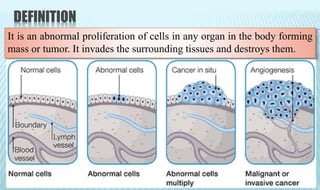
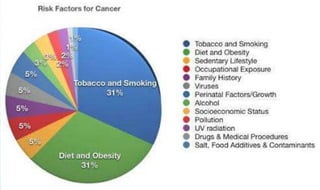
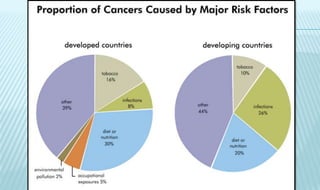
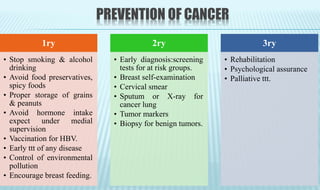
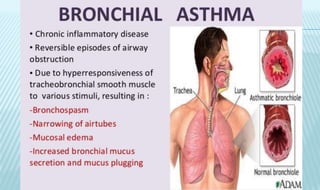
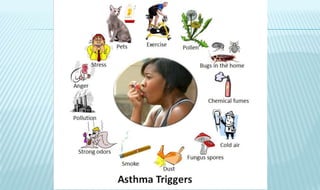
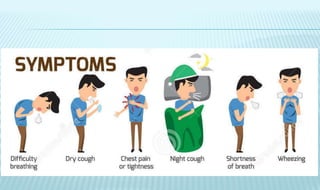
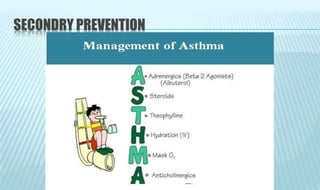
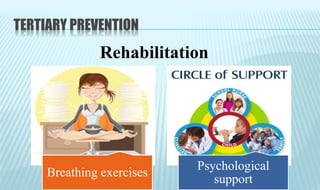
Non-communicable diseases (NCDs) such as cardiovascular diseases, cancer, respiratory diseases, and diabetes account for the majority of deaths globally. The document discusses NCDs in depth, including their definition, common risk factors, reasons for their increasing prevalence, and strategies for prevention and management. The key strategies discussed are health promotion through lifestyle changes, early detection via screening programs, and proper long-term medical management of diagnosed cases.