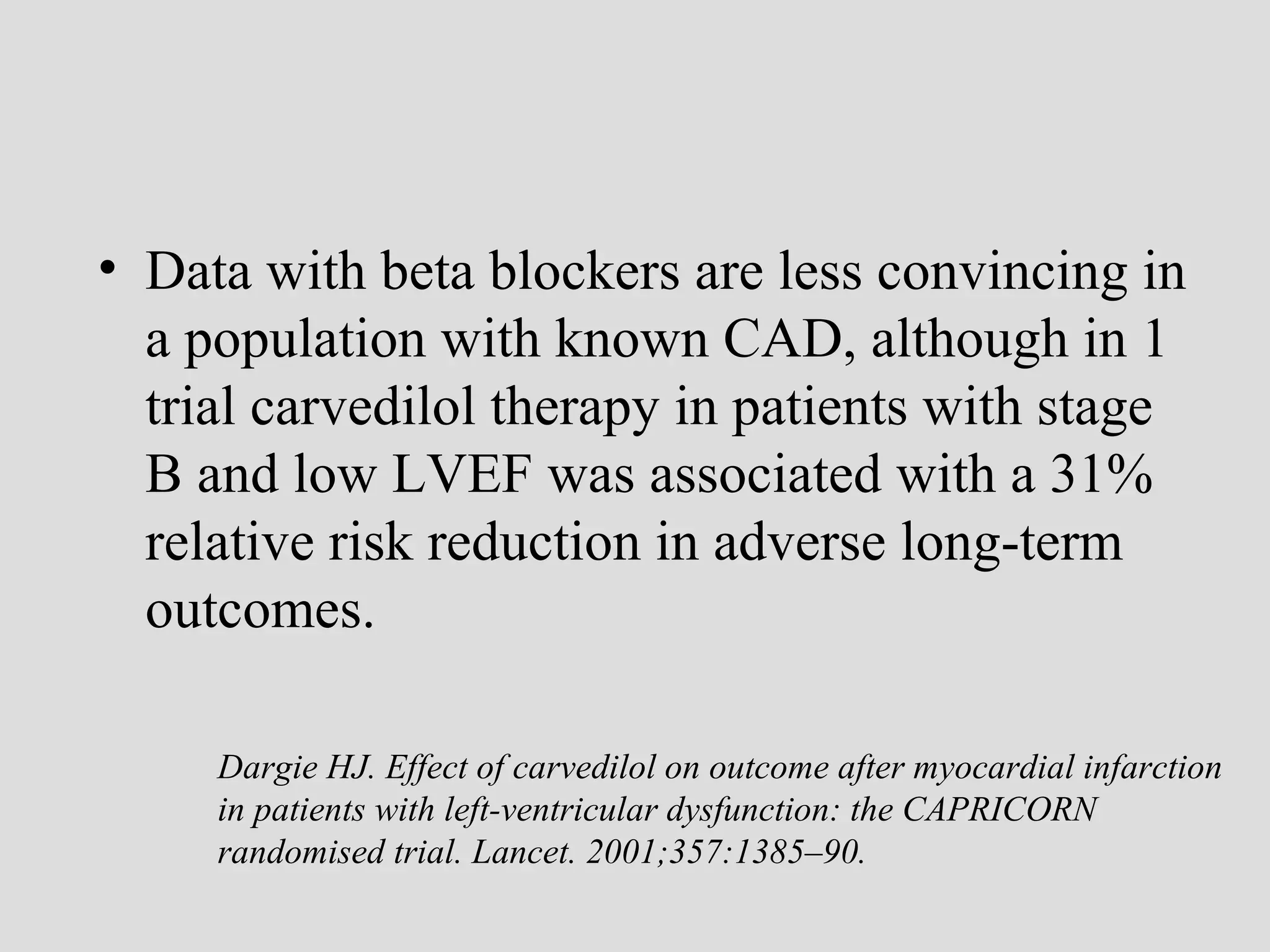
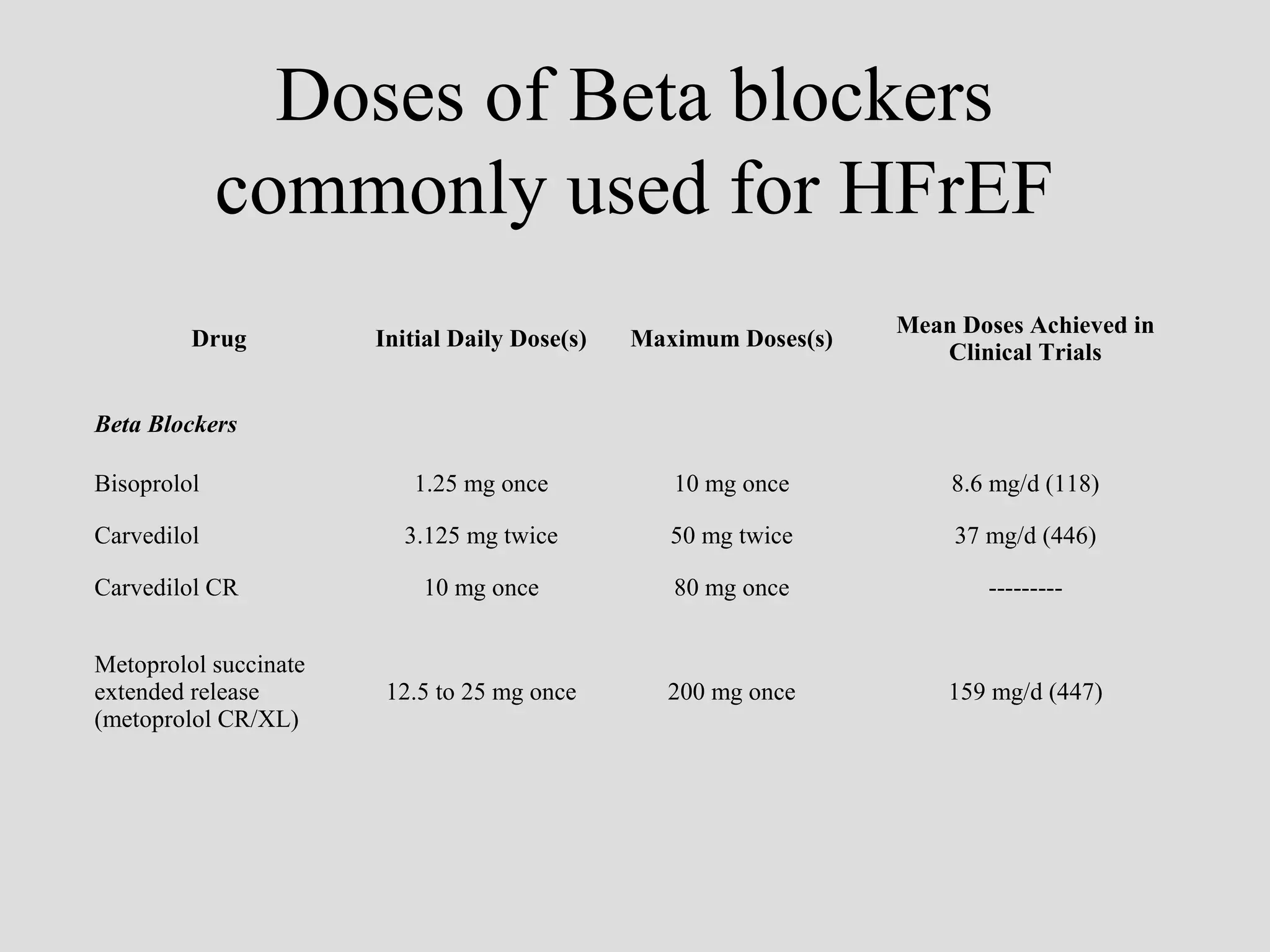
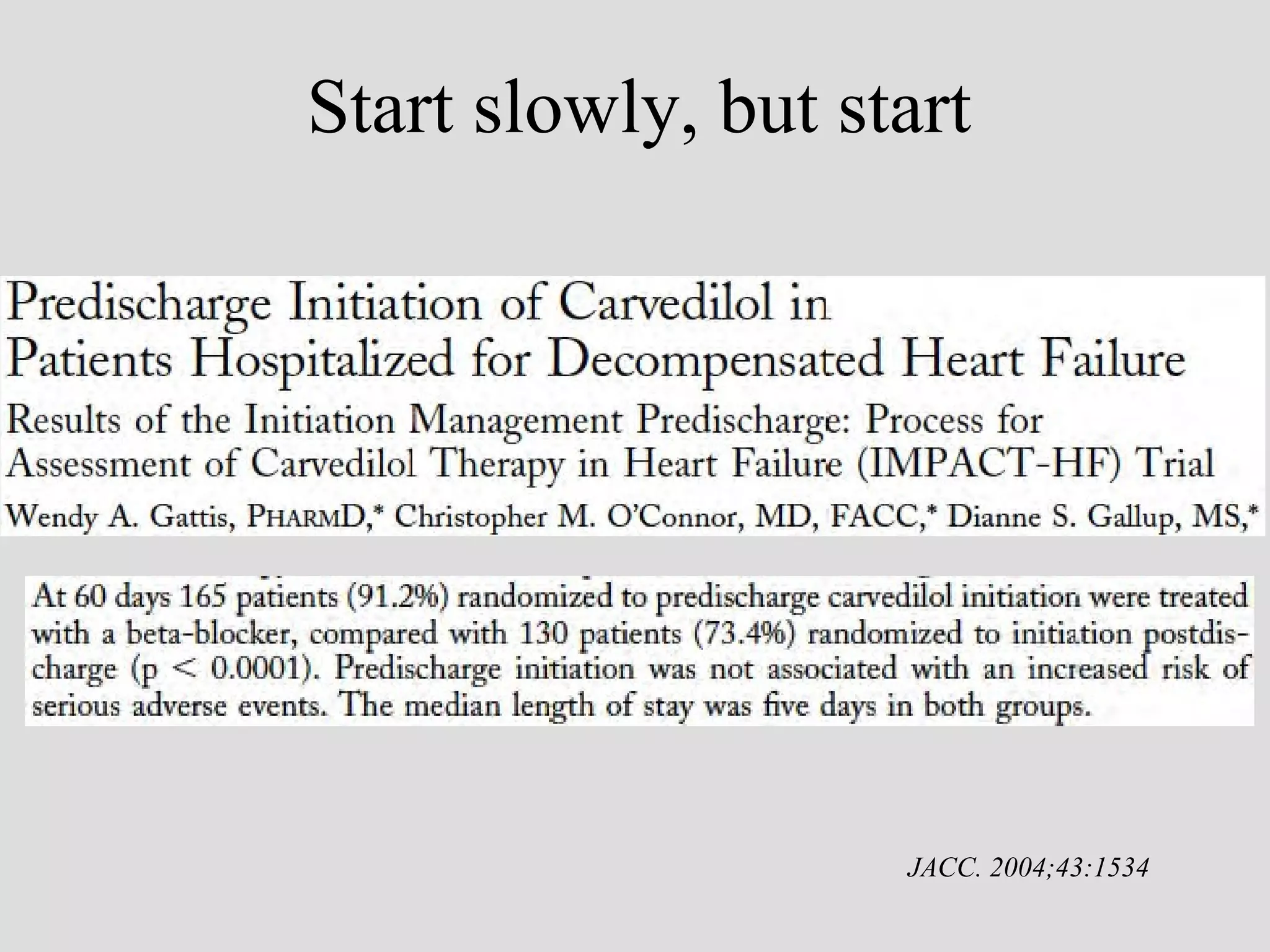
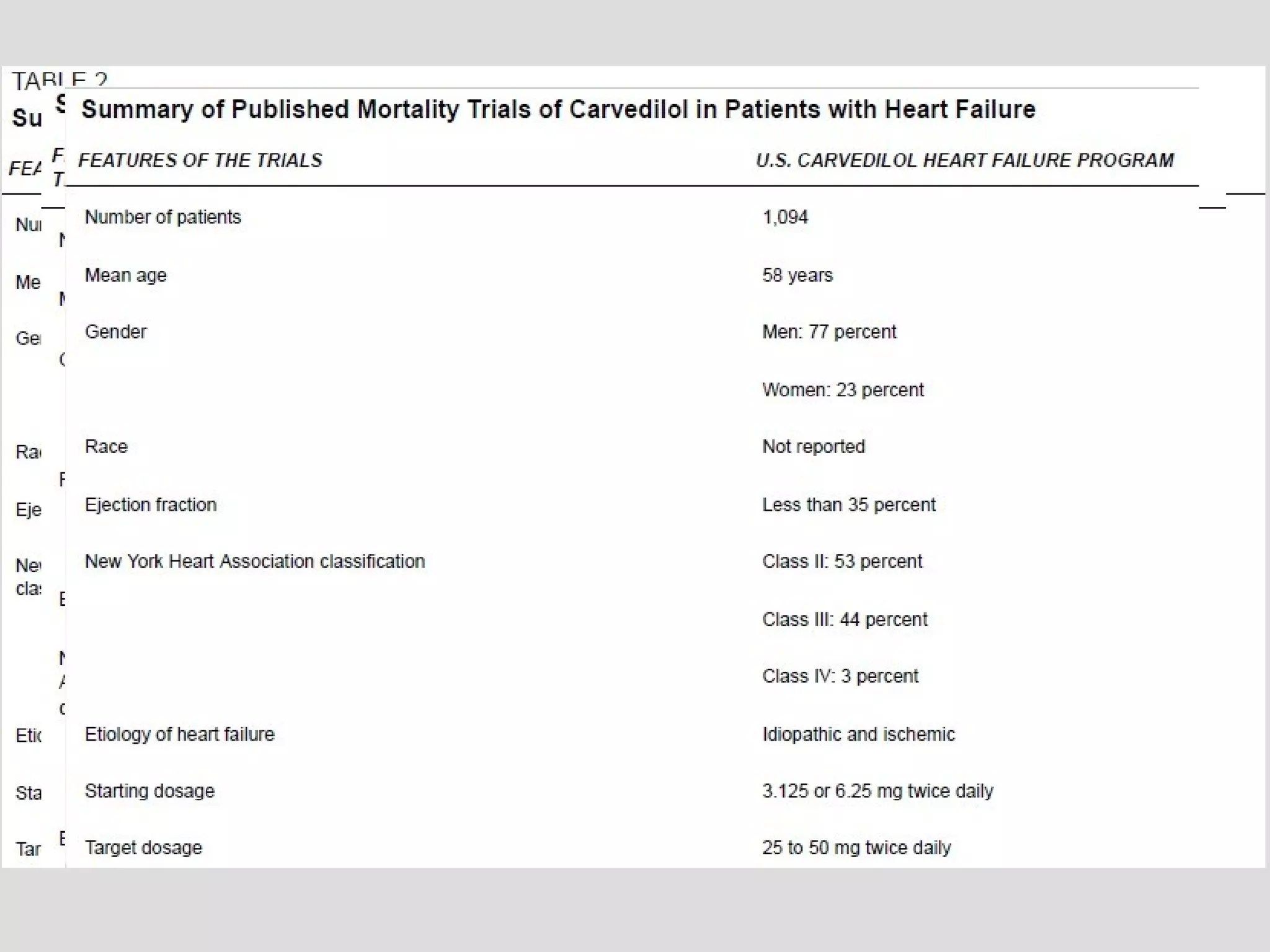
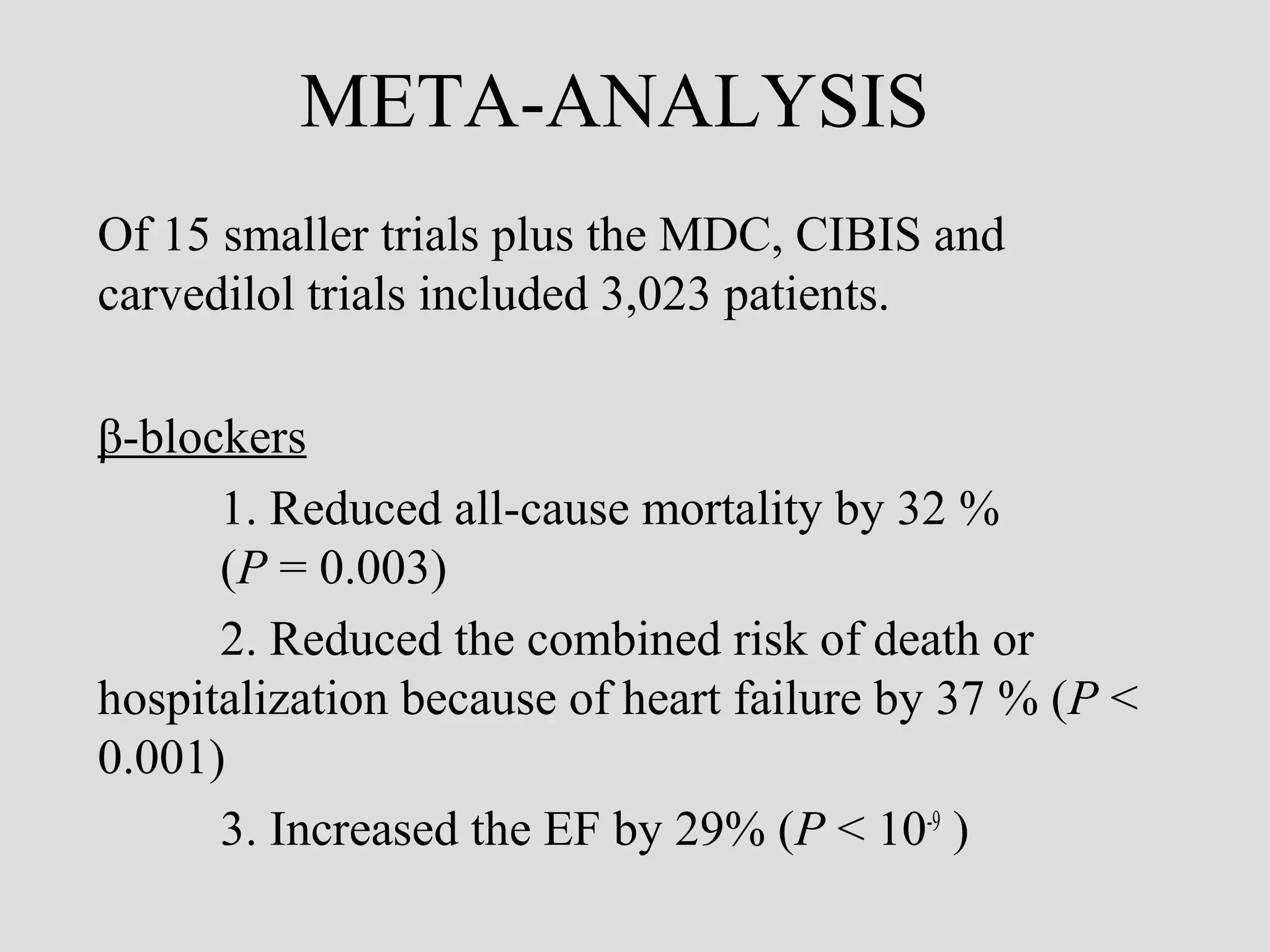
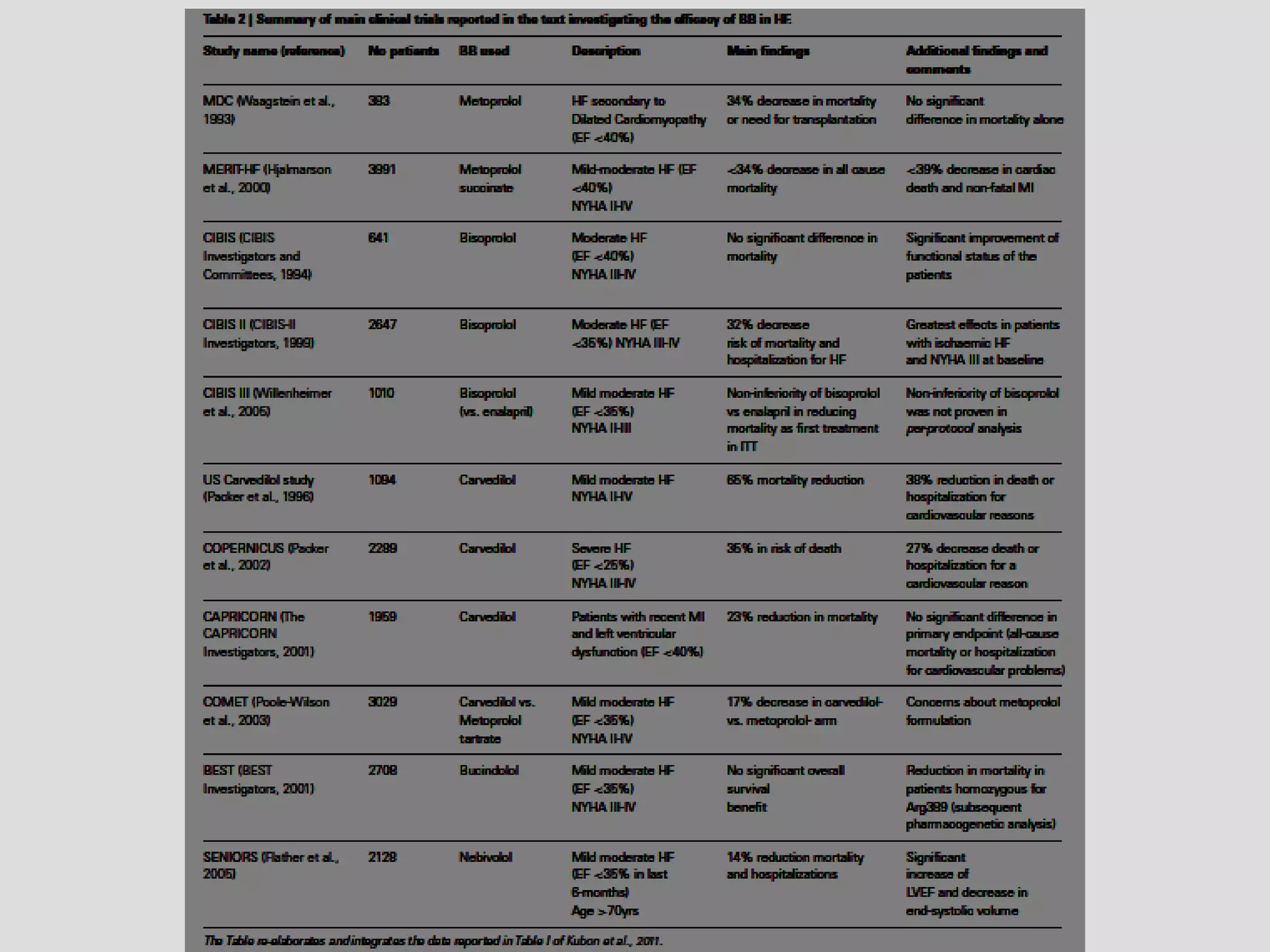
Beta blockers are the most effective therapy for heart failure according to clinical trials. Long term use of beta blockers such as bisoprolol, carvedilol, and sustained release metoprolol succinate can reduce mortality, heart failure hospitalizations, and improve ejection fraction and symptoms of heart failure. While initiation requires slow uptitration, discontinuation of beta blockers during heart failure hospitalization is generally not necessary and may worsen outcomes.