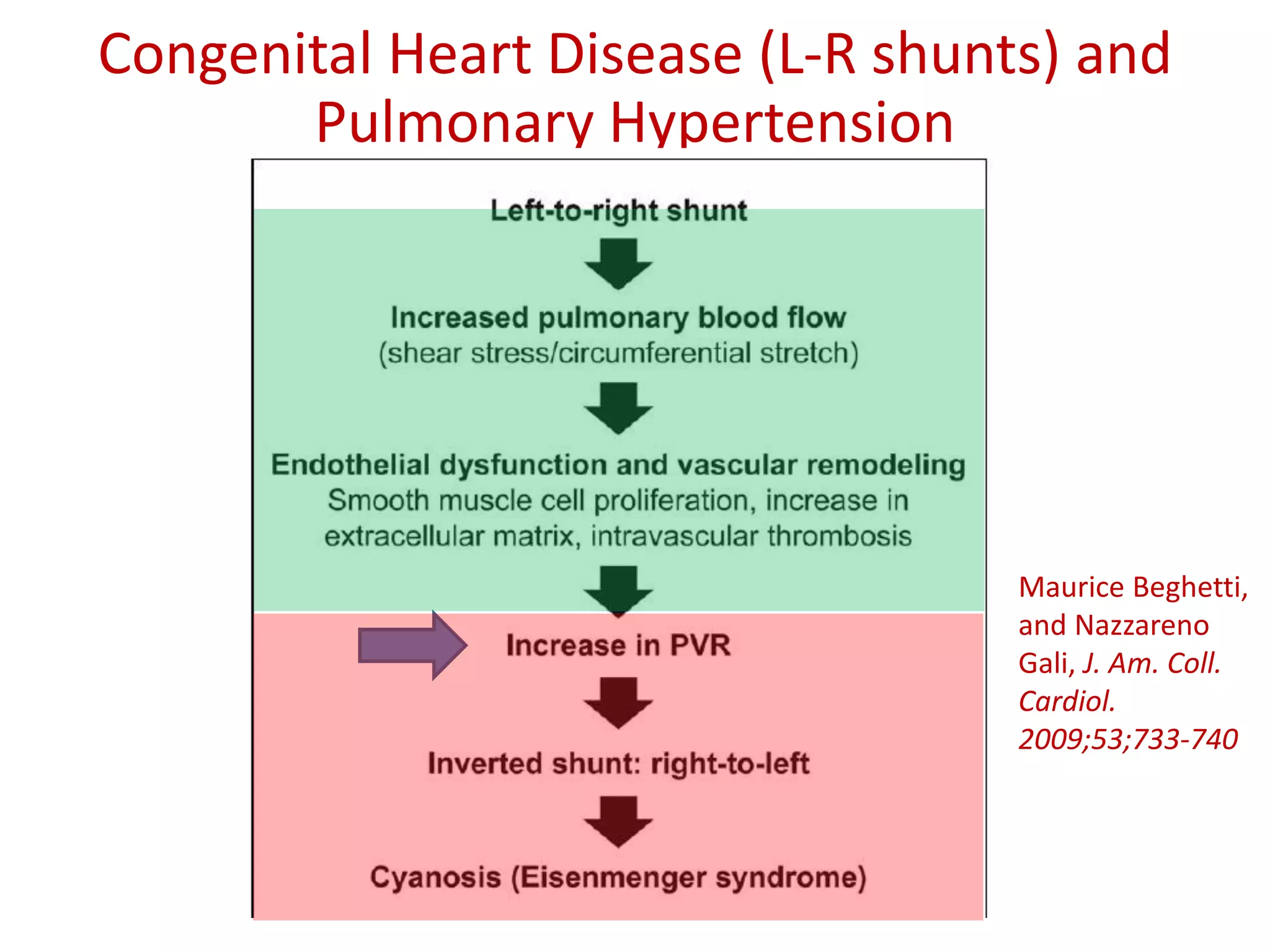
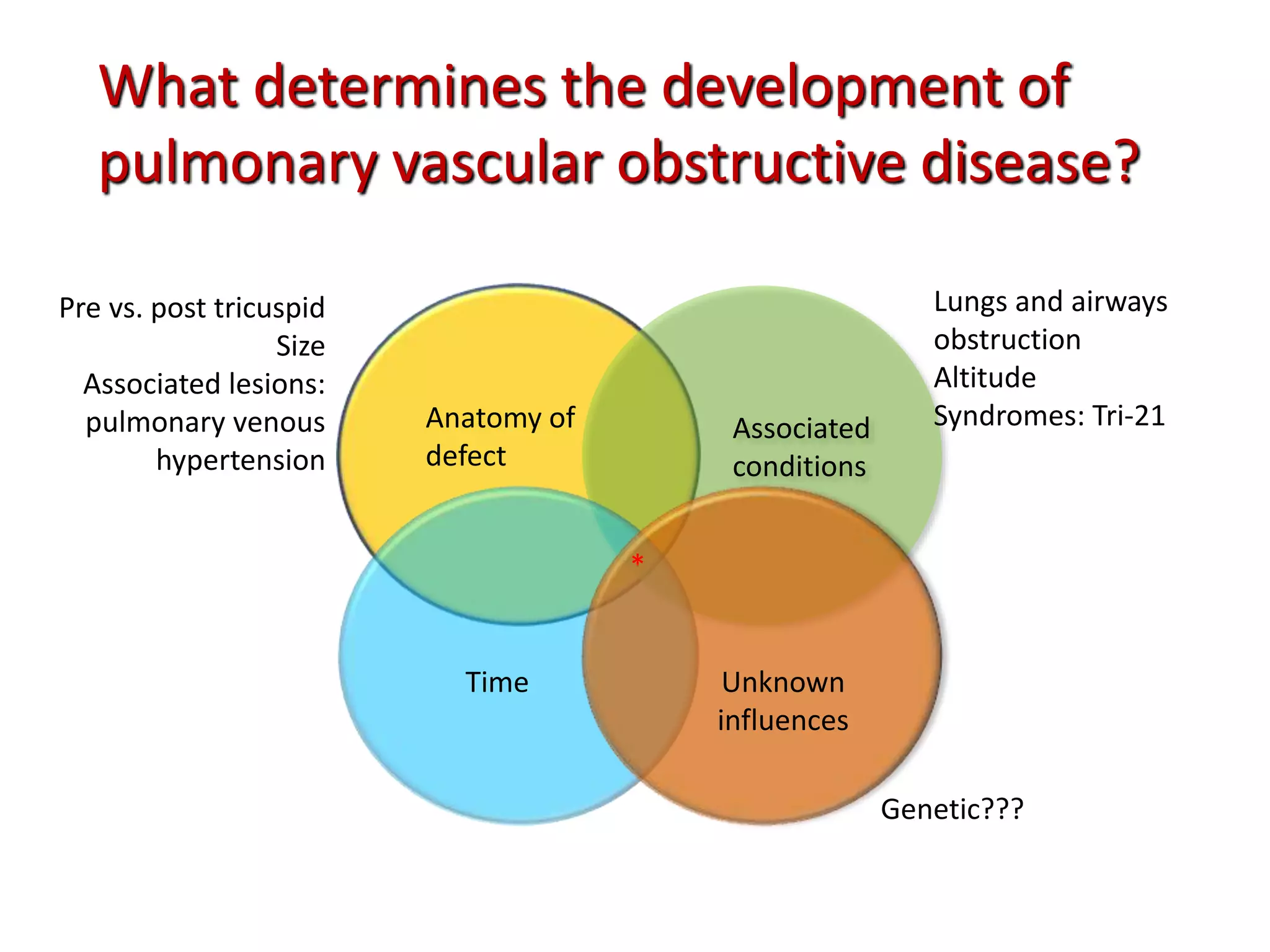
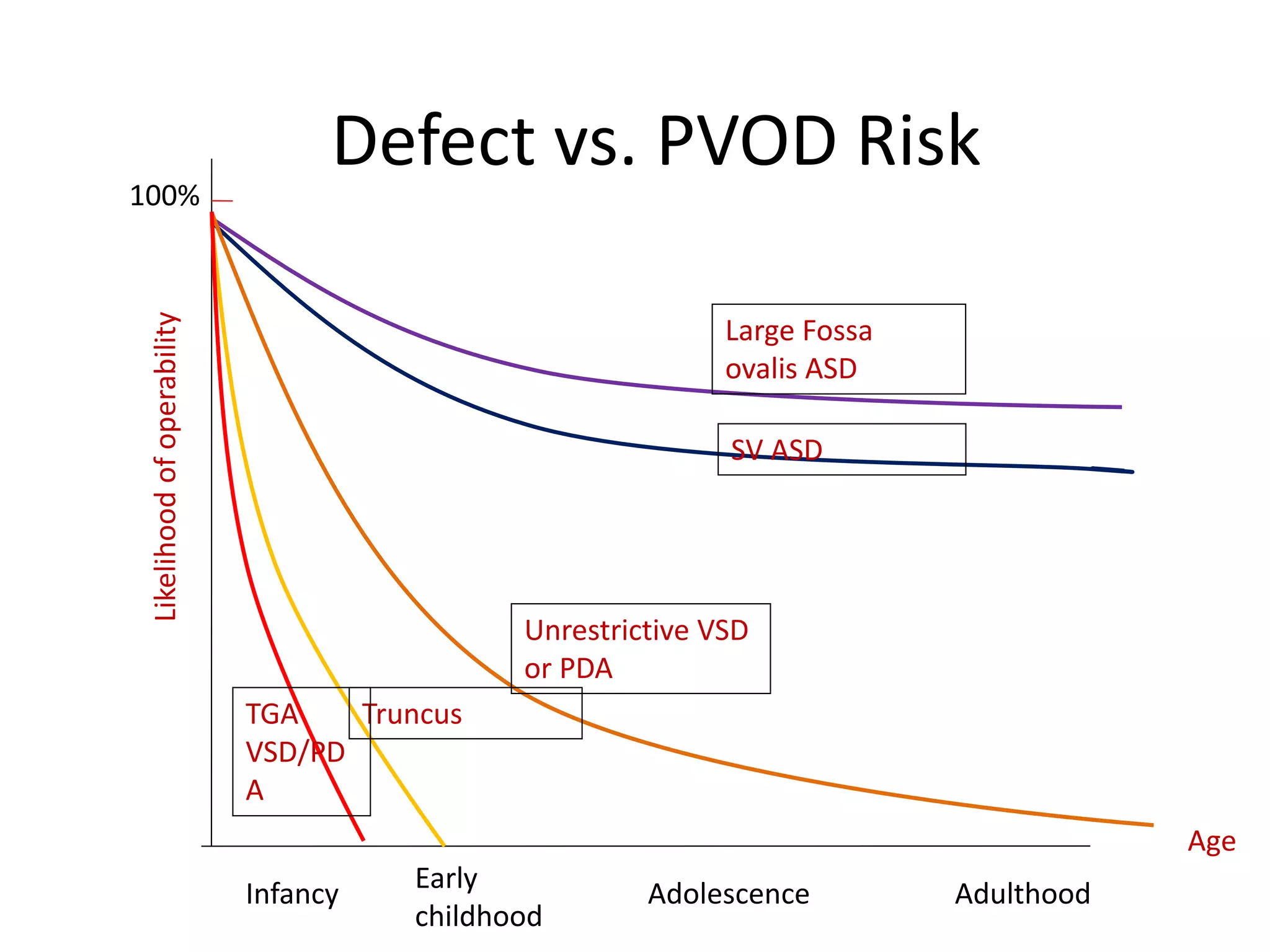
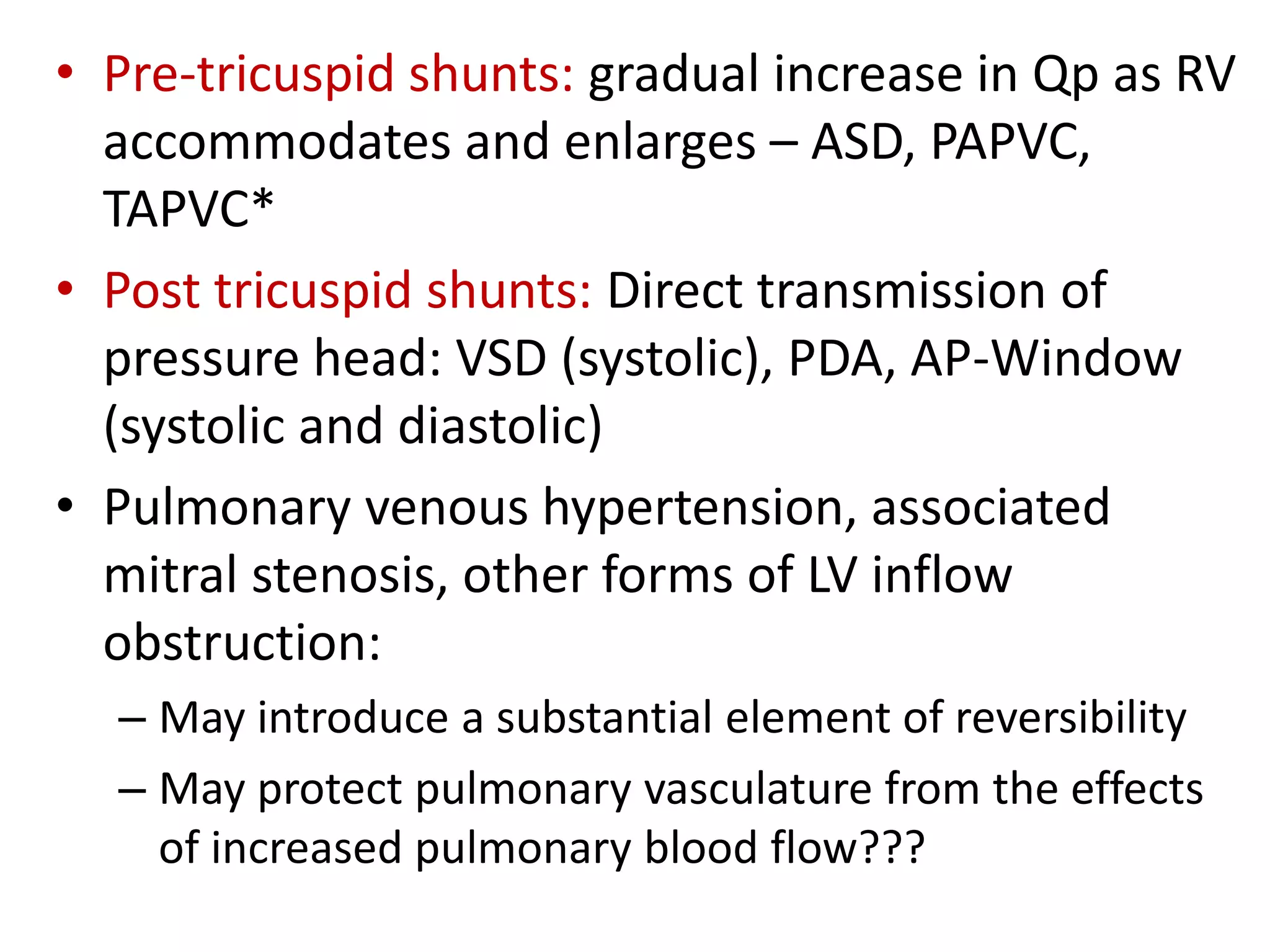
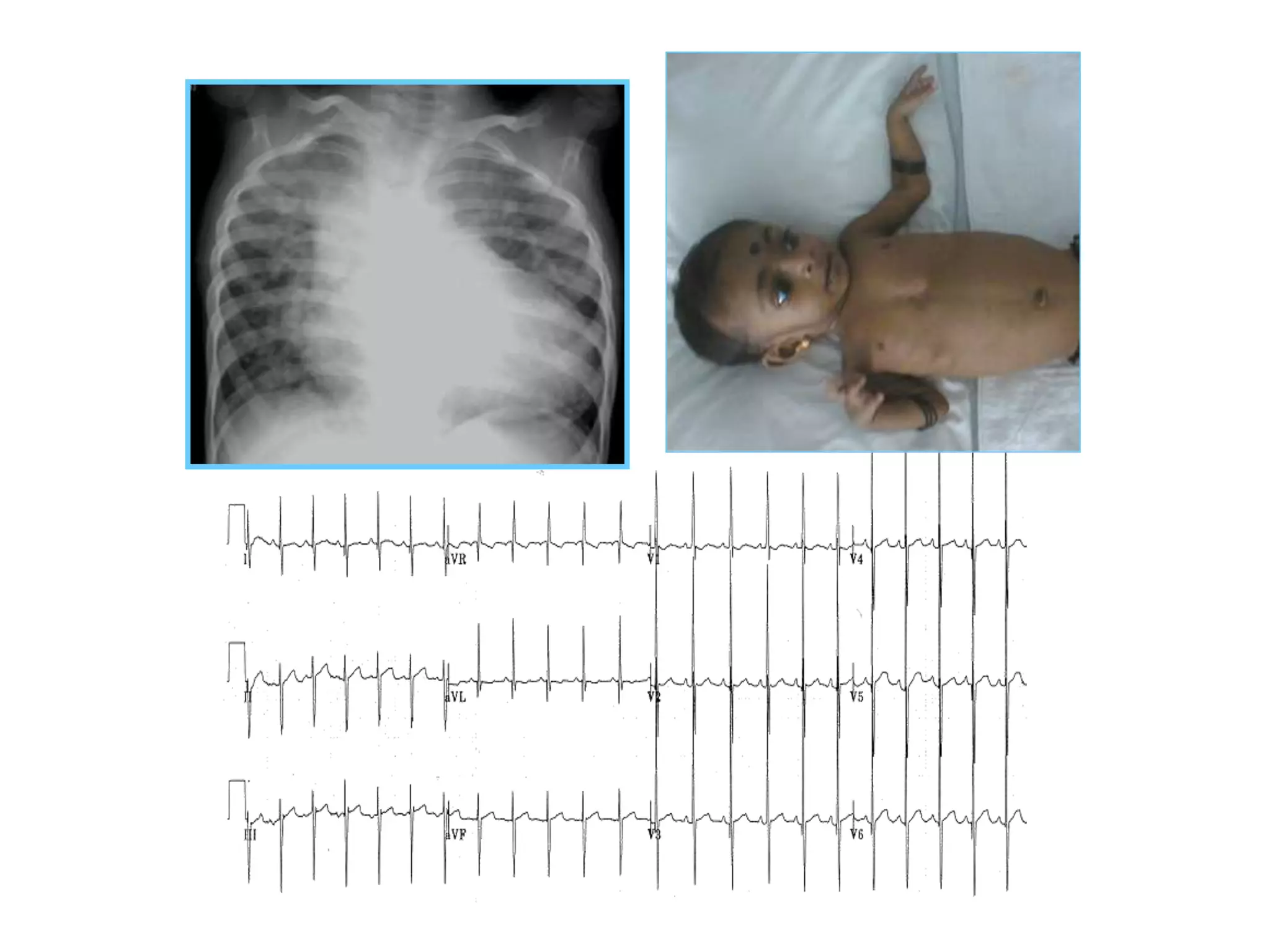
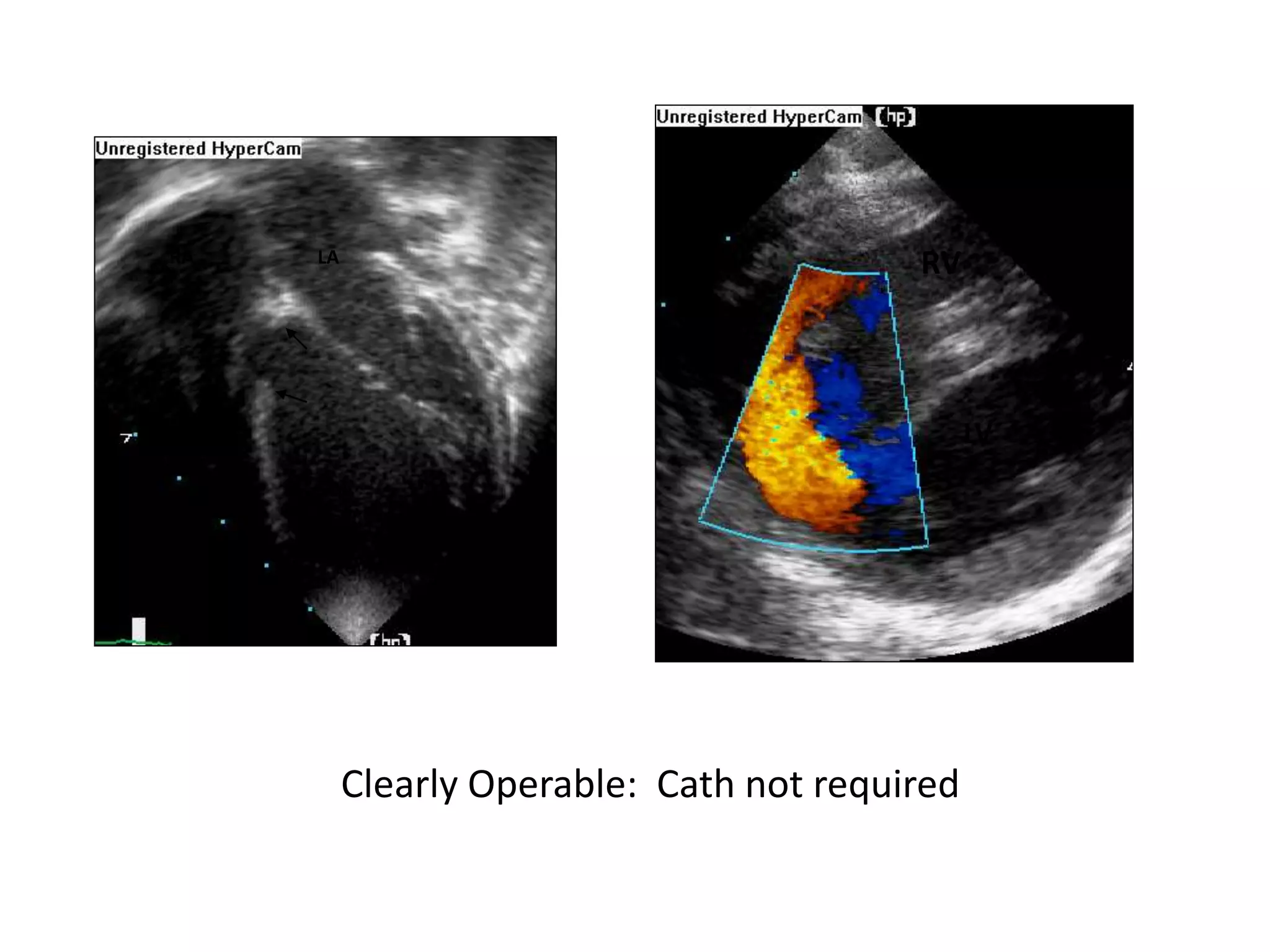
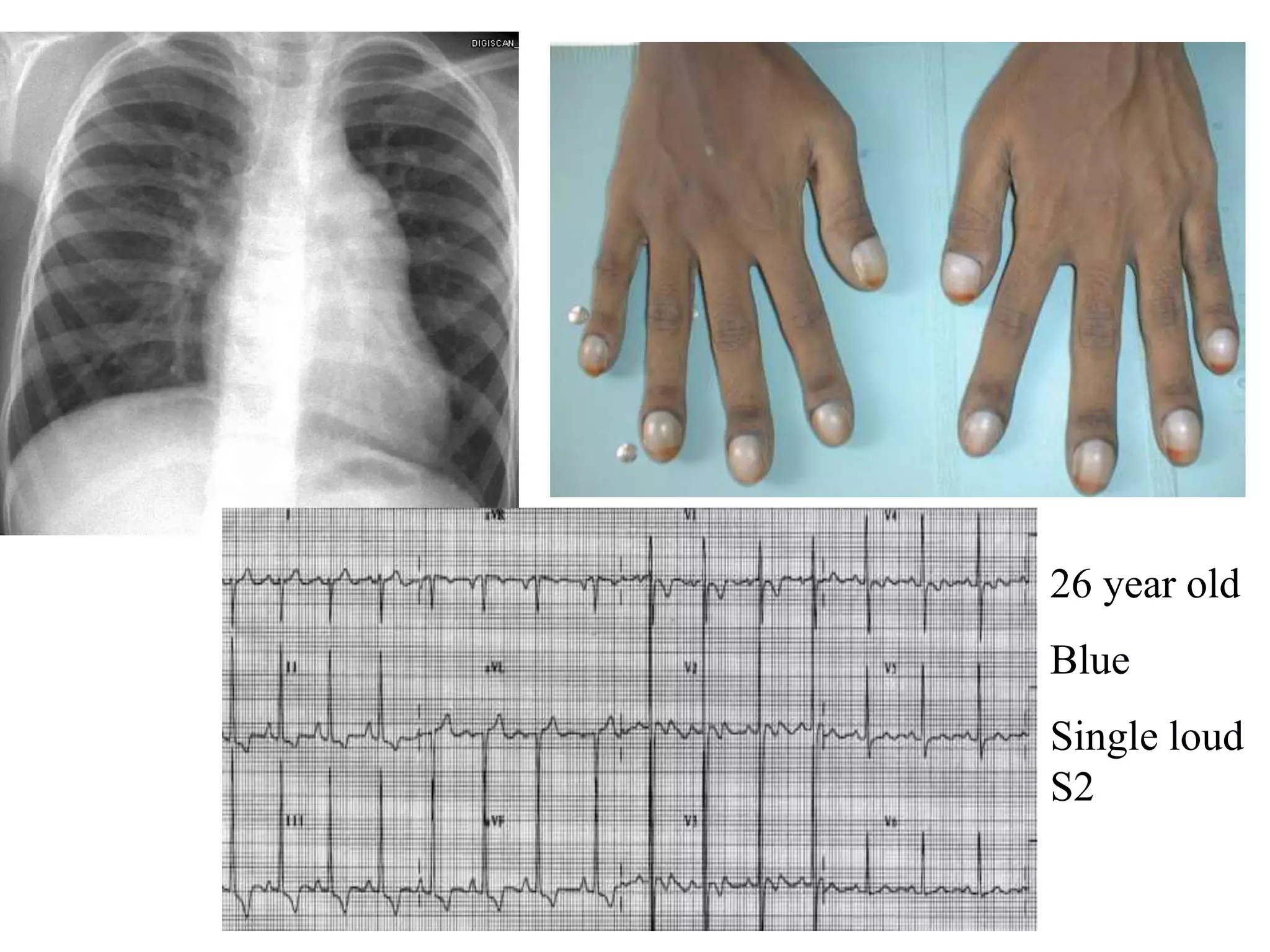
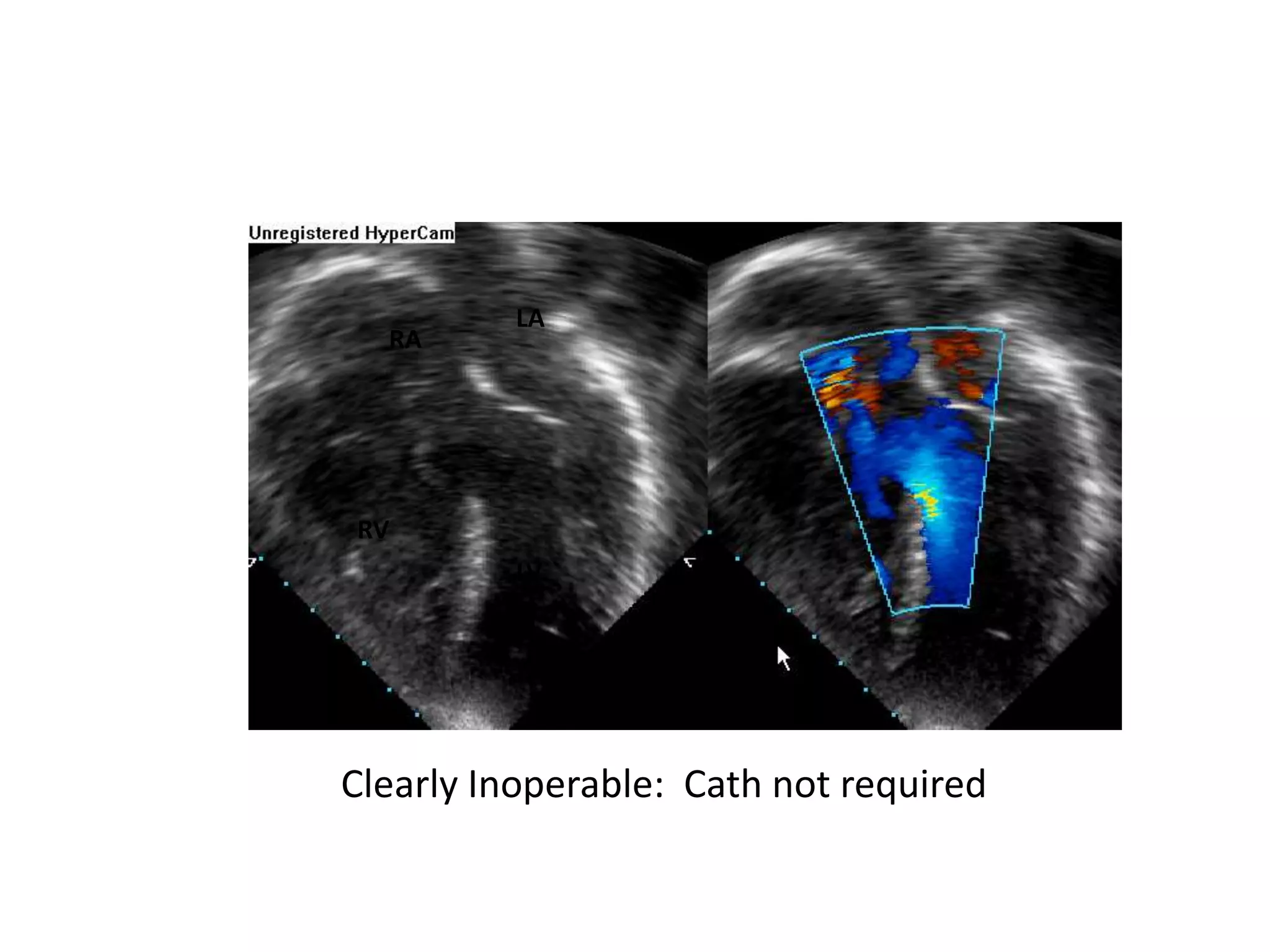
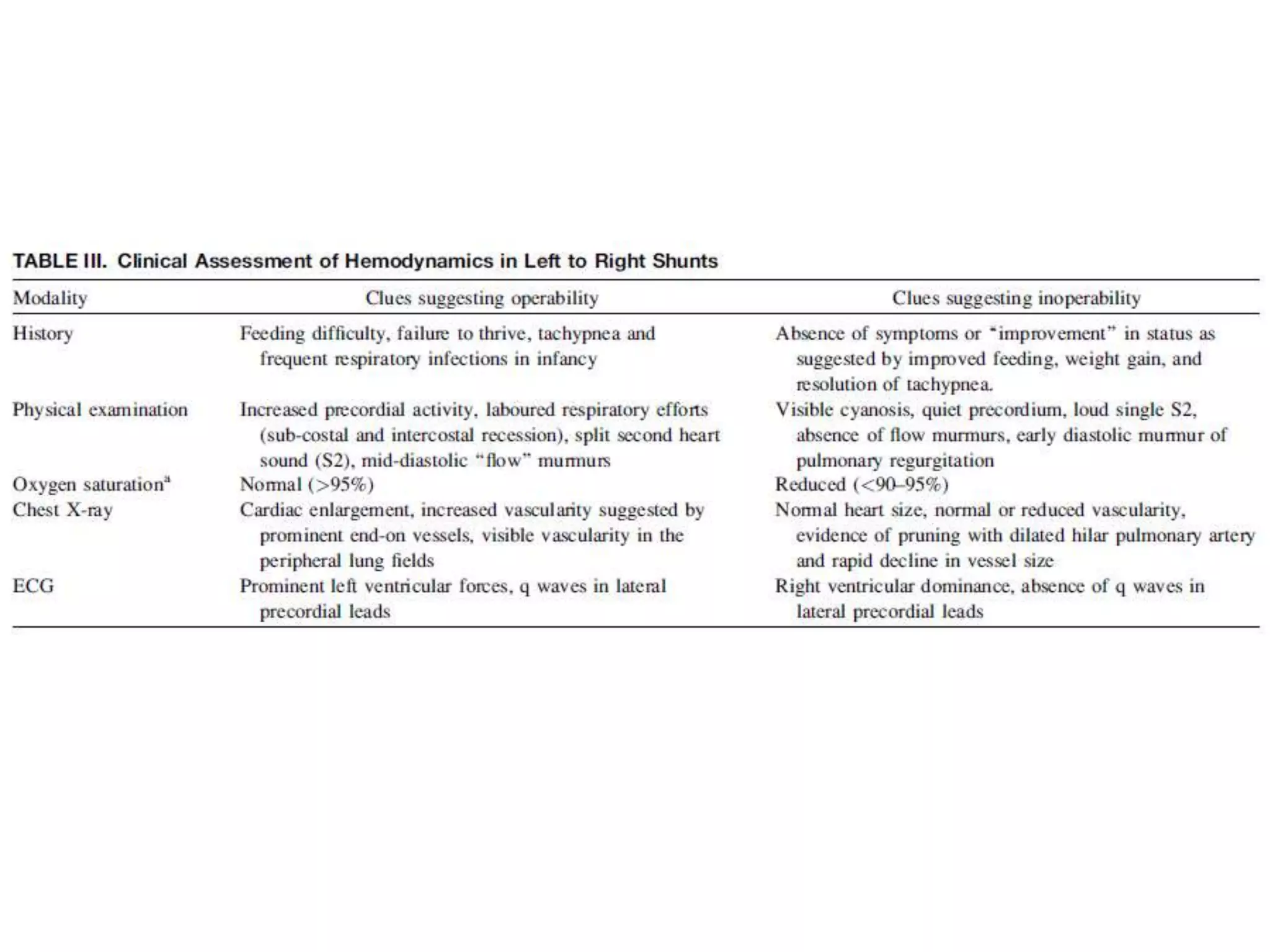
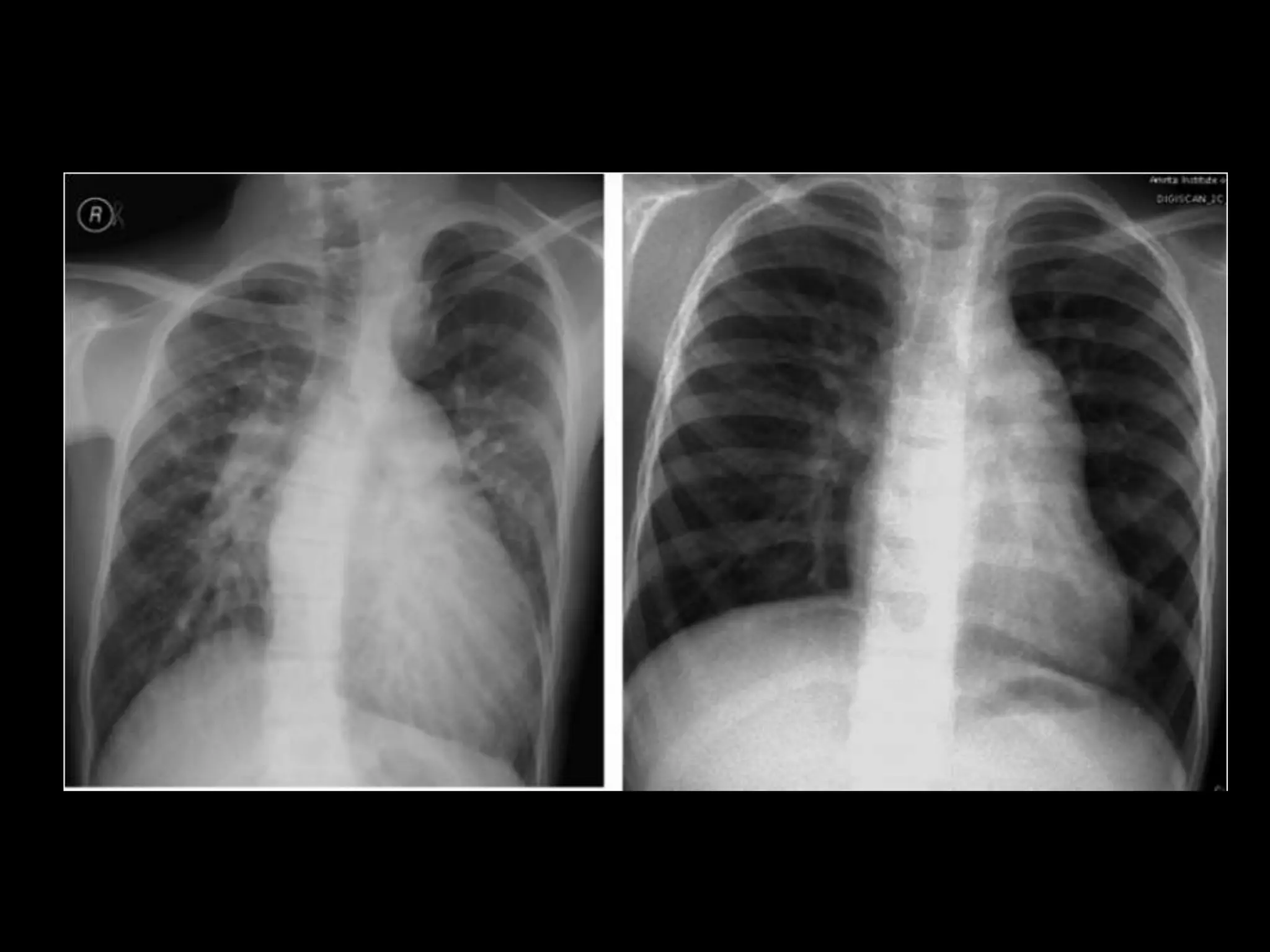
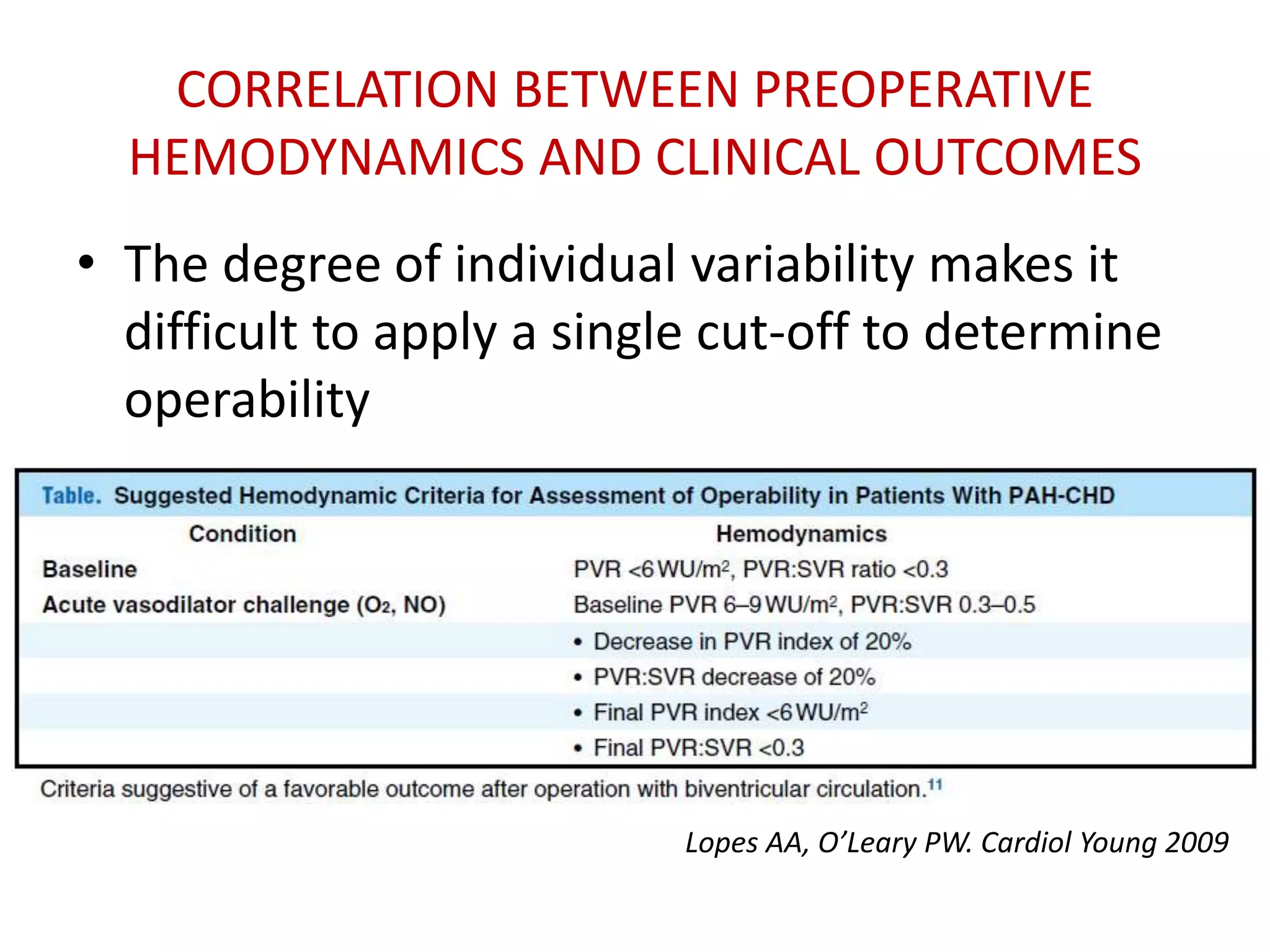
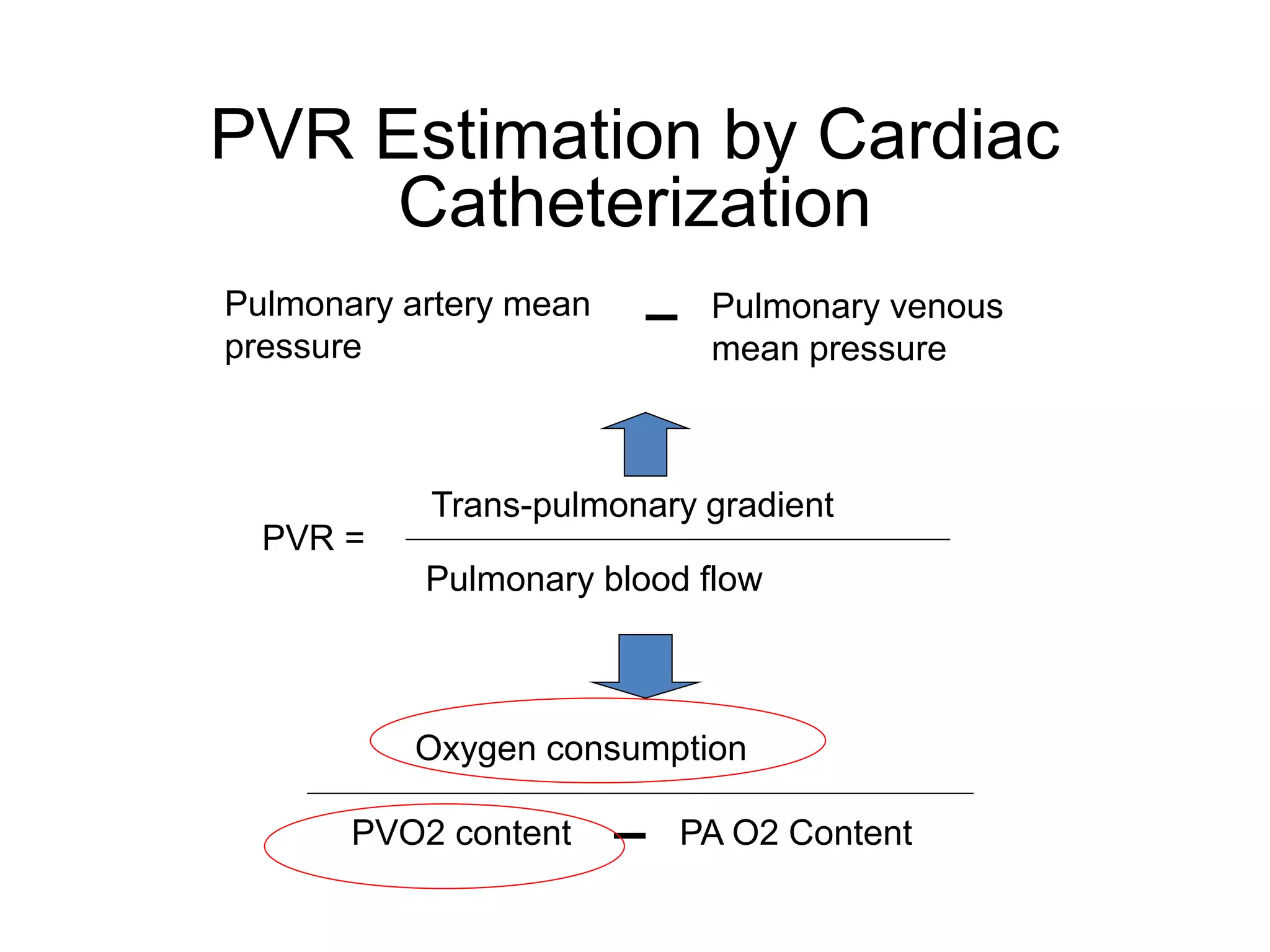
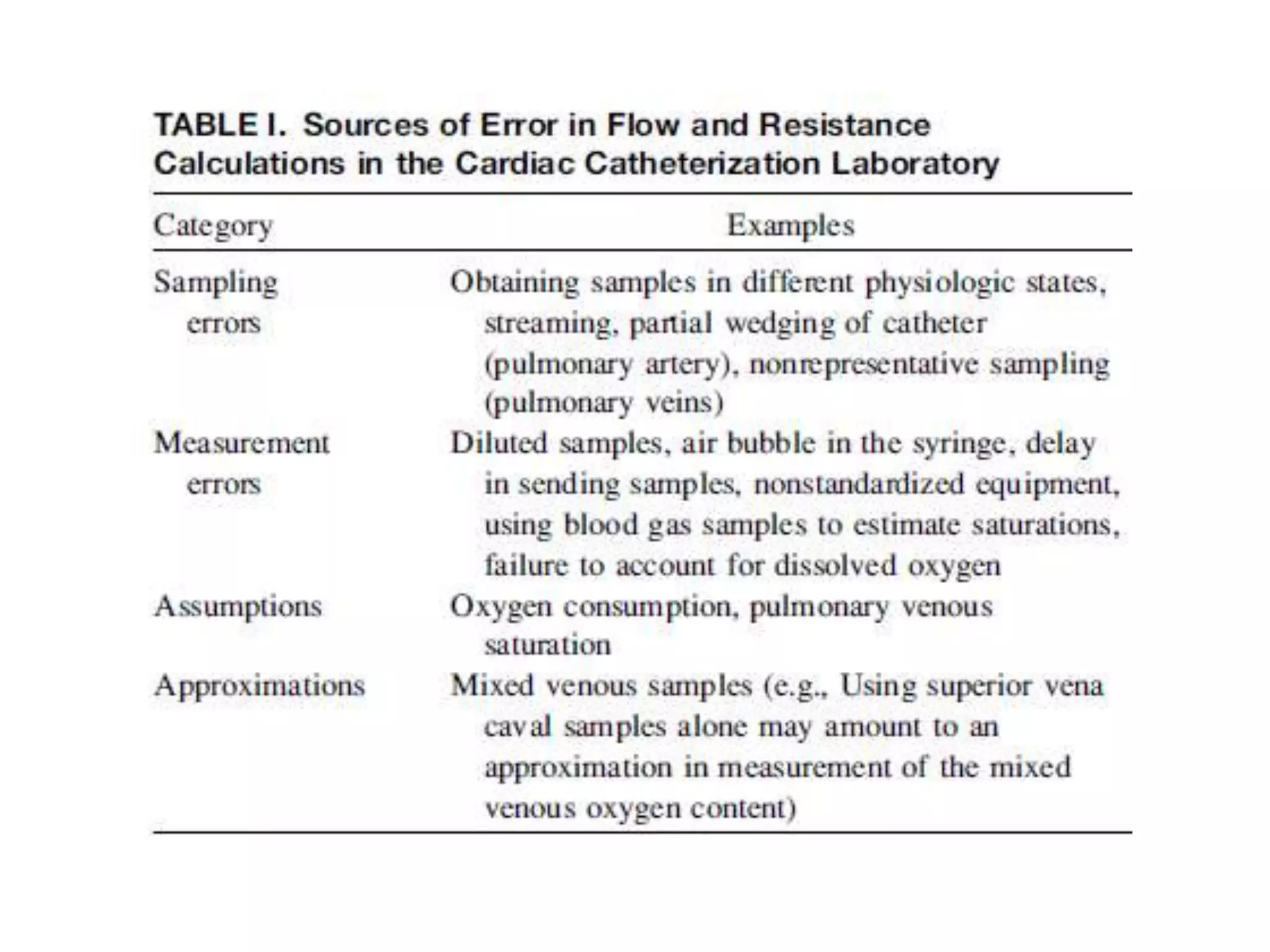
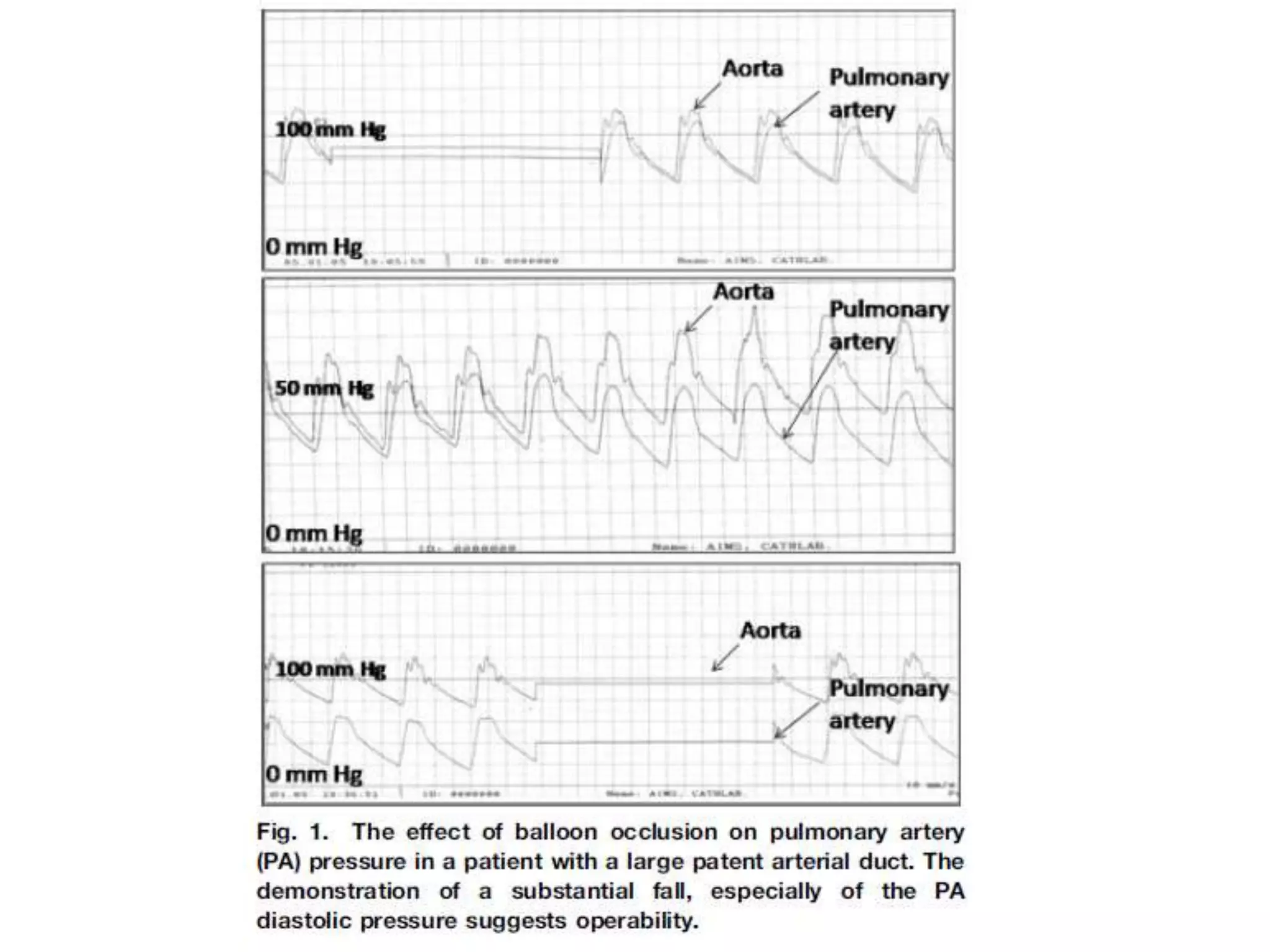
The document assesses the operability of left to right shunts and the implications of pulmonary arterial hypertension (PAH) associated with congenital heart disease (CHD). It outlines the challenges in determining operability and emphasizes the importance of comprehensive clinical evaluation, including various diagnostic tools like echocardiography and cardiac catheterization. Additionally, it highlights the need for clear guidelines and further studies to better assess individual patient outcomes and risks associated with surgery.