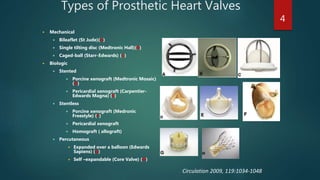
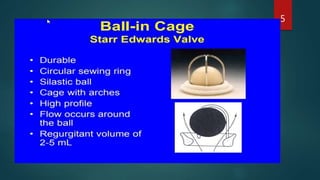
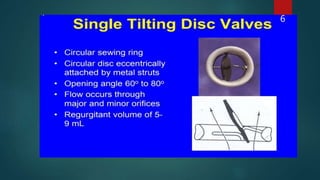
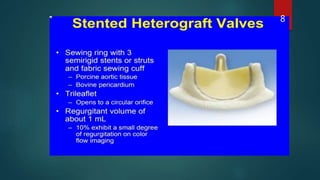
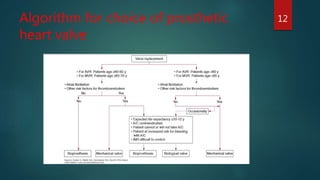
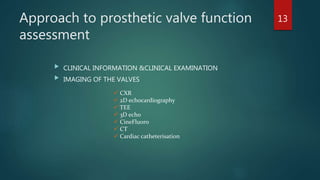
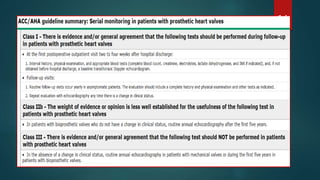
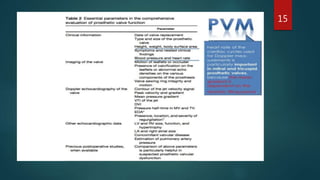
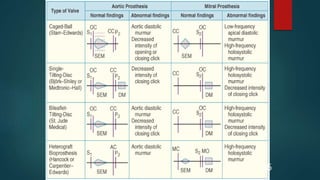
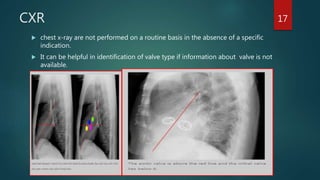
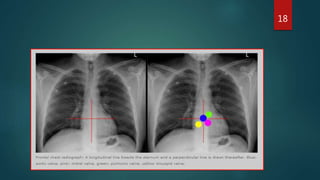
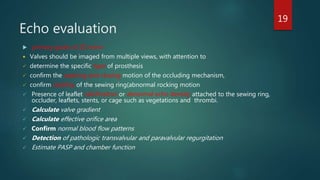
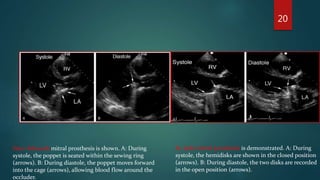
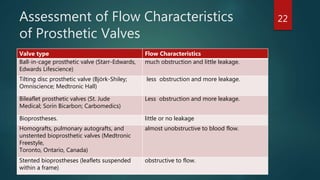
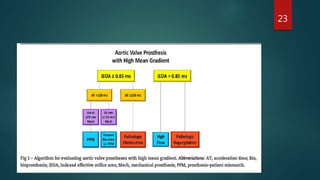
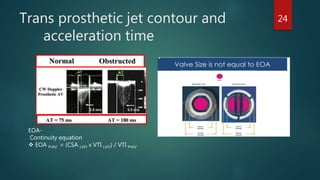
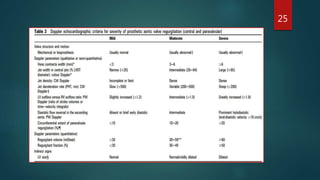
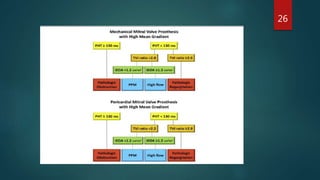
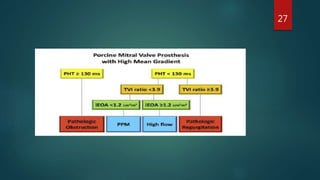
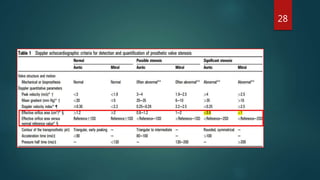
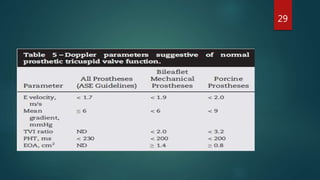
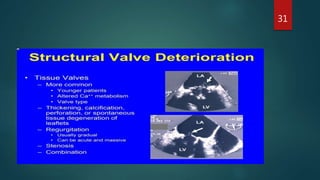
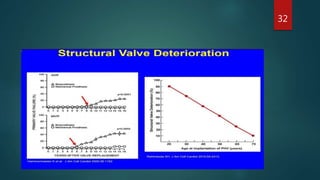
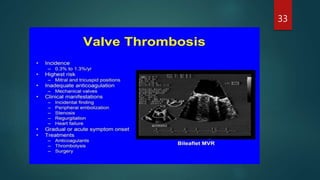
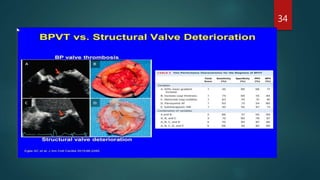
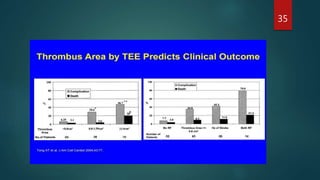
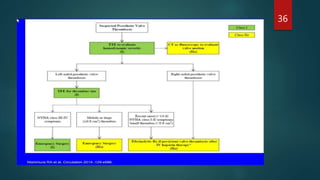
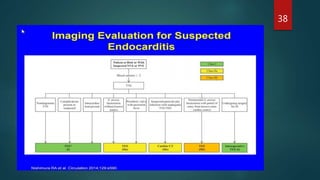
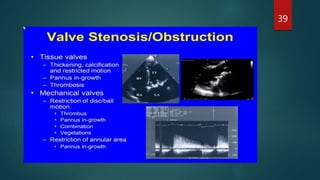
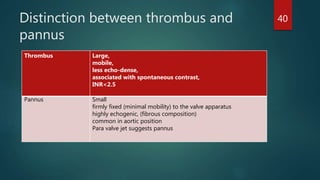
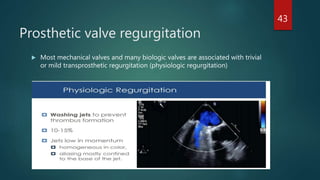
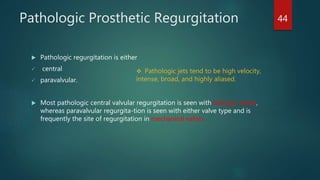
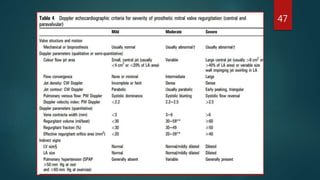
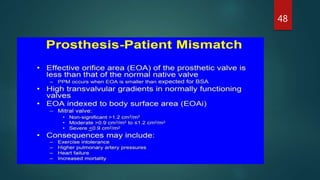
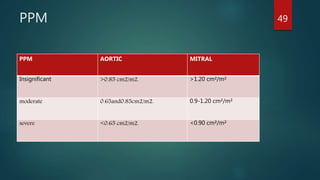
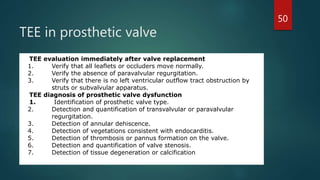
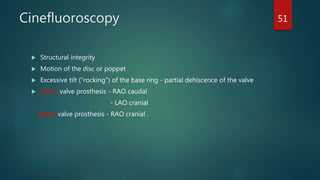
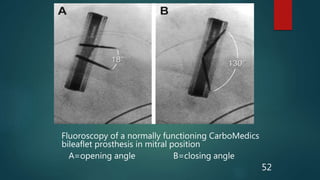
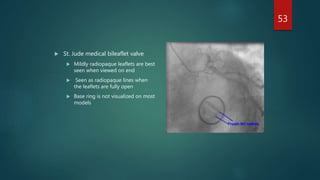
This document reviews prosthetic heart valves, detailing their evolution since the 1960s and classifying them into mechanical and biological types, each with distinct characteristics and failure rates. It discusses the benefits, complications, and assessment methods for these valves, emphasizing the need for anticoagulation in mechanical valves and the challenges of degeneration in biological valves. Key imaging methods for valve evaluation are also outlined, along with descriptions of prosthetic valve dysfunction and the implications of patient-prosthesis mismatch.