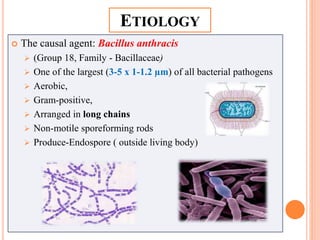
1. Anthrax is caused by the bacterium Bacillus anthracis. It forms spores that can survive for decades in the soil and infect humans and animals.
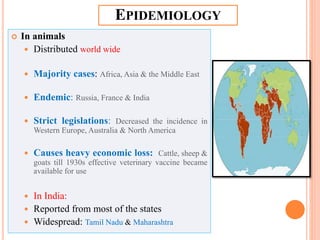
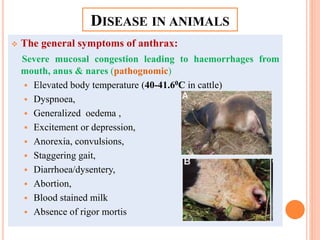
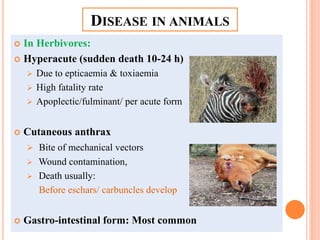
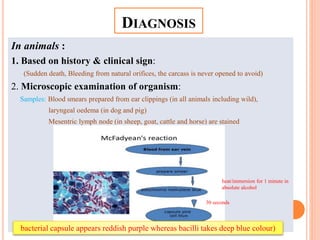
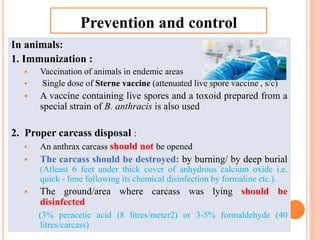
2. In animals, anthrax causes sudden death and bleeding from body openings. It is still endemic in some parts of the world. Vaccination and proper disposal of carcasses is important for control.
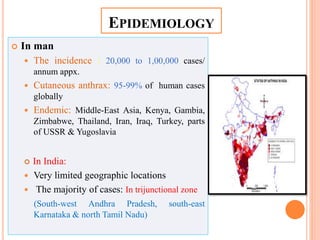
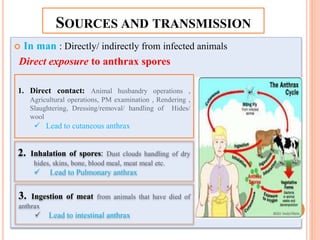
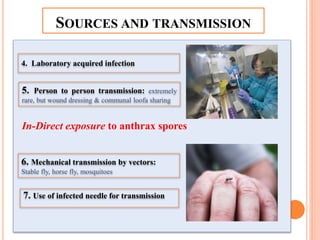
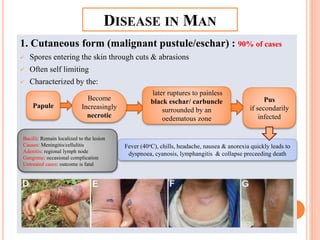
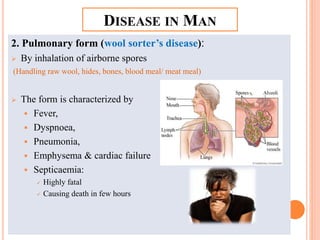
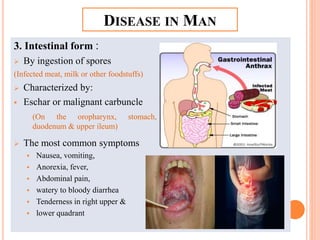
3. In humans, anthrax infection can cause skin lesions, lung infection, or intestinal illness depending on the route of exposure. Occupations working with infected animals or animal products are at highest risk.