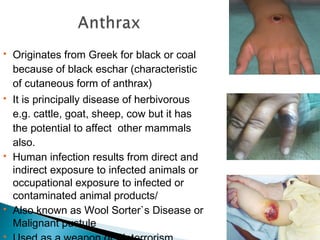
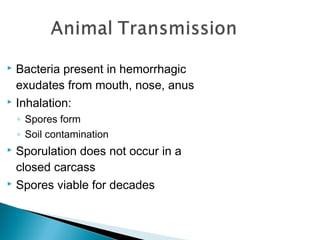
Anthrax is a potentially lethal disease caused by Bacillus anthracis bacteria. It can affect both humans and animals through contact with infected animals, animal products, or inhalation of spores. There are four types of anthrax disease in humans - cutaneous, inhalation, gastrointestinal, and meningeal. While anthrax infections can be deadly, prompt antibiotic treatment and vaccination can effectively treat and prevent the disease.