This document provides information about anthrax, including:
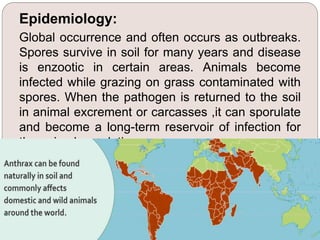
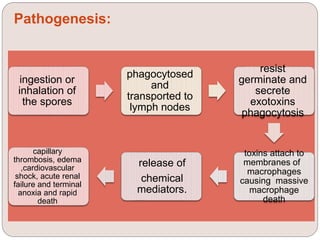
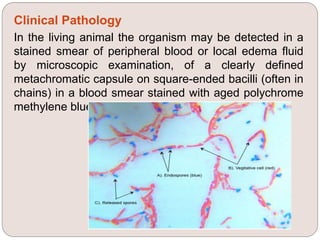
- It is caused by Bacillus anthracis, a spore-forming bacterium. Spores can survive in soil for years.
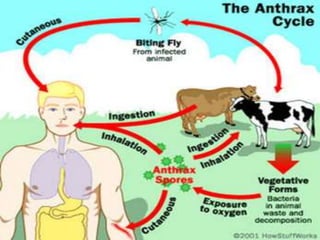
- Animals can be infected by ingesting spores from contaminated soil, food, or water. Humans can be infected through contact with infected animals or inhaling spores.
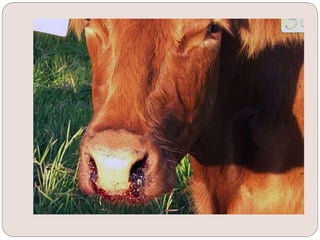
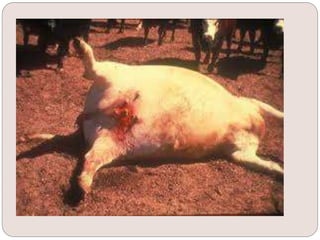
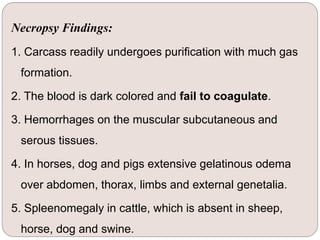
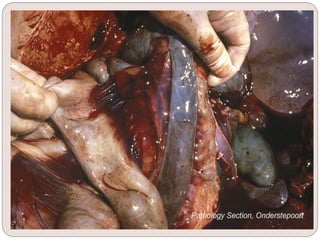
- Symptoms in animals include fever, respiratory distress, and edema. Untreated, it causes rapid death. Diagnosis is made by identifying B. anthracis in blood or fluid smears. Treatment involves antibiotics but anthrax serum is also used.
- Control involves quarantining infected farms, destroying contaminated materials, and