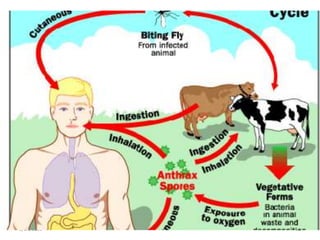
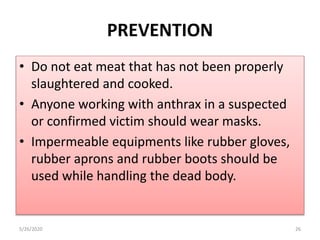
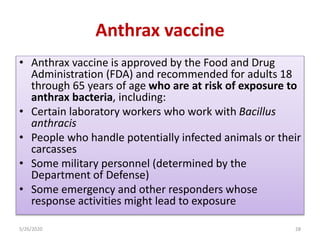
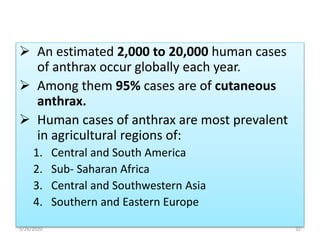
Anthrax is a serious infectious disease primarily affecting herbivores and is caused by the bacterium Bacillus anthracis. Humans can become accidental hosts through direct or indirect contact with infected animals or contaminated products, leading to various forms such as cutaneous, gastrointestinal, and inhalational anthrax. Prevention includes vaccination of at-risk populations and proper handling of infected materials, while treatment typically involves antibiotics like penicillin.