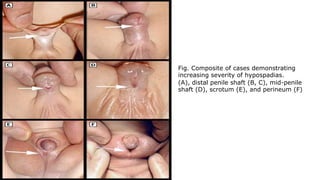
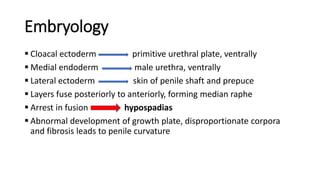
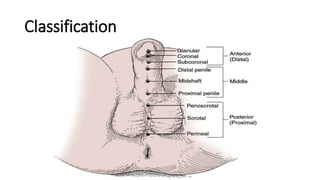
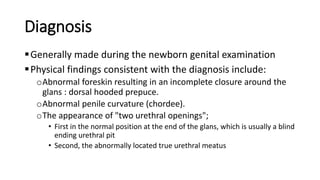
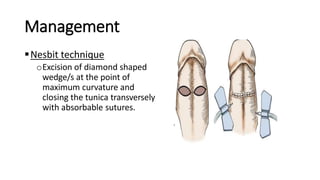
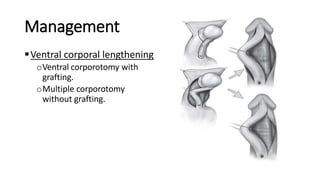
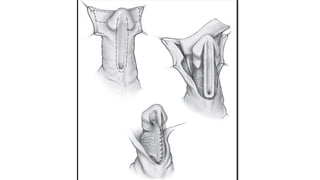
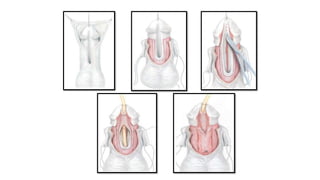
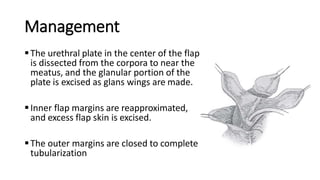
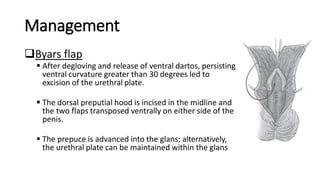
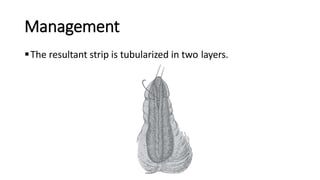
This document provides information on hypospadias, including its definition, embryology, classification, diagnosis, and management. It describes hypospadias as an abnormal ventral placement of the urethral opening in males, often accompanied by penile curvature and a dorsal hooded foreskin. The etiology is multifactorial involving genetic and environmental factors disrupting androgen stimulation in development. Surgical management aims to correct penile curvature, reconstruct the urethra, and provide skin coverage using techniques such as tubularized incised plate repair and preputial flaps depending on the location and severity of hypospadias.