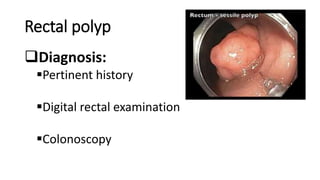
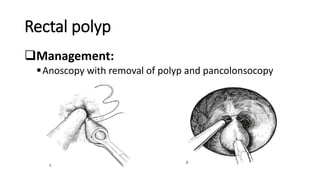
This document discusses rectal and umbilical polyps. For rectal polyps, it notes they occur most often in preschool children, are usually solitary, and can cause bleeding. It describes their appearance and causes, including obstruction of colonic glands. Diagnosis involves history, exam, and colonoscopy. Treatment is removal during colonoscopy.
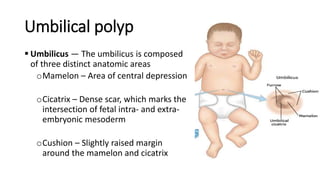
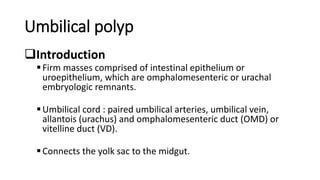
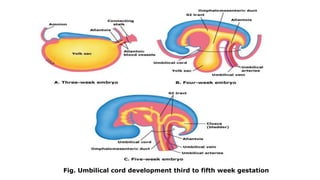
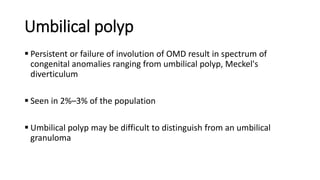
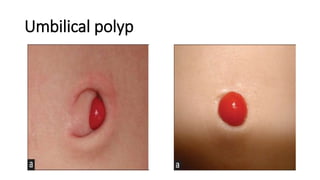
For umbilical polyps, it explains they are remnants of embryonic structures that normally dissolve. They present as masses or discharge from the umbilicus. Histology shows enteric or colonic mucosa. Treatment is surgical excision of the polyp, which is usually adequate without further inspection.