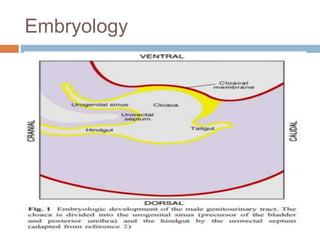
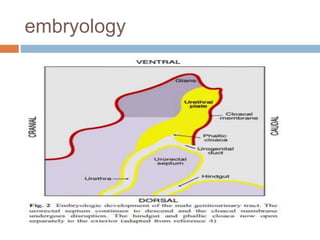
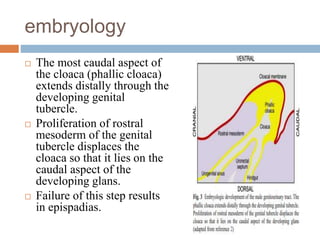
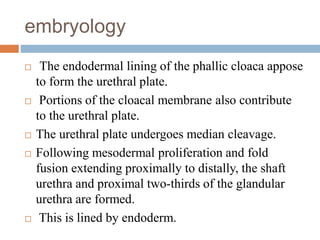
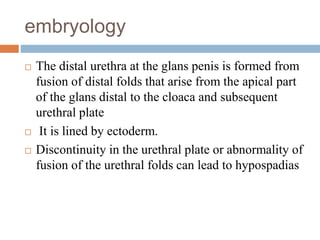
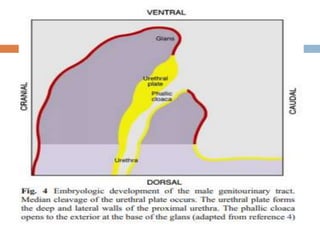
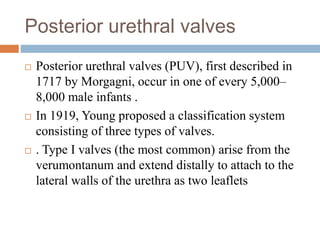
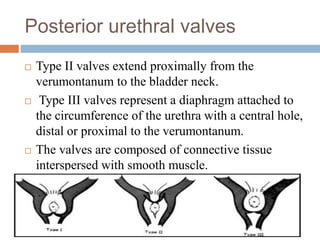
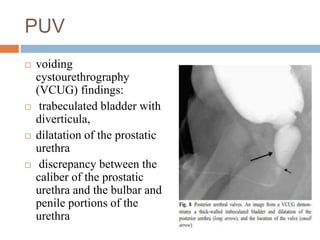
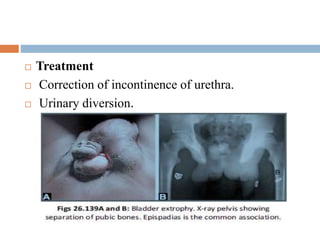
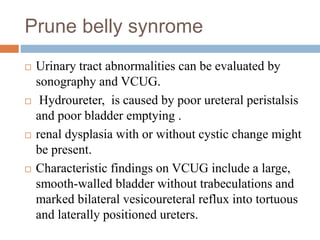
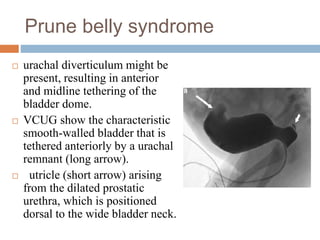
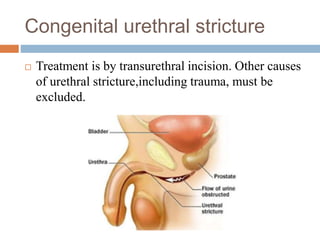
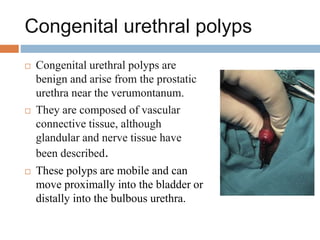
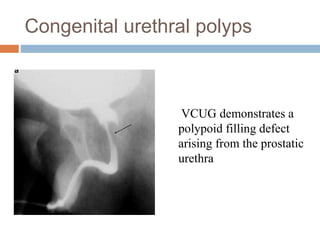
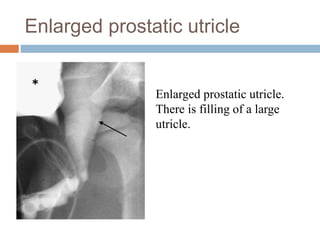
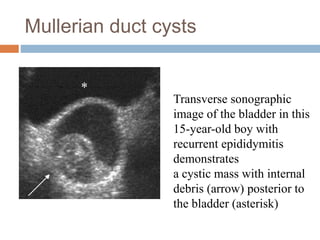
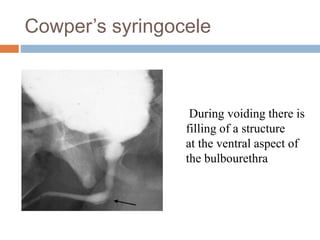
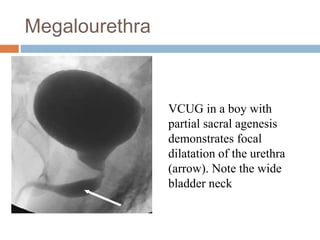
This document discusses the embryology and various congenital anomalies of the male urethra. It begins with the embryological development of the male urethra from the cloaca. It then describes several congenital anomalies in more detail, including posterior urethral valves, hypospadias, epispadias, prune belly syndrome, congenital urethral strictures, congenital urethral polyps, enlarged prostatic utricles, Mullerian duct cysts, and Cowper's syringocele. For each anomaly, it discusses features, diagnosis using imaging like VCUG, and potential treatments.