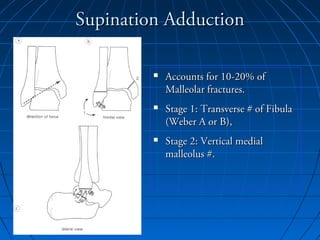
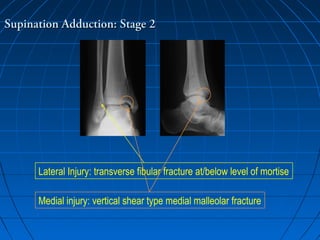
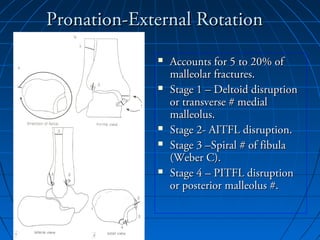
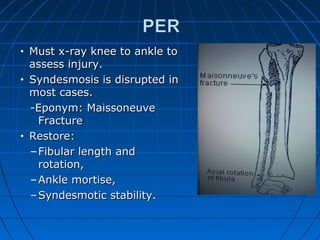
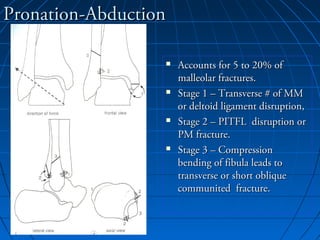
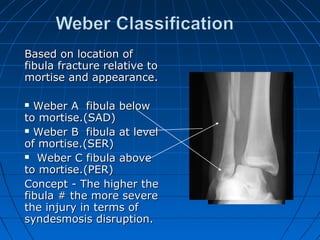
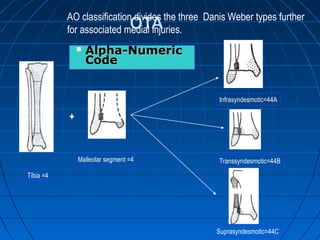
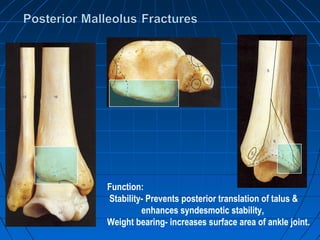
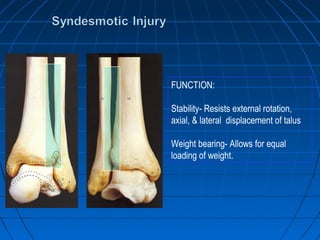
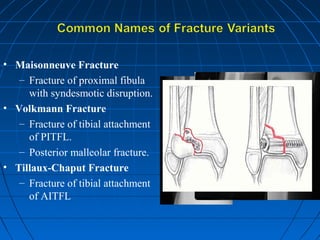
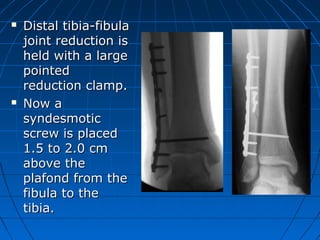
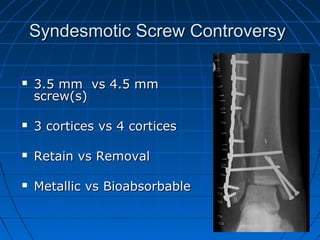
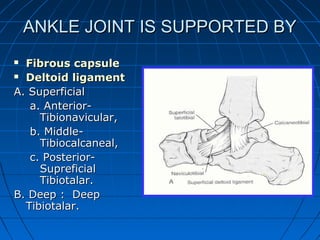
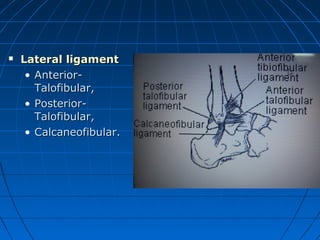
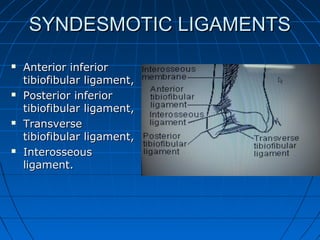
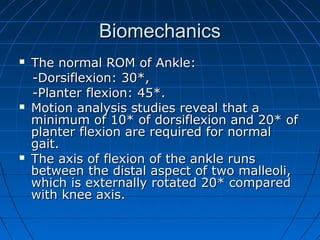
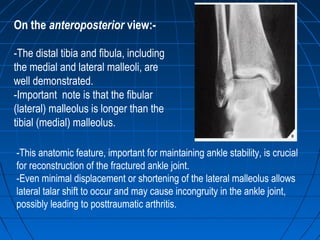
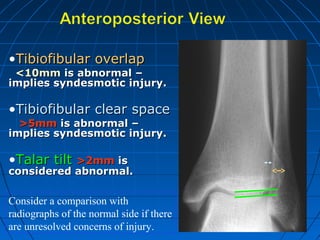
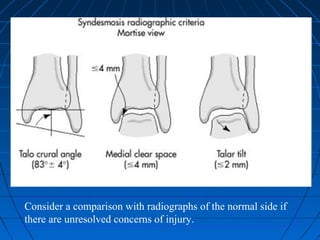
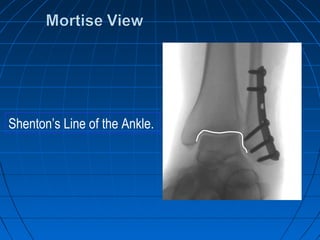
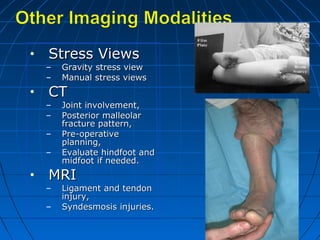
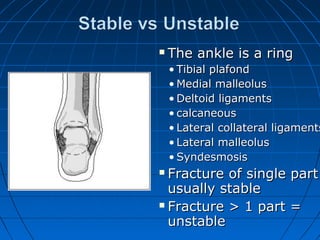
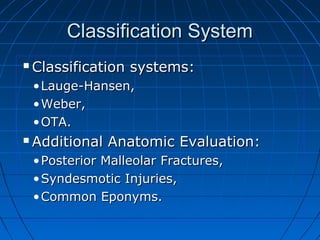
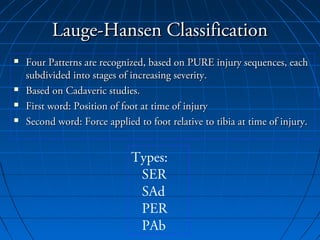
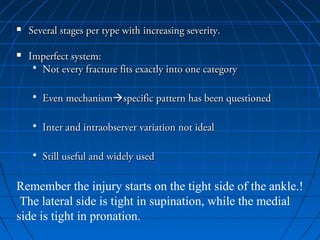
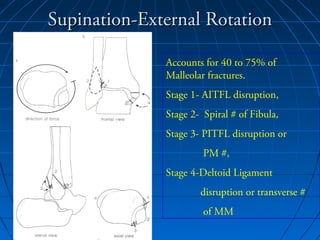
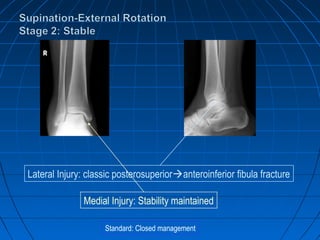
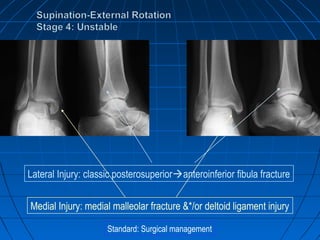
Ankle fractures are common injuries that require careful evaluation to identify bony and soft tissue damage. The ankle is a complex hinge joint supported by ligaments and the tibia, fibula, talus, and deltoid ligament. Classification systems like Lauge-Hansen and Weber are used to characterize fracture patterns and guide treatment, which may involve closed management or surgery to restore ankle anatomy and stability. Restoring length and rotation of the fibula as well as stabilizing potential syndesmotic injuries is important for successful outcomes.
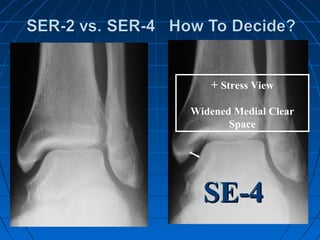
![GOAL: TO EVALUATE DEEP DELTOID [i.e. INSTABILITY]
METHOD: MEDIAL TENDERNESS
MEDIAL SWELLING
MEDIAL ECCHYMOSIS
STRESS VIEWS- GRAVITY OR MANUAL](https://image.slidesharecdn.com/anklefractures-160907184233/85/Ankle-fractures-29-320.jpg)