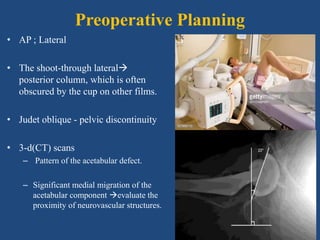
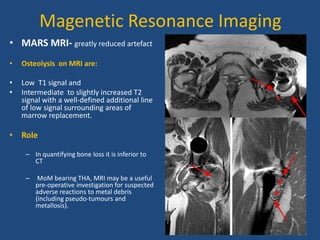
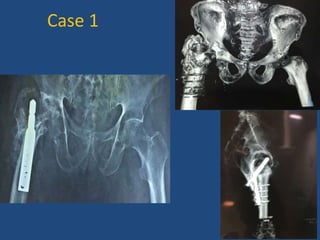
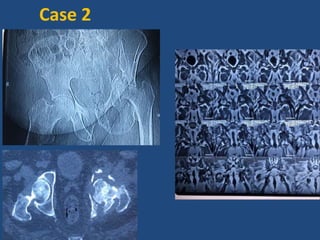
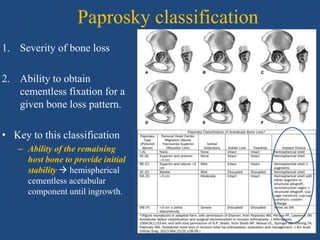
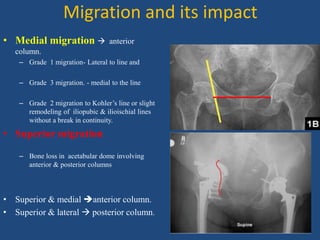
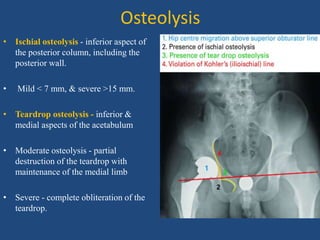
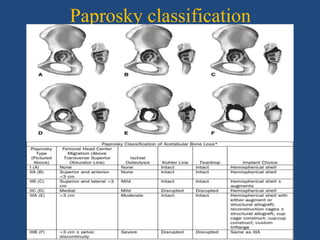
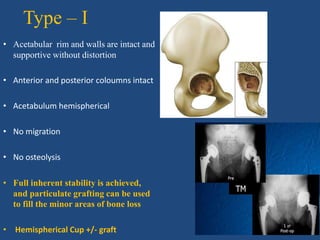
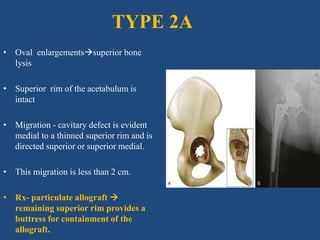
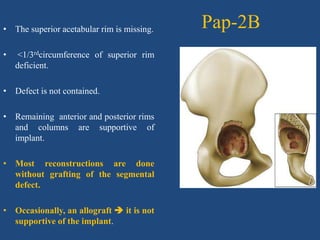
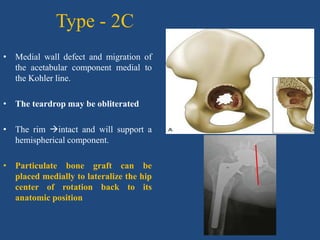
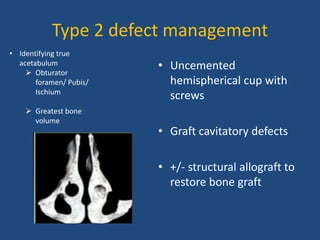
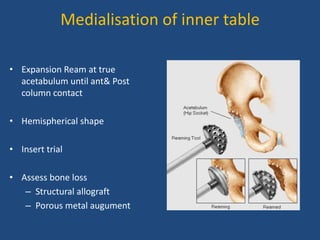
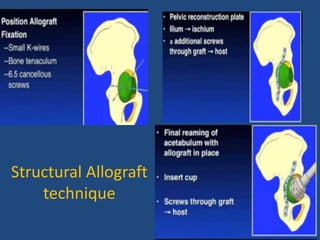
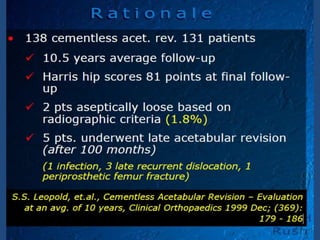
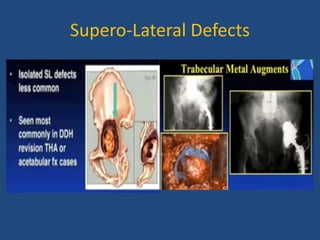
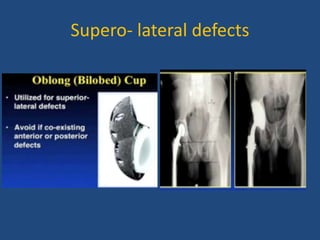
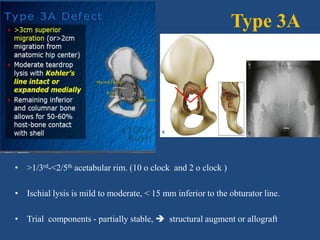
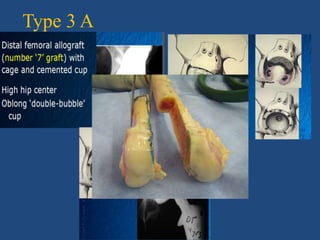
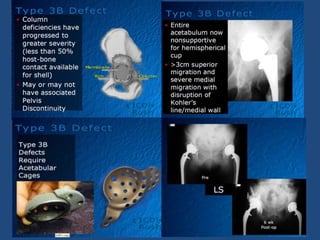
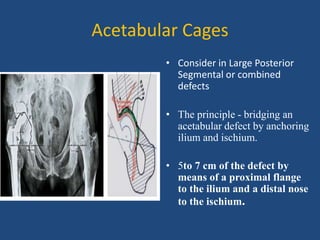
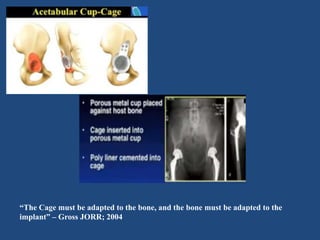
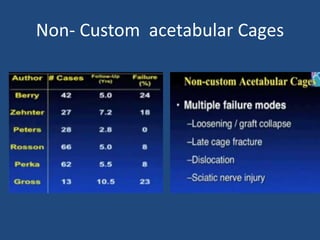
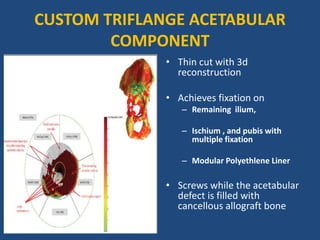
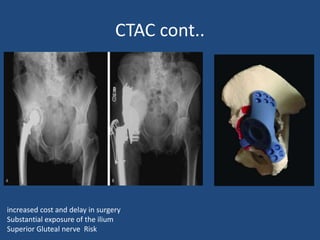
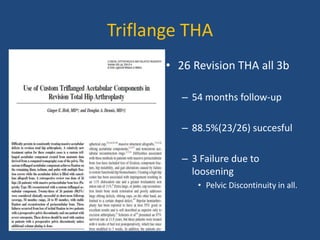
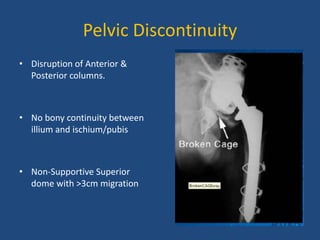
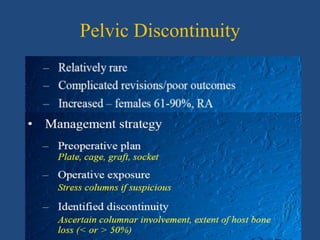
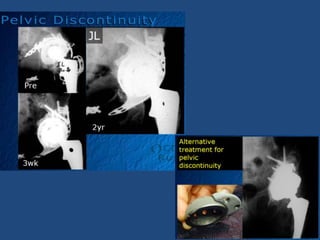
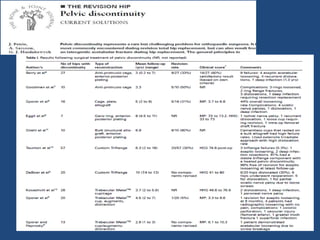
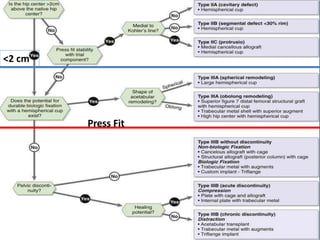
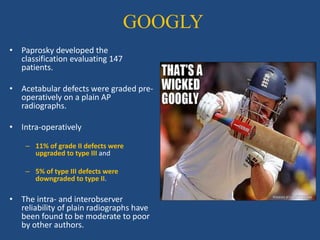
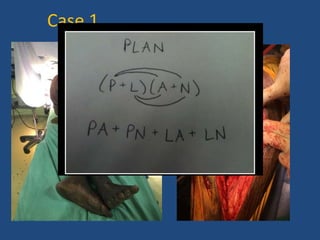
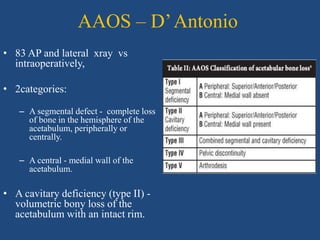
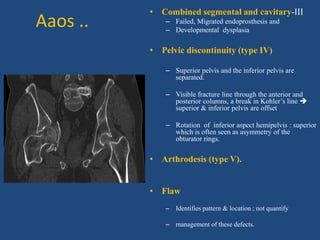
This document discusses acetabular defects and their reconstruction. It begins by describing common causes of acetabular deficiency like dysplasia, trauma, and loosening. Surgical goals are to restore hip mechanics, re-establish bone coverage of the acetabular component, and achieve rigid fixation. Preoperative planning involves imaging like x-rays and CT scans to evaluate the pattern and severity of bone loss. The Paprosky classification grades acetabular defects based on the amount of bone loss and ability to achieve cementless fixation. Different reconstruction techniques are described depending on the defect type, including various cup designs, bone grafting, and structural allografts.